Encephalopathy!!!
advertisement

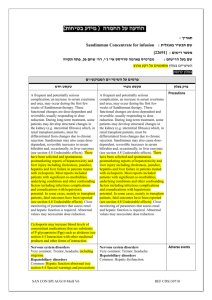
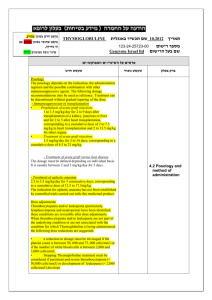
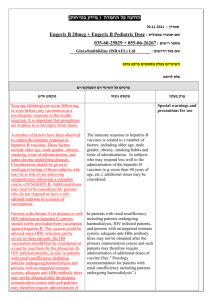
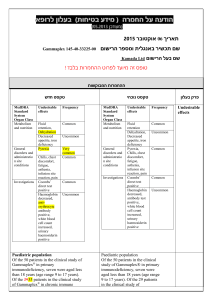
Acute Liver Failure - ALF Yaakov Maor M.D. Department of Gastroenterology and Hepatology Sheba Medical Center, Tel-Hashomer פרשת מקרה בן ,51יליד ישראל • מנכ"ל חברה נימצא 6חודשים בהודו • 3שבועות הרגשה רעה ,חוסר תיאבון ,בחילות • לפני שבועיים שתן כהה ובהמשך צהבת • מיומיים "שינוי בהתנהגות" וישנוניות • הוטס לארץ ישירות לחדר מיון פרשת מקרה בבדיקה: • ישנוני אך ניתן להערה • דופק 100לדקה ,ל"ד ,100/60חום 37.3c • צהבת בולטת בלחמיות ובעור • רעד מסוג Flapping Tremor • ללא סימני מחלת כבד כרונית • בטן רכה ,הכבד נמוש בקצהו ,הטחול אינו מוגדל פרשת מקרה :בבדיקות מעבדה Bilirubin-15 mg/dL • ALT-1800 IU/L; AST-1200 IU/L; ALP-220 IU/L • Glucose-80 mg/dL; Creatinine-1.2 mg/dl • INR-2.9 • Hb-12.8 g/dL; WBC-4,300; PLT-133,000 • pH-7.43; Lactate-21 mg/dL • Ammonia-90 µg/dL • Acute Liver Failure • Definition – Accurate diagnosis of the syndrome • Etiology – Determine prognosis and specific treatment • Initial resuscitation and treatment of complications • Timely transfer to a Transplant Center!!! Definition • Rapid development of hepatocellular dysfunction – Coagulopathy (INR 1.5), Jaundice • Encephalopathy!!! • Absence of a prior history of liver disease (Wilson’s disease, autoimmune hepatitis) Definition • Interval between the onset of illness and ALF <26 weeks (US ALF Study Group) • Jaundice-to-encephalopathy interval (Prognosis): - Hyperacute liver failure – Within 7 days - Acute liver failure – 7 – 21 days - Subacute liver failure – 21 days – 26 weeks Etiology • Viral infection – HAV, HBV (HDV), HCV?, HEV • Acetaminophen – Predictable, Direct (ETOH) • Idiosyncratic Hepatotoxicity – Halothane, Anti-TB • Idiopathic (15-44%) – Occult viral infection? • Rare: Autoimmune hepatitis, Wilson’s disease, Budd-Chiari syndrome, Pregnancy related, Toxins - Amanita Phalloides, Cancer Etiology 160 Tx. Free survival 140 Transplanted Transplant-Free Survival Rate 120 Died Before Tx. 100 80 68% 63% 60 50% 17% 50% 50% 40 Transplant-free survival – 11% (0-25%) 12% 20 25% 0% 13% AC AP Dr ug s HB V HA V Sh oc k AIH Wi lso Pr n eg na B.C ncy .S yn d Ca nc er Ind Ot he ete r rm ina nt 0 11% 0% Unfavorable • Idiopathic • Drugs (not ACPA) • HBV (acute on chronic) • Wilson • Etiology-Specific Therapies • Acetaminophen - N-Acetylcysteine • Hepatitis B – Lamivudine • Pregnancy-associated – Urgent delivery • Budd-Chiari syndrome - Angioplasty • Amanita Phalloides - Penicillin, Silibinin פרשת מקרה • לחולה נימצאו נוגדניםAnti HAV IgM : • אובחנה הפטיטיס Aחריפה! Natural History of ALF: Acute Liver Failure Acute Hepatitis Acute Liver Dysfunction SIRS DEATH החייאה וניהול ראשוני – ביחידה לטיפול נמרץ • ניטור מצב הכרה וסימנים חיוניים • החייאת נוזלים ומעקב תפוקת שתן • מעקב ומתן גלוקוז -היפוגליקמיה • אנזימי כבד • מעקב בדיקות דם כולל: • בילירובין • גלוקוז • קראטינין ואלקטרוליטים • ,INRפקטור V • לקטט • גאזים • אמוניה עורקית • ס .ד Encephalopathy – Precipitating Factors Non-neurological: • Sepsis and SIRS! • Hypoglycemia • Hypoxemia • Renal failure Neurological: • Occult seizures - 33% stage 3 – 4 encephalopathy • Cerebral edema Stages of Encephalopathy • Stage 1 – Affect, insomnia, concentration • Stage 2 - Drowsiness, disorientation, confusion, Agitation! Asterixis appears • Stage 3 - Marked somnolence and incoherence • Stage 4 - Coma Encephalopathy - Management • Quient enviroment! • Maintain the patient's head at a 30° to improve jugular venous outflow • Sedative-hypnotic drugs should be avoided – Clinical monitoring – Use Propofol!!! • Treat reversible conditions e.g., hypoglycemia • Patients encephalopathy stage 3 – 4 – intubation: - airway protection - Intra Cranial Pressure – ICP Encephalopathy - Management • Brain CT - Mass, intracranial hemorrhage, and evidence of brainstem herniation • Correlation between CT evidence of cerebral edema ande ICP is imperfect • Monitor and treat deeply sedated patients with phenytoin for sub-clinical seizure? ICP Monitoring • Most accurate way to detect intracranial hypertension • Should be limited to specialized units and to patients awaiting LTS with stage 3 – 4 encephalopathy • Has not been shown to increase survival • Aims: - ICP <20-25 mm Hg - Cerebral perfusion pressure (CPP) = Mean Arterial Pressure (MAP) – Intra Cranial Pressure (ICP) >50-60 mm Hg ICP Monitoring • Requires correction of underlying coagulopathy – Prognostic factor • Portal of entry for infectious organisms • Can precipitate intracranial hemorrhage • Trans-cranial Doppler has not been validated for ICP monitoring Treatment of ICP • Osmotherapy Mannitol – IV bolus of 0.5 to 1 g/kg 20% solution – May be repeated until plasma osmolarity reaches 320m Osm/L • Therapy with mannitol requires preserved renal function (or hemofiltration) • Hypertonic NaCl 30% – Maintain serum Na+ levels of 145-155 mEq/L Treatment of ICP • Hyperventilation - Cerebral vasoconstriction - CBF • New therapies: - N-Acetylcysteine (In non-acetaminophen ALF) Recently: Patients with early encephalopathy showed higher spontaneous survival rate - Mild hypothermia (32C - 34c) ICP via CBF • Not in use !!! - Lactulose – No proven benefit - Barbiturate Coagulopathy • Avoid plasma/PLT administration: - Index of hepatic function - Volume overload • Indications: - Bleeding - Invasive procedures - Prophylactic: PLT count <20,000; INR >7 • aFVII may be advantageous Coagulopathy • Monitor INR q 6-12 h (Obtain Factor V when INR> 2.5) Day INR 2# 3 3# 4 4# 5 Transfer to transplant Center Infections • Develop in 80% of patients • Accounts for 25% of patients who are excluded from liver transplantation • Clinical recognition of infection is difficult: SIRS may occur without infection • Infection may be without fever/leukocytosis in 30% • High level of suspicion for infection should be maintained with a low threshold for administration of antibiotics!!! Management - General • ICU admission and supportive treatment • Timely transfer to a Transplantation Center • Liver transplantation – The Only Established & Definitive Treatment Predictors of Prognosis Patients with ALF fall into two categories: • Intensive medical care enables recovery of hepatic function – Allow time for regeneration!!! • Require liver transplantation to survive Predictors of Prognosis Determinant of prognosis: • Regeneration • Liver dysfunction • Encephalopathy and Brain edema • Multi-Organ Failure – MOF Predictors of Prognosis Avoid the following two scenarios: • Death of the patient despite intensive medical care without consideration of transplantation • Unnecessary liver transplantation when recovery would have occurred spontaneously – Surgical mortality, lifelong immunosuppression Liver Transplantation • Clinical decision making aided by prognostic markers • Before the era of liver transplantation – <50% survival • Liver transplantation for ALF – 63% - >70% (Lower than other etiologies) King’s College Hospital Criteria ALF secondary to acetaminophen overdose: • pH <7.30 (irrespective of encephalopathy grade) or • Hepatic encephalopathy grade III-IV • INR >6.5 • Creatinine >3.4 mg/dL • Arterial Lactate >27 mg/dL King’s College Hospital Criteria ALF with other causes: • INR >6.5 (irrespective of encephalopathy grade) or any three of the following (irrespective of encephalopathy grade) • • • • • Age <10 or >40 years Non-A, non-B hepatitis or drug-induced origin Duration of jaundice before encephalopathy >7 days Bilirubin >17.6 mg/dL INR >3.5 Clichy Criteria Stage III-IV encephalopathy associated with: • Factor V level <20% in patients <30 years • Factor V level <30% of normal in patients >30 years (Based on cohort of patients with acute hepatitis B) Predictors of Prognosis • Model for End-Stage Liver Disease (MELD) Score – (Bilirubin; INR; Creatinine) • Elevated Alpha-Fetoprotein (Indicator of regeneration) • APACHE II Liver Transplantation • Contraindications to transplantation: - Irreversible brain damage (CPP <40 mm Hg) - Active extra-hepatic infection - Multiple-organ failure syndrome – MOF • Consider living-related liver transplantation פרשת מקרה • הוחל טיפול ב 6 N-Acetylcysteine -מ"ג לק"ג לשעה אבל... • • • • מצב הכרה – ישנוני יותר – שלב אנצפלופתי III-II הונשם ומקבל Propofol INRעלה ל ;6 -פקטור 15% -V קראטינין עלה ל1.9 mg/dl - העברה למרכז השתלות Intensive care Etiology – specific Rx. Consultation with LTS center Contraindication for LTS Yes No Transfer to LTS center – National status one Re-assess for recovery or contraindication for LTS No Liver Transplantation • קשר טלפוני ראשוני Yes Continue intensive support Ongoing intensive care :• העברה כאשר II • אנצפלופתיה דרגה , לקטטמיה,• חמצת • היפוגליקמיה • קואגולופתיה מטפסת פרשת מקרה • נוצר קשר עם מרכז השתלות בבלגיה • הועבר בהטסה להמתנה להשתלת כבד Experimental Therapy • Provide a bridge to liver transplantation/ Spontaneous regeneration and recovery • Auxiliary liver transplantation • Extracorporeal liver support devices: - Hemodiadsorption systems - Bioartificial liver devices • Nonhuman liver transplantation • Hepatocyte transplantation