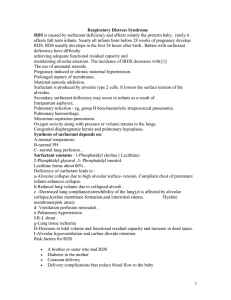
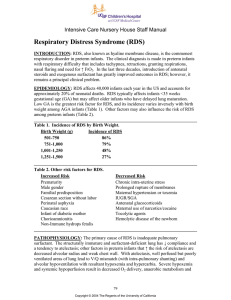
Respiratory Distress Syndrome
advertisement

Respiratory Distress Syndrome Resident Lecture Series Soo Hyun Kwon, MD Neonatal-Perinatal Fellow Overview • • • • • • • • • Definition Epidemiology Lung Development Pathophysiology Risk Factors Clinical Manifestations DDx Diagnosis Treatment Objectives • Define respiratory distress syndrome (RDS). • Discuss the epidemiology, pathophysiology, and diagnosis of RDS. • List a differential diagnosis for respiratory distress in the neonate. • Describe the treatments for RDS. • Discuss ventilation strategies that can be used in the infant who has RDS. • Describe long-term complications of RDS and its treatments. Definition • Formerly known as hyaline membrane disease • Deficiency of pulmonary surfactant in an immature lung • Disease of prematurity Epidemiology • Major cause of morbidity and mortality in preterm infants • 20,000-30,000 newborn infants each year • Incidence and severity of RDS are related inversely to gestational age of newborn infant • 26-28 weeks' gestation : 50% • 30-31 weeks' gestation : <30% • Overall incidence in 501-1500 grams: 42% • • • • 501-750 grams: 71% 751-1000 grams: 54% 1001-1250 grams: 36% 1251-1500 grams: 22% Phases of Lung Development Lung Development Surfactant • Complex lipoprotein • Composed of 6 phospholipids and 4 apoproteins • 70-80% phospholipids, 8-10% protein, and 10% neutral lipids Surfactant Metabolism Assessment of Fetal Lung Maturity • Lecithin/sphingomyelin (L/S) ratio • Lamellar body counts • Phosphatidylglycerol • After 35 weeks gestation L/S Ratio Pathophysiology Etiology • Preterm delivery • Mutations in genes encoding surfactant proteins • SP-B • SP-C • ATP-binding cassette (ABC) transporter A3 (ABCA3) Lung Compliance Normal Lung Hyaline Membranes Risk Factors • • • • Prematurity Maternal diabetes C-section delivery Asphyxia Surfactant Inactivation • Meconium and blood can inactivate surfactant activity (Full-term > Preterm) • Proteinaceous edema and inflammatory products increase conversion rate of surfactant into its inactive vesicular form • Oxidant and mechanical stress associated with mechanical ventilation that uses large TV Clinical Manifestations • • • • Tachypnea Nasal flaring Grunting Intercostal, subxiphoid, and subcostal retractions • Cyanosis Differential Diagnosis • • • • • • • • TTN MAS Pneumonia Cyanotic Congenital Heart Disease Pneumomediastinum, pneumothorax Hypoglycemia Metabolic problems Hematologic problems • Anemia, polycythemia • Congenital anomalies of the lungs Diagnosis • Onset of progressive respiratory failure shortly after birth • Characteristic chest radiograph • ABG • Hypoxia • Hypercarbia CXR Prevention • Antenatal glucocorticoids • Enhances maturational changes in lung architecture and inducing enzymes • Stimulate phospholipid synthesis and release of surfactant • All pregnant mothers at risk for preterm delivery at or below 34 weeks gestation should receive ACS Treatment • Surfactant Therapy • Assisted Ventilation Techniques • Supportive Care • Thermoregulation • Fluid Management • Nutrition References • • • • Jobe AH. Why Surfactant Works for Respiratory Distress Syndrome. NeoReviews. 2006; 7: 95-106. Pramanik AK, et al. Respiratory distress syndrome. http://emedicine.medscape.com/article/976034-overview. Saker F, Martin R. Pathophysiology and clinical manifestations of respiratory distress syndrome in the newborn. Uptodate. http://www.utdol.com Warren JB, Andersen JM. Respiratory distress syndrome. Neoreviews. 2009; 7: 351-361. Questions or Comments?