Respiratory Distress Syndrome RDS
advertisement

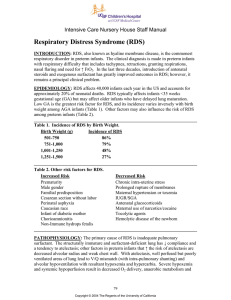
Respiratory Distress Syndrome RDS is caused by surfactant deficiency and affects mainly the preterm baby, rarely it affects full term infants. Nearly all infants born before 28 weeks of pregnancy develop RDS. RDS usually develops in the first 24 hours after birth.. Babies with surfactant deficiency have difficulty achieving adequate functional residual capacity and maintaining alveolar aireation. The incidence of IRDS decreases with:[1] The use of antenatal steroids. Pregnancy-induced or chronic maternal hypertension. Prolonged rupture of membranes. Maternal narcotic addiction. Surfactant is produced by alveolar type 2 cells. It lowers the surface tension of the alveolus. Secondary surfactant deficiency may occur in infants as a result of Intrapartum asphyxia. Pulmonary infection - eg, group B beta-haemolytic streptococcal pneumonia. Pulmonary haemorrhage. Meconium aspiration pneumonia. Oxygen toxicity along with pressure or volume trauma to the lungs. Congenital diaphragmatic hernia and pulmonary hypoplasia. Synthesis of surfactant depends on: A-normal temperature. B-normal PH C- normal lung perfusion. . Surfactant contains : 1-Phosphatidyl choline ( Lecithine) 2-Phosphtidyl glycerol .3- Phosphatidyl inositol. Lecithine forms about 60% . Deficiency of surfactant leads to : a-Alveolar collapse due to high alveolar surface- tension. Compliant chest of premature infants enhances collapse. b-Reduced lung volume due to collapsed alveoli . c –Decreased lung compliance(stretchibility of the lung),it is affected by alveolar collapse,hyaline membrane formation,and interstitial edema. Hyaline membrane(pink areas) d- Ventilation perfusion mismatch . e-Pulmonary hypertension f-R-L shunt . g-Lung tissue ischemia H-Decrease in tidal volume and functional residual capacity and increase in dead space. I-Alveolar hypoventilation and carbon dioxide retention Risk factors for RDS A brother or sister who had RDS Diabetes in the mother Cesarean delivery Delivery complications that reduce blood flow to the baby 1 Multiple pregnancy (twins or more) Rapid labor The risk decreases if the mother had hypertension or prolonged rupture of membranes CXR :Typical X-ray findings appear at 6-12 hours. 1-Ground glass appearance due to microatelactasis which is due to small alveolar radius and weak chest wall. 2-Air bronchogram . 3-In severe cases there is complete white out of the lung fields. Clinical features : Clinical features appear immediatly after birth or within 4 hours.The disease worsens for 48-72 hours.Recovery coincides with diuresis after a period of oliguria. resolution begins between 2 and 4 days. 1-Tachypnea,respiratory rate more than 60/minute . 2-Grunting:is a short low pitched sound heard during expiration when the infant expires with a partially closed glottis. It can conserve lung volume, keep the alveoli opened, it typically indicates, a paranchymal disease and a poor lung compliance . 3-Sternal, intercostals, sub costal retractions . 4- Cyanosis in room air. 5-Hypotonia. 6- Edema. 7- Hypothermia 8-Oliguria, diuresis is a sign of improvement. 9- Mixed respiratory and metabolic acidosis. The clinical diagnosis of RDS is made in preterm infants with respiratory difficulty that includes tachypnea,retractions,grunting,nasal flaring and need for high oxygen. Prevention of RDS: a-Good antenatal care. b-Good selection and timing of caesarian section. c-Betamethasone administration to mothers suspected to get preterm delivery at 24-34 weeks.This drug is superior to dexamethasone which is associated with high incidence of periventricular leukomalacia. Antenatal steroids significantly reduce mortality/It should be given 24-48 hours before delivery and not more than 7 days.It decreases the incidence of intraventricular haemorrhage and NEC. When a fetus must be delivered between 24 wk and 34 wk, giving the mother 2 doses of betamethasone 12 mg IM 24 h apart or 4 doses of dexamethasone 6 mg IV or IM q 12 h at least 48 h before delivery induces fetal surfactant production and reduces the risk of RDS or decreases its severity. The effect of treatment is optimal if the baby is delivered more than 24 hours and less than seven days after commencement of treatment. 2 d-Surfactant replacement, given as prophylaxis or rescue treatment, reduces the incidence and severity of respiratory distress syndrome, air leaks, and mortality in preterm infants with surfactant deficiency,It also decreases the incidence of IVH .Necrotizing enterocolitis, nosocomial infections, patent ductus arteriosus, intraventricular hemorrhage, and chronic lung disease, appears primarily unaffected Neither beneficial nor adverse effects of surfactant use on growth and/or neurodevelopmental parameters. Recommendations (1) Mothers at high risk of preterm birth should be transferred to p er i nat a l c ent re s w it h e x p er ienc e i n ma na gement of R DS (C). (2) Clinicians should offer a single course of antenatal steroids to all women at risk of preterm delivery from about 23 weeks up to 35 completed weeks• gestation (A). (3) Antibiotics should be given to mothers with preterm prelabour rupture of the membranes as this reduces the risk of preterm delivery (A). (4) A second course of antenatal steroids should be considered if the risk from RDS is felt to outweigh the uncertainty about possible long-term adverse effects (D). Treatment:The baby should be admitted to the Neonatal Intensive Care Unit(NICU). For babies with RDS to have best outcomes, it is essential that they have optimal supportive care, including maintenance of a normal body temperature, proper fluid management, good nutritional support, management of the ductus arteriosus and support of the circulation to maintain adequate tissue perfusion. Surfactant secretion generally increases during labour, therefore elective caesarean section of low-risk fetuses before 39 weeks• gestation should not be performed, as some of them may develop RDS or other respiratory disorders A treatment strategy of early (within 20 to 30 min after birth) surfactant therapy is associated with significant decrease in duration of mechanical ventilation, lesser incidence of air leak syndromes, and lower incidence of bronchopulmonary dysplasia. 1- surfactant :There are two types of surfactants: A-natural from bovine or porcine source which is prefered B-Synthetic. Complications of surfactant include: blockage of endotracheal tube transient hypoxia,hypotension,pulmonary hemorrhage. surfactant supplementation prior to the first breath is feasible and is of value as a protection against the respiratory distress syndrome Dose 3-4 ml/kg for 2 doses 12 hours apart Recoomedations for use of surfactant 1. Surfactant replacement therapy should be directed by physicians qualified and trained in its use and administration 3 2. Nursing and respiratory therapy personnel experienced in the management of low birth weight infants, including mechanical ventilation, should be available 3. Equipment should be available. 4-It should be used in specialized centers. Complications of surfactant 1-Obstruction of endotracheal tube. 2-Increase O2 requirements. 3-Pulmonary haemorrhage(rare). 2-Maintain temp . Body temperature should be maintained at 36.5– 37.5°C at all times 3-Correct hypoxia:supplemental oxygen should be maintained between 85 and 93% and not exceed 95% 4-Correct acid – base abnormalities . 5-Nutrition ,Fluid should be given on the first day as 10% dextrose 65-75mls/kg/24 hours, later electrolyte fluid is added.. Full nutrition requirements for glucose, amino acids and lipids can be safely commenced on the first day of life and progressively increased to 3.5 g/kg/day of amino acids and 2.5–3.0 g/ kg/day lipids 6–18 g/kg/day. Dextrose 10% solution at 100 ml/kg . 20 ml/kg/day of breast milk, should be provided 6-Antibiotics .Because it is difficult to differentiate RDS from sepsis especially group B streptococci antibiotics are given and a combination of penicillin or ampicillin and gentamicin are used. It is considered good practice to screen all babies with RDS by performing blood cultures as well as looking for other evidence of sepsis such as neutropenia or an elevated C-reactive protein and initiating antibiotic therapy whilst awaiting results. Prophylactic fluconazole and nystatin can reduce invasive fungal infection rates, fluconazole 3 mg/kg body weight twice weekly for 6 weeks. 7-Inhaled nitrous oxide. Inhaled nitric oxide improves gas exchange, decreases pulmonary vascular lability, and reduces pulmonary inflammation the incidence of chronic lung disease and death has been decreased by INO. 8-Assisted ventilation: 9-Inositol administration: Inositol influences cellular function and organ maturation.The administration of inositol to premature infants with respiratory distress syndrome who are receiving parenteral nutrition during the first week of life is associated with increased survival without bronchopulmonary dysplasia and with a decreased incidence of retinopathy of prematurity. The trend now is to use Nasal IPPV or Nasal CPAP instead of Invasive IPPV. 9-Inositol administration: Inositol influences cellular function and organ maturation.The administration of inositol to premature infants with respiratory distress syndrome who are receiving parenteral nutrition during the first week of life is associated with increased survival without bronchopulmonary dysplasia and with a decreased incidence of retinopathy of prematurity. 4 11-Caffeine should be part of routine care for very preterm babies with RDS to facilitate extubation Sudden deterioration of RDS on spontaneous breathing. 1-Pneumothorax . 2-Periventricular hemorrhage . 3-Infection . 4 –Aspiration. 5-Apnea . Complications of RDS : 1-Air leak . 2-PDA . 3-Periventricular hemorrhage . 4-BPD(Bronchopulmonary Dysplasia) . 5-Pneumonia . 6-Complications of mechanical ventilation . 7-Neurological complications . 8-Retinopathy of prematurity . Dr Sabih S AL-FETLAWI MRCP(UK) FRCP(Edin) MRCPCH(UK) 5