EN8Oza
advertisement
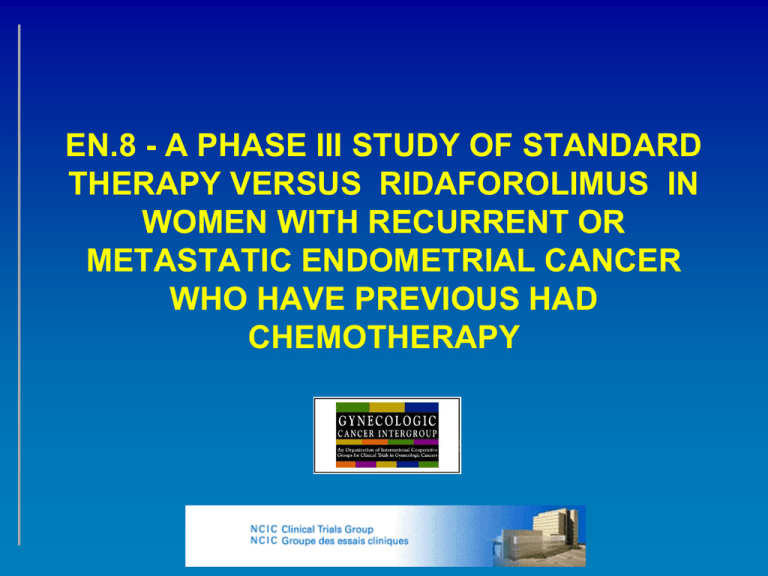
EN.8 - A PHASE III STUDY OF STANDARD THERAPY VERSUS RIDAFOROLIMUS IN WOMEN WITH RECURRENT OR METASTATIC ENDOMETRIAL CANCER WHO HAVE PREVIOUS HAD CHEMOTHERAPY Proposed Design Change • Accrual to the phase 2 studies has been slower than expected. • Reasons: start up for centres, increasing use of prior chemotherapy in preference to hormonal agent. • Consider allowing either hormonal OR chemotherapy as the control arm for this study. Schema R A Women with N recurrent or D metastatic O endometrial M cancer I 1-2 Prior Z Chemotherapy E Arm 1: ridaforolimus 40 mg po days 1-5 each week Imaging Disease Survival q8 progression follow-up weeks Arm 2: medroxy progesterone 200 mg or megestrol 160 mg (as per local practice) po daily Chemotherapy options Sample size: Approximately 460 patients Eligibility • • • • • Metastatic or recurrent endometrial cancer, not curable by other means Patient with endometrial carcinoma for whom a hormonal therapy or chemotherapy would be considered an acceptable treatment option. At least one prior chemotherapy and up to two prior chemotherapy regimens (chemotherapy may have been administered in the adjuvant OR for metastatic disease settings). Measurable or non-measurable disease (per RECIST) site of disease ECOG Performance status 0-2 mTOR in Endometrial Ca temsirolimus everolimus ROUTE DOSE 1st LINE ACTIVITY 2nd LINE ACTIVITY IV 25 mg Q wk ~25% RR 7% RR (100/mo) (60% SD) (2/27) 10 mg QD ND 0% RR PO (56/mo*) ridaforolimus IV 12.5 QDx5 Q2 wk CBR 40% ND (130/mo) 9% RR (4/45) CBR 30% ridaforolimu s PO 40 QDx5 Q wk 206I NCIC 205 RP2 (160/mo*) RR endpoint PFS endpoint NCIC CTG IND.192 Phase II Trial Update • Patients enrolled = 13 • 8 on study, 4 off study • 1 confirmed PR to date • (no prior chemo patient) • Toxicity: ALT, Diarrhea, Granulocytopenia, Mucositis/Stomatitis (grade 1, 2) Dose Intensity (n = 9 patients) Planned Actual Cycles (N) Dose Units/week Receiving Median Median > 90% of (Range) Intensity (Range) Planned DI 112.5 ridaforolimus 2 (1-6) 200 mg (56.8-200) 11.1 Agent Stratification • Patients will be stratified by: – Cooperative group – Performance status – Prior chemotherapy – Hormone receptor (ER/PR) status – Tumour grade – Proposed treatment (chemo versus hormones) Endpoints • Primary Endpoint: – Overall survival • Secondary Endpoints: – Response rates – Duration of response – Time to progression – Toxicity – Quality of Life – Economic Analysis • Correlative Studies: – To explore potential prognostic and predictive factors in correlative studies of archival endometrial tissue. Statistics • The primary endpoint of the study is overall survival. • We assume that the median overall survival for patients with prior chemotherapy treated with hormones is 8 months and the hazard ratio of ridaforolimus to hormones will be 0.75 (an improvement of 2.7 months in median survival); a two-sided alpha 0.05; and 80% power, then 380 deaths will be required. • Sample Size and Duration of Study • Accrual rate duration of follow-up sample size total duration • 150 per year 12 months 450 4.0 years • 200 per year 12 months 460 3.3 years Translational Research • Formalin-fixed paraffin embedded blocks and one plasma blood sample will be obtained from patients entered into EN.8 phase 3 trials. • These samples will be analyzed for genetic abnormalities likely to correlate with benefit/resistance to mTOR inhibitor. The genetic profile will be determined through translational research studies undertaken concurrent with the proposed phase 3 trials. • The studies will evaluate the following: – – – One hundred snap frozen endometrial carcinoma specimens with associated blood samples will be obtained from the Ontario Tumour Bank. DNA will be extracted and assessed for amplifications and deletions. 100 samples will identify genetic events occurring at > 3%. DNA from formalin fixed paraffin embedded samples obtained from NCIC CTG phase 2 studies of mTOR inhibitors will be extracted and analyzed for deletions and amplifcations identified from study 1. DNA results will be correlated with clinical outcomes of patients entered into the phase 2 trials to determine the genetic abnormalities that correlate with patient outcome. The genetic profile will be tested on tumour samples and germline DNA obtained from patients enrolled on EN.8 study. Status • Company and NCIC CTG phase II trials underway – Accrual slower than expected; both protocols amended to allow 1 prior chemotherapy – Company trial – RP2 - amended to allow chemotherapy OR hormonal agent in control arm – Projected completion of accrual April 2010 and analysis around ASCO • Potential to look at accrual rate and efficacy patients versus hormone or dealers choice control • Concept updated for potential international group collaborators • First draft of protocol completed – internal review prior to distribution to company and collaborators Questions • Design acceptable? • Chemotherapy Control Options? – Proposed: • Platinums – carboplatin, cisplatin • Taxanes – paclitaxel, docetaxel • Doxorubin or doxil • Single agent or combination • Groups that are interested? • Expected accrual?