Chemo and endocrine
advertisement

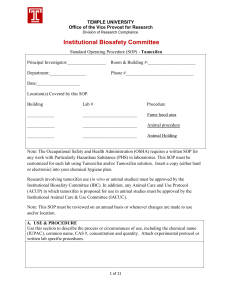
When all you have is a hammer… Endocrine therapy Chemotherapy Targeted therapies Radiotherapy 1 Hormonal treatment of Breast Cancer Time Line 1990’s Demonstration of the therapeutic efficacy of Tamoxifen 1970’s Development of Tamoxifen 1870 1980’s 1st description of surgical oophorectomy ER/PR detection and resurgence in interest in endocrine Rx Endocrine pathways in cancer Estrogen and Progesterone receptors Several authors demonstrated the relationship of the cytosolic form ER to the efficacy of endocrine therapy. The nuclear translocation and subsequent transcription are dependent on several corepressors and activators. The SRC co activator action is particularly important in this regard. Recently ER-β has been identified. Rationale for receptor based Rx Response rates to endocrine manipulation in ER +ve patients was as high as 53% ( only 6% in ER –ve) – Whitliff et al. Receptors correlate with other prognostic markers: 20% 40% 60% Disease-free interval Decreasing tumor size Prolongation of DFS is independent of menopausal status, tumor size, and nodal status. 45% ER-/PR+ 34% ER+/PR- ER-/PR- 80% 100% 78% ER+/PR+ Receptor positivity also correlates with: Cellular turnover rates, Nuclear grade, and Degree of histologic differentiation 0% 10% Mechanism of action All endocrine therapies target the estrogen receptor at one level or other. While the PR receptor doesn't act as a target directly it does indicate a functional ER pathway as it is a ER induced gene. Endocrine therapies Selective Estrogen Receptor Modulators: Letrozole Anastrazole Exemestane Fluoxymesterone Progestins Megestrol acetate Medroxyprogesterone acetate High dose Estrogens Steroidal Antiestrogens: Fulvestrant LHRH agonists Leuprolide Goserelin Aromatase inhibitors: Tamoxifen Torimefene Androgens Gland ablation Ovary Pituitary Adrenals SERM The SERMs are chemically diverse compounds that lack the steroid structure of estrogens but possess a tertiary structure that allows them to bind to the estrogen receptor. Examples: Tamoxifen Raloxifen Toremifene Selective modulation explained by: Differential estrogen-receptor expression in a given target tissue Differential estrogen-receptor conformation on ligand binding Differential expression and binding to the estrogen receptor of coregulator proteins Tamoxifen Chemically a triphenylethylene. The trans isomer is used as a citrate salt. MOA: Competitive binding to the estrogen receptor resulting in reduction of transcription of estrogen regulated genes. Dimethylaminoethoxy side chain and the trans configuration are crucial for the antiestrogenic activity of tamoxifen The net result is a block in the G1 phase of the cell cycle and a slowing of cell proliferation. Tamoxifen is thus, a cytostatic drug. Pharmacokinetics Long t1/2 : 7 -14 days. OD dose can be used Reduced bioavailability is not a cause for resistance. False negative receptor assays for several months after stopping Rx in tumor tissue. Metabolism in liver and excretion in feces ► Renal dysfunction not a contraindication. Metabolized by CYP 450 3A4 enzyme: Can reduce warfarin metabolism. Careful INR monitoring needed in patients receiving warfarin with tamoxifen. Aromatase Inhibitors Include a class of drugs which prevent peripheral conversion of androgens to estrogen. Also cause selective impairment of gonadal steroidogenesis. Thus are capable of selective estrogen deprivation without impairment of adrenal androgen synthesis. Two types exist: Type I : Enzyme inactivators (Steroidal) Type II : Competitive antagonists ( Non steroidal) 3 generations exist: 1st generation: Aminoglutethemide 2nd generation: Formestane (Type I) , Fadrazole 3rd generation: Exemestane (Type I) , Anastrazole , Letrozole, Vorozole 3rd generation AI These drugs inhibit the Aromatase enzyme selectively by blocking the heme moiety of the enzyme. Active sites of other steroidogenic enzymes remain free. 3rd generation AIs are 3 times more potent than aminoglutethemide. Dose: Letrozole (Femara) – 2.5 mg OD Anastrazole (Arimidex) – 1 mg OD Exemestane (Aromasin) – 25 mg OD Anastrazole Letrozole Ovarian Ablation/ Suppression Ovarian ablation classically includes techniques that cause permanent cessation of menstruation. Techniques: Surgical oophorectomy Radiation induced oophorectomy Ovarian suppression on the other hand refers to the suppression of ovarian function through the use of LHRH analogues. Uses: Treatment of breast cancer: Adjuvant setting Metastatic cancer Prevention of hereditary breast cancer syndromes Radiation oophorectomy First series reported by Foveau de Courmelles in 1922 Radiation oophorectomy: Non invasive and cheap procedure. Low dose carries little additional morbidity. However takes time for effect to appear usually 2-3 months For such reason best avoided when prompt relief is needed. Also best reserved for the patient with slow progression of disease. Technique Position: Supine Field selection: Parallel opposing two field technique Energy : Co60 or 6 MV LINAC Dose Schedules: In a younger women 10 – 12 Gy in 5 -6 divided fractions is preferred. In older women shorter course of radiation can give equivalent ovarian ablation. Field borders: The volume of interest is the entire true pelvis 10 x 15 cm field is opened. Lower border is placed just below the superior border of pubic symphysis. Results Treves in 1957 showed that following ovarian irradiation 10 yrs survival improved from 33.8% to 42.3%. Benefit was greater in patients who had node negative disease as compared to patients with node positive disease. Paterson and Russel (1959) also found that survival improved from 54.9% to 62.6% after addition of ovarian irradiation. Endocrine therapy in the adjuvant setting Ca Breast for adjuvant therapy Low risk*, node -ve High risk, node -ve Receptor + ve Receptor - ve Receptor + ve No Rx Node +ve Receptor - ve Chemotherapy Tamoxifen only Premenopausal CCT + Tamoxifen# Postmenopausal CCT + AI * Low risk defined as -ve axillary lymph nodes and tumor size ±1 cm, nuclear grade 1, special histologic type or 1-2 cm tumor with positive steroid receptor and special histologic type. # Ovarian suppression may be considered in those who remain premenopausal after chemotherapy. 23 Adjuvant Tamoxifen alone Several trials have demonstrated that tamoxifen adds significantly to the DFS in the adjuvant setting. Two major trials have also demonstrated a OS benefit Trial Dose Duration DFS OS NATO 20 2 P < 0.05 P < 0.05 Christie 20 1 P < 0.05 NS Stockholm 30 2 P < 0.05 NS CRC 20 2 P < 0.01 NS Scottish 20 5 P < 0.05 P < 0.05 Overall benefits of tamoxifen Rx 1 of every 2 Reduction in Annual Odds ± SE Years Recurrence 0–1 53 ± 5 recurrences and 1 of every 3 deaths are avoided by the tamoxifen therapy. Death 22 ± 10 2–4 42 ± 5 29 ± 6 5–9 31 ± 6 29 ± 5 While the patients are on tamoxifen: Tamoxifen continues to demonstrate further reductions in the odds of recurrence and death in years 5 through 9. This is called the “carryover effect” Optimal Duration of Tamoxifen Rx Reduction in recurrences Reduction in deaths Tamoxifen ~ 1 yr 18% ± 3 11% ± 3 Tamoxifen ~ 2 yr 24% ± 2 14% ± 2 Tamoxifen ~ 5 yr 43% ± 3 23% ± 4 In the EBCTSG meta-analysis 5 yr tamoxifen reduced the risk of recurrence and death twice as much as 2 yr tamoxifen therapy. In two large European trials from Britain and Sweden, women treated with tamoxifen for 5 years, had fewer recurrences and deaths than those treated for only 2 years. Dose of tamoxifen 20 mg once daily dose of tamoxifen is the standard dose. Higher doses are not more effective Also lead to greater incidence of side effects. Tamoxifen in Elderly patients All meta-analyses have demonstrated a stastically significant benefit for addition of Tamoxifen in patients aged > 70 yrs. ECOG evaluated the role of 2yr tamoxifen therapy vs placebo in 180 women aged > 65yrs Drug was well tolerated Significant reduction in recurrences Borderline significant reduction in risk of death Tamoxifen also reduced the incidence of contralateral breast cancers Problems with adjuvant tamoxifen in elderly population: High risk of death for unrelated cancer (22% in ECOG trial) Poor adherence to prescribed treatment Risk of thromboembolism increases with age. Tamoxifen and chemotherapy Advantages of combining CCT with Tmx include: Elimination of both chemoresistant and tamoxifen resistant cell populations. Tamoxifen and progestins inhibit pglycoprotein, an effect that could enhance sensitivity to drugs such as doxorubicin. The apoptosis inhibitor Bcl-2 is down-regulated by tamoxifen, possibly enhancing sensitivity to drugs using this cell death pathway. Disadvantages of combined approach: Cytostatic nature of tamoxifen may interfere with chemotherapy by locking cells in chemoresistant phases of cell cycle. It also antagonizes calmodulin and is an effective Ca2+ channel antagonist—effects that could alter drug uptake. AI in adjuvant setting 7 trials have been reported all of which involve post menopausal females with HR +ve disease. A theoretical priming benefit initial tamoxifen made many trials use tamoxifen in initial 2-3 yrs prior to witching over to tamoxifen. Yrs Tmx N FU (mo) DFS OS MA 17 (Let)* 5 5157 30 2.4% NA ATAC (Ana) 0 6186 68 2.4% 0.3% BIG 01-98 (Let) 0 8010 26 1.9% 0.7% ABCSG/ARNO (Ana) 2 3224 28 2.4% NA ITA (Ana) 2 426 24 7.1% NA IES (Exe) 2-3 4742 31 3.5% 0.6% Trial * Placebo controlled Tamoxifen Toxicity Menopausal symptoms: 50% - 60% ( N.B. 40% 50% in placebo) MC in premenopausal Vaginal dryness and discharge may occur in excess. Maybe seen in as high as 10% of patients. But no randomized comparisons available. Keratopathy, maculopathy & cataract Reported with high doses However NSABP studies have found no increase in vision threatening ocular toxicity. Severe thromboembolism seen in ~ 1% patients in the preventive setting. Risk up to 10 times that experienced by healthy women Complication more common in elderly patients with metastatic breast cancer and who are receiving CCT Carcinogenesis: Ocular toxicity: Thromboembolism: Depression: Increased risk of endometrial cancers (hazard rate of 1.7 per 1000 – NSABP B 14 data) Mostly low grade & stage I tumors. Other tumors: Hepatomas Clear cell sarcomas of ovary Toxicity of AIs vs Tamoxifen MA -17 ATAC BIG IES - 1.7% - 14% - 3.3% - 1.5% Endometrial Cancer NA - 0.6% - 0.4% NA Thromboembolic events NA - 1.7% - 1.2% - .9% Cardiac complications 0.5% 0% 0.4% NA Arthalgia /Myalgia 23% 7% NA 6% Osteoporotic fractures 2.3% 2.2% 1.7& 2% 6% 5% 4% 2% Vaginal Complications Hot flushes Tmx poorer AI poorer Since the absolute benefit of using a AI in adjuvant setting over tamoxifen is ~ 2% reduction in recurrence rates and 1.5% reduction in mortality this excess toxicity needs to be balanced against the bone damage produced by AIs in this setting. Endocrine therapy in the neoadjuvant setup Use of hormone therapy Best suited for a hormone receptor positive, postmenopausal woman Presence of +ve HR strongly influences response to preoperative endocrine therapy Complete and partial response rates of the order of 40 - 70% Majority of patients will have evidence of tumor shrinkage by 3 months. Progression of disease is uncommon in hormonesensitive patients receiving preoperative therapy (<5%) Summary The strategy of preoperative endocrine therapy will require more studies. Exciting area for further translational research: The therapeutic target is known and can, therefore, be measured The biologic pathways arising from the therapeutic target have been extensively studied Slower response to therapy gives a greater window of opportunity for assessing changes in tumor tissue. Caution: 2nd generation taxane based CCT regimes have clinical response rates ranging from 80 -90%. Endocrine therapy in Metastatic Breast Cancer Guidelines Endocrine therapy should be started in all hormone receptor positive females with metastatic breast cancer. Hormone therapy may be suitable as a sole therapy in patients with severe comorbid conditions or very old age. AI are standard 2nd line agents after tamoxifen therapy. Recently evidence has emerged which highlights the superiority of AI in the 1st line setting too. In premenopausal females ovarian ablation may be another alternative. It also allows use of AI in this population. Selection of the appropriate initial management depends on: Tempo of the disease (Slower progress, fewer symptoms) Vital organ involvement ( Bone & Soft tissue) General condition of the patient (Older age, poorer GC) Socio economic conditions. Selection of patient & Rx Site Premenopausal % OR Local recurrence 12% Opposite breast 10% Opposite axilla 10% Bone (osteolytic) 40% Bone (osteoblastic) 30% Lung 15% Liver 11% Brain 2% Soft tissue 15% Neck nodes 13% Ovarian Ablation Postmenopausal Tamoxifen AIs Resistance Fulvestrant / Progestins ?? High dose Estrogen Tumor Flare Tumor Flare: Incidence: 4% to 7% with high-dose estrogen 3% to 13% with tamoxifen Dramatic in bone pain, an in size & number of metastatic skin nodules, and erythema. Within days to several weeks after starting treatment Hypercalcemia in 5% Tumor regression may occur as the flare reaction subsides Look for objective evidence of disease progression if the patient's symptoms have not resolved by 4 to 6 weeks as flare is transient AI : 1st line therapy 3 major pahse III trials have directly compared tamoxifen against AI. All have shown an improvement in time to progression (TTP) The study by the International Letrozole Breast Cancer Group is the largest in the series. Trial Drug Nabholtz et al1 Ana TARGET trail2 Ana N 353 Tmx 668 Tmx Mouridsen et al5 Let Tmx 907 RR TTP (mo) Comment 21% 11.1* 17.7% 5.6 32.9% 8.2 32.6% 8.3 Retrospective analysis revealed longer TTP with Anastrazole after combining these two trials3,4 30% 9.4 20% 6.0 41 Taxanes — Taxanes are among the most active agents for metastatic breast cancer – Docetaxel, Paclitaxel, NabPaclitaxel. Anthracyclines – Doxorubicin, Epirubicin, Caelyx. Capecitabine / 5 FU Eribulin Vinorelbine Gemcitabine Ixabepilone Etoposide Cyclophosphamide Methotrexate Platinum agents Combination Chemotherapy High Dose Chemotherapy and Stem Cell Transplant – no benefit. Common Adjuvant Regimens First Generation 20% → Second Generation CMF*6 → CAF*6, CEF*6 CMF*6 → CE(50)F*6 20% → Third Generation FAC*6 → TAC*6 → CE(100)F*6 → FEC*3→D*3 AC*4 → AC*4→Txl*4 q3wk → Dose Dense (CA*4→Txl*4 q2wk) AC*4 → TC*4 Doxorubicin R A N D O M I Z E Cyclophosphamide 60 mg/m2 IV Day 1 600 mg/m2 IV Day 1 Every 21 days x 4 cycles Docetaxel Cyclophosphamide Every 21 days x 4 cycles 75 mg/m2 IV Day 1 600 mg/m2 IV Day 1 2nd Generation Adjuvant Chemo Trials First Generation → Second Generation → Third Generation CMF*6 → CAF*6, CEF*6 CMF*6 → FAC*6 → TAC*6 CE(50)F*6 → CE(100)F*6 → FEC*3→D*3 AC*4 → AC*4→Txl*4 q3wk → Dose Dense (CA*4→Txl*4 q2wk) AC*4 → TC*4 45 46 What’s the Goal? • Select patients who will require systemic therapy • Find predictive factors (either before or early in treatment) that allow for accurate tailoring of therapy 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 File:1911 Solvay conference.jpg DCIS Heterogeneous group of proliferative lesions & have diverse malignant potential DCIS accounts for approx 21% of all new breast cancers diagnosed in the US. Over 90 % of which are detected only on imaging studies. ADJUVANT RADIOTHERAPY FOR INVASIVE BREAST CANCER 50 Gy / 25 # , 42.4 Gy / 16 # , 40.05 Gy / 15 # -Breast Conserving Surgery -Post Mastectomy ( Absolute ) T3 / T4 / >=4 positive nodes / close or positive margins. ( Relative ) >2 cm tumor , LVI, Grade 3, Age < 50, 1 – 3 positive nodes, ENS, receptor negative tumors, lobular histology. Boost – Age < 50 , close or positive margins. 16 Gy/8# , 10 Gy/5# , 9 Gy/3# Early side effects Skin changes Tiredness Nausea. Potential long-term side effects Cosmetic – telangectasia , pigmentation , scarring , pain Restricted shoulder movement Cardiac complications Pneumonitis , fibrosis Effect on the bones Lymphedema Brachial plexopathy Radiation induced second malignancies. MALE BREAST CANCER Breast cancer is much less common in men than in women. Men tend to present at an older age than women. Invasive ductal breast cancers predominate in men (≥90 percent) Breast cancers that arise in men are more often hormone receptor positive than female breast cancers, but they less often overexpress HER2. Mammography is abnormal in 80 to 90 percent of cases, and can usually differentiate breast cancer from gynecomastia. Biopsy is required to confirm the diagnosis and assay for hormone receptors and HER2 expression, both of which may influence the selection of treatment. Any man with a diagnosis of breast cancer should be referred for genetic counseling and BRCA testing. Treatment on lines very similar to female breast cancer TREATMENT PATTERNS OF OLDER WOMEN — Often receive less than standard therapy worldwide. In the largest study, which involved over 120,000 women, increasing age was associated with the following treatment trends ●Decreased surgical rates. ●Less frequent use of adjuvant radiation therapy (RT) following breast conservation surgery ●Increased use of primary endocrine therapy – Primary endocrine therapy (without surgical treatment) was administered in a higher proportion of women as age increased. In addition, older women have generally not participated in clinical trials evaluating the treatment of breast cancer. As a result, there is a lack of evidence-based guidelines to inform the treatment of breast cancer in this population. Breast cancer is a major health concern in the geriatric population. Patients with breast cancer over age 65 to 70 years should be screened for geriatric syndromes using a brief tool. The treatment approach to medically fit older women with newly diagnosed non-metastatic breast cancer is similar to that of younger women. For medically frail women with breast cancer who are not candidates for surgery (including those who decline surgery) -For patients with hormone receptor-positive breast cancer, we offer primary endocrine therapy rather than chemotherapy.) -For patients with hormone receptor-negative disease, we suggest single agent chemotherapy rather than combination chemotherapy -For patients with HER2-positive disease (regardless of hormone receptorstatus), we suggest single agent HER2-directed therapy -An alternative option would be to add a HER2-directed agent to systemic therapy, provided patients are aware of the additional risks associated with combined treatment. -Supportive care and referral for palliative care services. Gestational breast cancer - is commonly defined as breast cancer that is diagnosed during pregnancy, in the first postpartum year, or any time during lactation. ●In general, pregnant women with breast cancer should be treated according to guidelines for non-pregnant patients, with some modifications to protect the fetus. ●Either breast conserving surgery or mastectomy is a reasonable option in the pregnant woman with breast cancer. A choice between them is guided by tumor characteristics and patient preferences. ●Women with breast cancer during pregnancy should undergo an axillary node dissection. The safety of sentinel lymph node biopsy has not been established. ●For women who require adjuvant radiation therapy (RT), we recommend adjuvant RT be administered after delivery rather than during pregnancy ●For women in whom chemotherapy is recommended, we initiate treatment after the first trimester. ●We recommend against use of Herceptin during pregnancy due to fetal risks , and fetal death Thank You