Paediatric safe prescribing: do inpatient prescriptions adhere to hospital guidelines
for safe prescriptions and antibiotic prescribing?
Dr Claire Hawcroft and Dr Camilla Eiffe, F1 doctors in Paediatrics.
claire.hawcroft@doctors.org.uk
St George’s Hospital, London. February 2011.
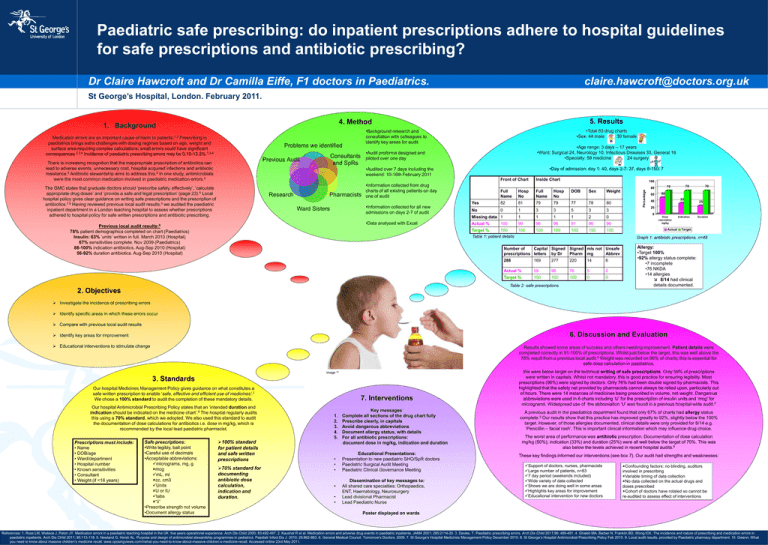
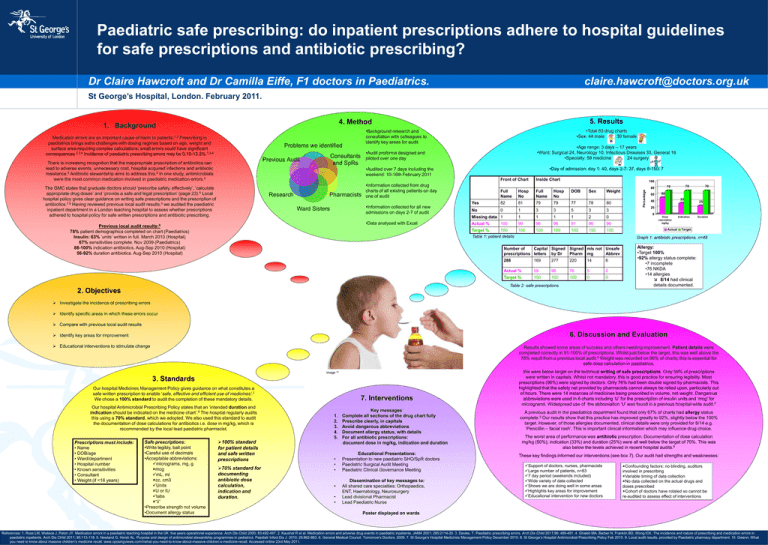
5. Results
4. Method
Medication errors are an important cause of harm to patients.1,2 Prescribing in
paediatrics brings extra challenges with dosing regimes based on age, weight and
surface area requiring complex calculations; small errors could have significant
consequences.2,3,4 Incidence of paediatric prescribing errors may be 0.15-13.2%.1,3,4
Problems we identified
•Age range: 3 days – 17 years
•Ward: Surgical 24, Neurology 10, Infectious Diseases 33, General 16
•Specialty: 59 medicine
24 surgery
•Audit proforma designed and
piloted over one day
Consultants
and SpRs
Previous Audit
There is increasing recognition that the inappropriate prescription of antibiotics can
lead to adverse events, unnecessary cost, hospital acquired infections and antibiotic
resistance.5 Antibiotic stewardship aims to address this.5 In one study, antimicrobials
were the most common medication involved in paediatric medication errors.2
•Total 83 drug charts
•Sex: 44 male
39 female
•Background research and
consultation with colleagues to
identify key areas for audit
•Day of admission: day 1: 40, days 2-7: 37, days 8-150: 7
•Audited over 7 days including the
weekend: 10-16th February 2011
Front of Chart
The GMC states that graduate doctors should ‘prescribe safely, effectively’, ‘calculate
appropriate drug doses’ and ‘provide a safe and legal prescription’ (page 23).6 Local
hospital policy gives clear guidance on writing safe prescriptions and the prescription of
antibiotics.7,8 Having reviewed previous local audit results,9 we audited the paediatric
inpatient department in a London teaching hospital to assess whether prescriptions
adhered to hospital policy for safe written prescriptions and antibiotic prescribing.
Research
Pharmacists
•Information collected from drug
charts of all existing patients on day
one of audit
•Information collected for all new
admissions on days 2-7 of audit
Ward Sisters
•Data analysed with Excel
Previous local audit results:9
78% patient demographics completed on chart (Paediatrics)
Insulin: 63% ‘units’ written in full. March 2010 (Hospital)
67% sensitivities complete. Nov 2009 (Paediatrics)
88-100% indication antibiotics. Aug-Sep 2010 (Hospital)
56-92% duration antibiotics. Aug-Sep 2010 (Hospital)
Inside Chart
100
Full
Name
Hosp
No
Full
Name
Hosp
No
DOB
Sex
Weight
Yes
82
81
79
79
77
78
80
No
0
1
3
3
5
3
3
Missing data 1
1
1
1
1
2
skjdjlj
0
Actual %
99
96
96
91
96
96
100
100
100
100
100
100
Target %
100
100
Table 1: patient details
60
70
70
80
Percentage
1. Background
70
50
33
40
25
20
0
Dose
calculation
mg/kg
Actual
Indication
Duration
Target
Graph 1: antibiotic prescriptions, n=48
Number of
Capital Signed
prescriptions letters by Dr
Signed mls not Unsafe
Pharm mg
Abbrev
288
169
277
220
14
6
Actual %
59
96
76
5
2
Target %
100
100
100
0
0
Table 2: safe prescriptions
Allergy:
•Target 100%
•92% allergy status complete:
•7 incomplete
•76 NKDA
•14 allergies
8/14 had clinical
details documented.
2. Objectives
Investigate the incidence of prescribing errors
Identify specific areas in which these errors occur
Compare with previous local audit results
6. Discussion and Evaluation
Identify key areas for improvement
Educational interventions to stimulate change
Results showed some areas of success and others needing improvement. Patient details were
completed correctly in 91-100% of prescriptions. Whilst just below the target, this was well above the
78% result from a previous local audit.9 Weight was recorded on 96% of charts; this is essential for
safe dose calculation in paediatrics.
Image 10
3. Standards
Our hospital Medicines Management Policy gives guidance on what constitutes a
safe written prescription to enable ‘safe, effective and efficient use of medicines’.7
We chose a 100% standard to audit the completion of these mandatory details.
Our hospital Antimicrobial Prescribing Policy states that an ‘intended duration and
indication should be indicated on the medicine chart’.8 The hospital regularly audits
this using a 70% standard, which we adopted. We also used this standard to audit
the documentation of dose calculations for antibiotics i.e. dose in mg/kg, which is
recommended by the local lead paediatric pharmacist.
Prescriptions must include:
• Name
• DOB/age
• Ward/department
• Hospital number
• Known sensitivities
• Consultant
• Weight (if <16 years)
Safe prescriptions:
•Write legibly, ball point
•Careful use of decimals
•Acceptable abbreviations:
micrograms, mg, g
mcg
mL, ml
cc, cm3
Units
U or IU
tabs
“ii”
•Prescribe strength not volume
•Document allergy status
100% standard
for patient details
and safe written
prescriptions
70% standard for
documenting
antibiotic dose
calculation,
indication and
duration.
7. Interventions
1.
2.
3.
4.
5.
•
•
•
•
•
•
We were below target on the technical writing of safe prescriptions. Only 59% of prescriptions
were written in capitals. Whilst not mandatory, this is good practice for ensuring legibility. Most
prescriptions (96%) were signed by doctors. Only 76% had been double signed by pharmacists. This
highlighted that the safety net provided by pharmacists cannot always be relied upon, particularly out
of hours. There were 14 instances of medicines being prescribed in volume, not weight. Dangerous
abbreviations were used in 6 charts including ‘U’ for the prescription of insulin units and ‘mcg’ for
micrograms. Widespread use of the abbreviation ‘U’ was found in a previous hospital-wide audit.9
Key messages:
Complete all sections of the drug chart fully
Prescribe clearly, in capitals
Avoid dangerous abbreviations
Document allergy status, with details
For all antibiotic prescriptions:
document dose in mg/kg, indication and duration
A previous audit in the paediatrics department found that only 67% of charts had allergy status
complete.9 Our results show that this practice has improved greatly to 92%, slightly below the 100%
target. However, of those allergies documented, clinical details were only provided for 8/14 e.g.
‘Penicillin – facial rash’. This is important clinical information which may influence drug choice.
Educational Presentations:
Presentation to new paediatric SHO/SpR doctors
Paediatric Surgical Audit Meeting
Paediatric Clinical Governance Meeting
These key findings informed our interventions (see box 7). Our audit had strengths and weaknesses:
Dissemination of key messages to:
All shared care specialties: Orthopaedics,
ENT, Haematology, Neurosurgery
Lead divisional Pharmacist
Lead Paediatric Nurse
The worst area of performance was antibiotic prescription. Documentation of dose calculation
mg/kg (50%), indication (33%) and duration (25%) were all well below the target of 70%. This was
also below the levels achieved in recent hospital audits.9
Support of doctors, nurses, pharmacists
Large number of patients, n=83
7 day period (weekends included)
Wide variety of data collected
Shows we are doing well in some areas
Highlights key areas for improvement
Educational intervention for new doctors
Confounding factors: no blinding, auditors
involved in prescribing
Variable timing of data collection
No data collected on the actual drugs and
doses prescribed
Cohort of doctors have rotated so cannot be
re-audited to assess effect of interventions
Poster displayed on wards
References: 1. Ross LM, Wallace J, Paton JY. Medication errors in a paediatric teaching hospital in the UK: five years operational experience. Arch Dis Child 2000; 83:492-497. 2. Kaushal R et al. Medication errors and adverse drug events in paediatric inpatients. JAMA 2001; 285:2114-20. 3. Davies, T. Paediatric prescribing errors. Arch Dis Child 2011;96: 489-491. 4. Ghaleb MA, Barber N, Franklin BD, Wong ICK. The incidence and nature of prescribing and medication errors in
paediatric inpatients. Arch Dis Child 2011; 95:113-118. 5. Newland G, Hersh AL. Purpose and design of antimicrobial stewardship programmes in pediatrics. Paediatr Infect Dis J 2010; 29:862-863. 6. General Medical Council. Tomorrow’s Doctors. 2009. 7. St George’s Hospital Medicines Management Policy December 2010. 8. St George’s Hospital Antimicrobial Prescribing Policy Feb 2010. 9. Local audit results, provided by Paediatric pharmacy department. 10. Gwenn. What
you need to know about massive children’s medicine recall. www.oposingviews.com/i/what-you-need-to-know-about-massive-children-s-medicine-recall. Accessed online 23rd May 2011.