OB/gyn Week 4a
Gynecologic Infxns
Normal Vaginal Ecosystem
• pH ~ 4.0
– Estrogen stimulates glycogen
– Glycogen metabolized to lactic acid by
lactobacillus (healthy vaginal flora)
• Many aerobic, anaerobic, and fungal
organisms present
• Normal vaginal secretions (vary with cycle)
– White, floccular, odorless
– Present in fornix, not usually on vaginal walls
Vulvovaginitis
• Vaginal discharge is the most common
symptom in gynecology
• Three common infectious causes
– Bacterial Vaginosis (BV)
– Trichomonas vaginalis
– Candida albicans
• Common non-infectious causes
– Atrophic vaginitis
– Desquamative inflammatory vaginitis
Vulvovaginitis
• Bacterial Vaginosis (BV)
– Most common vaginal infection
– Associated with PID, endometritis, premature rupture of
membranes during labor, post-op infections of upper genital tract
– Can occur with or without sexual activity
(treat partner if infection is recurrent or stubborn)
• Trichomonas
– Not associated with upper tract infections
– May be a vector for other bacterial or viral diseases
– Sexually transmitted
• Candida
– Not strictly considered an STI
– Not associated with upper tract infections
– Symptoms may be hypersensitivity related
Vulvovaginitis
• Less common causes of vulvovaginitis
– Cytolytic Vaginosis (CV)
• Not an STI
• Not associated with upper tract disease
• Cells lyse, which is painful.
– Lactobacillosis (LB)
• Same as above
• Cells don’t lyse.
Evaluation of Vaginal
Discharge
• History – Problem focused
– HPI, PMHx, PFSHx, ROS, use of irritants or allergens
• PE
– vulvar inspection, speculum exam, bimanual exam
• Lab/Diagnostic testing
– pH
– Wet mount
– Cultures if appropriate
– PAP if appropriate
– Serology and other blood tests as appropriate
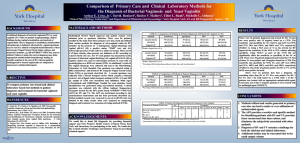
Vaginal
discharge
Present at
introitus
Color
Viscosity
Consistency
Location in
vagina
Normal
BV
No
Yes
White
Gray
Trich
Candida
Yes
Yes
Profuse
Yellowgray
High
Low
Low
Floccular Thin
Thin
Frothy
Fornix
Vaginal Vaginal
walls
Walls
White
High
Curdy
Vaginal
walls
Sx
Normal
None
BV
Odor,
Discharge
PE
Normal
No
inflammation
pH
Amine
<4.5
Neg
>4.5
Pos
Wet
mount
Lacto- Clue cells,
bacillus decreased
Lactobacillus
Trich
Pruritus,
Profuse
discharge,
Odor
Erythema,
Edema
>4.5
Occ. Pos
Candida
Pruritus,
Discharge
Erythema,
Excoriation
<4.5
Neg
Motile
Hyphae or
organisms, budding
WBC’s
yeast
Desquamative Inflammatory
Vaginitis
• Cause unknown - may be autoimmune
• Sx’s – purulent discharge, burning,
dyspareunia
• Vagina and vulva erythematous
• pH > 4.5
• Absence of lactobacilli
Atrophic Vaginitis
• Common in peri, post-menopausal women
• Result of decreased estrogen activity
– Less glycogen, less lactic acid, pH rises
•
•
•
•
•
Sx’s – vaginal pruritus, burning, spotting
Discharge minimal
Vaginal walls thin, lack rugae
pH >5
Wet mount – decreased lactobacillus,
parabasal cells, WBC’s
Cytolytic Vaginosis &
Lactobacillosis
• Cause unknown
• Sx’s – from thin/watery to thick/curdy
discharge, burning, dyspareunia
• pH 3.5-4.5 (Lower than normal pH )
• Overgrowth of lactobacilli
• In CV, cytolysis of vaginal epithelial cells
TREATMENT OF
VULVOVAGINITIS
• Bacterial Vaginosis
– Conventional
• Metronidazole (oral and/or topical)
• Clindamycin (oral and/or topical)
Bacterial Vaginosis
• Naturopathic treatment
– Strategies
•
•
•
•
•
Lower pH
Promote immune response
Restore flora balance
Reduce inflammation
Provide anti-microbial activity
SAMPLE TREATMENT
REGIMEN FOR BV
• Nutrition
– Avoid refined CHO (carbos)
– Live culture yogurt
• Vitamin A and/or E vaginal suppositories
• Lactobacillus – 1 capsule vaginally X 7 days
• Boric acid – 600 mg vaginal suppository – 1
daily X 7 days
TRICHOMONAS
• Conventional treatment
– Metronidazole
• Treatment of partner may be indicated
TRICHOMONAS
• Naturopathic treatment
– Strategies – same as BV
• Sample treatment regimen for trichomonas
– Immune and anti-inflammatory support as
indicated
– Melaleuca oil (tea tree) suppositories 1 vaginally X
7-10 days – this is 40% tea tree oil
– Lactobacillus vaginal suppositories
CANDIDA VULVOVAGINITIS
• Conventional treatment
– Topical imidazoles or triazoles – creams or
suppositories 1, 3, or 7 days OR
– Nystatin 100,000 unit vaginal tablet X 14
days OR
– Fluconazole oral 150 mg single dose
CANDIDA VULVOVAGINITIS
• Naturopathic treatment
– Same as BV except no pH lowering
• Sample treatment regimen for candida
– Nutrition
• Avoid refined CHO
• Live culture yogurt
– Immune and anti-inflammatory treatments as indicated
– Boric acid suppositories 600 mg vaginally qD X 3-7 days
– Lactobacillus suppositories 1 vaginally qD X 3-7 days
– Vitamin A and E vaginal suppositories
Treatment for CV
(Cytolytic Vaginosis )
• Conventional
– Increase vaginal pH
• Douche or sitz bath in Na bicarbonate
– 1 tsp. In 1 pint H2O 1-2 X week OR
– 2-4 TBSP in 2 inches warm bath water 15 min. 2-3 X week
• Discontinue tampon use for at least 6 months
• Naturopathic
– Same as above
– (don’t use probiotics to treat these!)
Treatment for Desquamative
Vaginitis
• Conventional
– Intravaginal corticosteroids OR
– 2% clindamycin cream – anti-inflammatory
– Recurrence rate 30% - treat again if necessary
• Naturopathic
– Strategies –soothe tissue and restore flora
• Calendula herbal douche or suppositories daily X 7
days
• Saline douche?
• Probiotic suppositiories X 7 days
ATROPHIC VAGINITIS
• Conventional treatment
– Topical estrogen cream (vaginally) OR
– Oral estrogen OR
– Transdermal estrogen OR
– Vaginal lubricants PRN - Replens
Atrophic Vaginitis
– Treatment Strategies
• Support endogenous estrogen activity
• Supply exogenous estrogen
• Provide anti-inflammatory support
– Sample treatment regimen
• Soy and other phytoestrogens in diet
• Vitamin E suppositories 400 iu vaginally 1 X week
• Oral phytoestrogens as indicated
• DHEA may help treat vaginal atrophy
• Stimulate vaginal epithelium but not uternine
endometrium
• Increased bone density
[From Natural Medicines Comprehensive Database]
Vaginitis:
General Preventative Measures
•
•
•
•
•
•
Avoid sexual activity during treatment
Wear loose fitting clothing
Wear cotton underwear
Do not douche routinely
Wash/bathe with gentle, non-irritating soaps
Barrier contraceptive techniques may reduce
recurrence and transmission (partner to
partner)
• Eat a whole foods diet
CERVICITIS
• Cervix is made up of two epithelial cell types
– Squamous and columnar
• Squamous epithelium is the ectocervix
– BV, trich, candida, HSV, HPV can infect
• Columnar epithelium is the endocervix
– between them is transitional zone
• Mucopurulent cervicitis (MPC) is an infection of
the columnar epithelium of the cervix
– Chlamydia trachomatis (CT) and Neisseria gonorrhoeae
(GC) are primary infectious agents
Diagnosis of MPC
• Symptoms
–
–
–
–
Vaginal discharge
Dyspareunia (pain with sex)
Postcoital bleeding
Spotting
UP TO 60% OF WOMEN WITH CT or GC ARE ASYMPTOMATIC
• Signs
– Hypertrophy and/or edema of cervix
– Mucopurulent, yellow discharge from cervix
• Diagnosis confirmed by gram stain of discharge
• Organism ID’d by culture or PCR test of
endocervical or urine sample
Treatment of MPC
• Conventional treatment is antibiotics
(CDC has current recommendations)
• Naturopathic treatment
– Conventional antibiotic AND
– Immune support
– Oral probiotic support
• COMPLICATIONS OF UNTREATED CT/GC
INCLUDE PID, SALPINGITIS, INFERTILITY
KEY CONCEPTS
• Appropriate Hx critical to providing diagnostic information
• Vulvovaginitis
– BV, Trich, Candida, CV, LB, DIV, atrophic vaginitis
– Diagnosed with characteristics of discharge, pH, wet mount
– Naturopathic treatments effective
• Cervicitis
–
–
–
–
–
CT, GC main causes
Often asymptomatic, or mucopurulent discharge
Dx by culture or PCR of endocervical sample
Antibiotics with adjunct support is optimum tx approach
Ineffective treatment can result in PID, infertility
Infestations: Crab Lice
• Pediculosis Pubis: crab louse (Phthirus
pubis) infestation
– Different species than head or body louse
– Transmitted by close (usually sexual)
contact, MAY also be via infected towels, or
bedding
– Most contagious of all STDs
– Eggs deposited on base of pubic hair
Pubic Lice
• Symptoms:
– Itching in pubic area
– Allergic sensitization develops over at least
5 days to weeks
– Definitive diagnosis via microscopic
visualization of louse
Pubic Lice
• Crab louse:
Infestations: Scabies
• Scabies: parasitic infection of itch mite
(Saroptes scabiei)
• Transmitted by close contact and infected
bedding/ clothes
• Widespread over body (no predilection for hairy
areas as lice)
• Travels rapidly over skin, but able to survive
only a few hours away from warmth of skin
• Predilection for warm, moist areas (folds of skin
or under elastic bands)
• Not exclusively a gynecological infection
Scabies
• Symptoms
– Severe, intermittent itching
– Onset of itching may be up to 3 weeks after
infection
– Red, thin, burrow under skin surface
– May imitate any other itchy dermatological
condition
Scabies
Infestations: Treatment
Conventional
• Pediculosis pubis: Permethrin 1% cream rinse
applied to pubic area, rinsed off after 10 minutes
• Scabies: Permethrin 5% cream applied all over
body (except face) overnight (8-14 hours), then
washed off
*Permethrin is neurotoxic and carcinogenic
Natural treatments take more time and care to
achieve results - wash all bedding/clothes/etc,
apply mix of tea tree oil and olive oil to area
Viral infections:
Molluscum Contagiosum
• Molluscum Contagiosum
– In children may appear all over body
– In adults it is an asymptomatic viral disease
of primarily the vulvar skin
– Appear as small nodules or domed
papules, have “umbilicated center”
– Caused by poxvirus
– Mildly contagious; spread via sexual and
nonsexual contact and auto-inocculation
Molluscum Contagiosum
Molluscum Contagiosum
• Molluscum contagiosum treatment:
–
–
–
–
Cryosurgery
Electrocautery
Excision
Trichloroacetic acid or Ferric subsulfate or
iodine
Viral Infections:
Genital Warts
• Condyloma acuminatum: genital warts
– HPV
– Clinically recognizable, macroscopic lesion in only
30% of cases
– Prevalence as high as 50% in sexually active
teenagers with multiple partners
– Several morphologic types
– May occur singularly or in clusters
– Usually asymptomatic but may cause pain, itching,
tendency to bleed depending on size and location
Genital Warts
Genital Warts
• Treatment of external genital warts
–
–
–
–
Cryosurgery
Surgical excision
Laser surgery
Chemical applications
•
•
•
Podofilox 0.5% solution
Podophyllin resin 10%-25%
Imiquimod 5% cream
– Natural therapies
•
•
Immune support
Topical thuja oil
Viral Infections: HSV
• Genital herpes
– Herpes simplex virus HSV I (classically
oral) and HSV II (classically genital)
– Recurrent, incurable epidemic disease
– 60 million individuals in US infected
• 80% unaware
• Asymptomatic transmission
– Not physically debilitating but overwhelming
psychologic burden
HSV
• Herpes simplex virus
–
–
–
–
Majority new infections in women ages 15-35
Incubation period 3-7 days
Multiple crops of ulcers for 2-6 weeks
Prodrome: tingling sensation prior to
outbreak – contagious as of this stage
– Viral shedding 2-3 weeks after vulvar lesions
appear
– Severe vulvar pain, tenderness, inguinal
adenopathy, pruritis, discharge
– Systemic symptoms such as fever, malaise,
associated with primary outbreak
HSV
• Herpes simplex virus
– Average four recurrences during the first year
– Recurrences may be asymptomatic
– 80% chance recurrence first year with HSVII;
55% HSVI
– Recurrences triggered by stress, menses, illness
– Recurrent infections may appear in extra-genital
sites
– Virus resides in a latent phase in dorsal root
ganglia of S2-S-4
HSV
HSV
• Major concern is risk of transmission
– Avoid sexual intercourse from onset of
prodromal symptoms until all lesions
healed
– Active viral shedding may occur even in the
absence of symptoms
– Inform potential sexual partners
– Use condoms even while asymptomatic
– Avoid oral-genital and oral-oral contact
during “fever blister” (HSV infection on
face/ around mouth)
HSV
• Herpes simplex virus I and II Treatment
– Acyclovir, Famciclovir, Valacyclovir
• Higher doses more frequently during outbreak
• Lower doses less often as suppressive therapy
• Natural therapies:
– L-lysine - 500-1200 mg daily (preventative), and
1-5 grams daily during prodrome/outbreak
– Anti-viral herbs: Lemon balm, Licorice, Lomatium
– Healthy nutrition (low sugar, refined carb, healthy
fats and proteins)
Bacterial: Soft Chancre
• Chancroid: soft ulcerative lesion on vulva
– Initial lesion soft papule
– Papule becomes pustule which then ulcerates,
becomes painful and tender
– Dirty, grey, nectotic, foul-smelling exudate
• Haemophilus ducreyi: highly contagious
• Short incubation period: 3-6 days
• Needs opening through skin to infect: tissue
trauma, excoriation
• Conventional tx = Antibiotics
*Rare in U.S. - more common in developing regions
Chancroid
Bacterial: Syphilis
• Syphillis: complex systemic disease
produce by Treponema pallidum
• Cofactor in transmission and acquisition
of HIV
• “Great imitator” may present as many
different diseases
• Incubation period 10-90 days
Syphilis
• Primary syphilis
– Hard chancre: painless ulcer on vulva,
vagina, or cervix (5% on extragenital
regions)
• Usually solitary, red, round ulcer with firm, wellformed, raised edges, yellow-grey exudate
• Heals spontaneously within 2-6 weeks
• May be asymptomatic
– Regional lymphadenopathy
Syphilis
• Secondary syphilis
– Systemic spread via blood
– 50% of untreated primary syphilis
progresses to secondary
– Other 50% becomes latent infection
– Develops between 6 weeks and 6 months
– Most infections during the first 2 years of dz
– Symptoms:
• Classic red rash on palms and soles
• Condyloma latum: large, raised greyish-white
areas on vulva
1° and 2° Syphilis
Syphilis
• Tertiary Syphilis
– Develops is 33% of those not treated during
primary, secondary, or latent phases
– Destructive effects on CNS, cardiovascular and
musculoskeletal systems
•
•
•
•
•
Optic atrophy
Tabes dorsalis (degeneration of sensory neurons)
Generalized paresis
Aortic aneurysm
Gumma of skin and bones (abscess with obliteration of
small vessels and necrosis)
Syphilis
• Diagnosis:
– Serologic tests positive 4-6 weeks post
exposure
– Screening: VDRL, RPR tests inexpensive,
easy to perform but non-specific (many false +)
– Dark-field microscopy to confirm
– CSF examination if any neurologic or
ophthalmologic signs or symptoms, HIV
infection
– Test for HIV infection
Syphilis
• Syphilis Treatment:
– IM Penicillin
• Titers should be measured in 6 and 12 months
– Tetracycline or Doxycycline if penicillin
allergy
– Evaluation and treatment of sexual partners
Bacterial: TSS
• Toxic shock syndrome
– Acute, febrile illness produced by bacterial
exotoxin (S. aureus)
– Involves multiple organ systems
– 50% cases sequelae of focal skin infection
(usu. post surgery or procedure)
– 50% of cases are menses related
• History of foreign object in vagina (tampon,
diaphragm)
TSS
• TSS requirements for illness
development:
– Colonization or infection with
Staphyloccocus aureus
– Bacterial production of TSS toxin-1
– Toxins need route of entry into systemic
circulation
• Micro-ulcerations from tampons may
provide toxin’s entry into systemic
circulation
TSS
• TSS symptoms
–
–
–
–
Unexplained fever after menses
Rash after menses
Prodromal flulike illness first 24 hrs
High fever with headache, myalgia, sore
throat, vomiting, diarrhea, generalized skin
rash, hypotension
– Rash: first appears as intense sunburn,
becoming macular after 48 hrs, then flaky
desquamation of skin over face and trunk
– Tenderness of external genitalia
TSS
• TSS Diagnosis:
• Culures of vagnia, cervix, and blood
• Rule out Rocky Mountain spotted fever, scarlet
fever, leptospirosis
• Treatment:
– Requires ICU care
– IV antibiotics, fluids, steroids for severe
cases