Female, Adolescent,
Gynaecological
Multidisciplinary Network
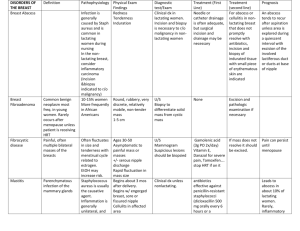
Diagnostic criteria
Mayer-Rokitansky Syndrome (MRKH)
Congenital Adrenal Hyperplasia (CAH)
Androgen Insensitivity Syndrome: Complete and partial (AIS; CAIS)
Gonadol Dysgenesis and Turner’s Syndrome
Premature Ovarian failure
Vaginal tissue abnormalities i.e. graft vs host disease
Didelphus uterus and other uro-genital septum abnormalities
Uro-genital structural abnormalities from S.A & FGC abnormalities
Paediatric & Adult gynaecologists
Lead consultants: Valeria Ivanova; Anna Bashford; Paddy
Moore
MRKH & 1:10 urethral displacement, Shear's vaginoplasty
all Mullerian anormalies: i.e. Didelphus uterus or partial
endometrial or uterine tissue
other uro-genital differences that require reconstructive
surgery and medical treatment i.e. vaginal scarring
Support endocrinology with laparoscopic diagnosis, EUA,
gonad removal, and any surgery required by CAH and AIS
young women etc.
Endocrinology
Lead consultants: Stella Milsom & Megan Ogilive
Congenital Adrenal Hyperplasia (CAH)
Partial and Complete Androgen Insensitivity Syndrome (AIS:CAIS)
Premature ovarian shut down
Turner’s and Gonadol dysgenesis
All other metabolic and karotype differences that impact on
fertility and sexual functioning, gender orientation.
Support colleagues with HRT advise
Currently our lead researchers/publishers.
Physiotherapy: Jillian Wood
Major role in vaginal construction through dilation
Provides a pelvic floor assessment to assist diagnosis and
treatment plans
Reversing hypertonic pelvic muscles and pain syndromes
from past treatment, historical S.A., circumcision
MRKH women with urethral differences, continence and
hypertonic pelvic floors/pain problems
Associated urinary & bowel problems
Prepares adolescents for Internal exams
Clinical Psychologist (Prue)
Works within a Critical Health theoretical paradigm
Facilitates treatment outcomes by identifying individual’s
subjective desires that may not fit within cultural or medical
normative practises
Where subjective desire is co-constituted through the
intersection of our physical bodies, cultural training and
available material resources.
Example: The idea of being ‘intersex’ has been formed
through advocacy groups and the shift in medical treatment
protocol’s, which themselves are both material and cultural
resources
Psychology assumptions:
Therefore we cannot assess our patients future needs
through either medical or cultural theoretical models alone
This group of patients have very specific competing desires
i.e. such as wanting to be ‘normal’ and have ‘sex’ like their
friends but have different corporeal bodies which are not
necessarily ready to structurally change to fit cultural
norms
Because subjective desire is co-constituted through the
intersection of unstable bodies within unstable cultures,
sexual preferences and gender orientation are not always
stable.
Psychology Assessment necessary for
treatment decisions
Physical & emotional safety
Cognitive and emotional development
Interdependent and independent decision-making
Understands and is adjusting to diagnosis
Can tolerate the unexpected and understands medical limitations in that we cannot
predict every treatment outcome
Can identify current gender orientation, sexual readiness and preferences
Maintains family, friendship relationships and avoids social isolation
Have a critical analysis of medical and cultural norms and can negotiate their own
treatment preferences within our clinic
Corporeal readiness for dilation necessary for vaginal construction
Aims for national network
(FPAMN)
Equal and standardize access within NZ
Access to a corporeal form (where medically & financially
possible) that meets patients preferences
Provide a seamless & consistent transfer from paediatric
services
To audit our services fit with current social/medical ethics
and does not marginalize sexual/cultural differences
Succession planning to maintain expertise within NZ
6-12 monthly goals for FPAMN
network (if funded)
To increase from our current 188-240 appointments per year
To appoint a co-ordinator
To run weekly clinics within GOP National Women’s
To develop strong network ties and training throughout NZ
To provide virtual consultations throughout NZ
To formulate a website and patient information pamphlets