Systemic T-cell Lymphoma
advertisement

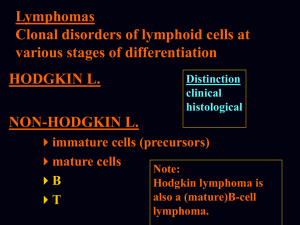
Clinical Exchanges in T-cell Lymphomas: Expert Insight into Current Issues and Future Directions Steven Horwitz, MD Memorial Sloan Kettering Cancer Center New York, NY WHO 2008 CLASSIFICATION OF MATURE T/NK-CELL NEOPLASMS T-cell prolymphocytic leukemia Mycosis fungoides T-cell large granular lymphocytic leukemia Sezary syndrome Chronic lymphoproliferative NK cells Primary cutaneous CD30+ lymphoproliferative Aggressive NK-cell leukemia Adult T-cell lymphoma/leukemia Systemic EBV-positive T-cell lymphoma Extranodal NK/T-cell lymphoma, nasal type Enteropathy-type intestinal T-cell lymphoma Hepatosplenic T-cell lymphoma Angioimmunoblastic T-cell lymphoma (AITL) Anaplastic large cell lymphoma, ALK-positive Anaplastic large cell lymphoma, ALK-negative Peripheral T-cell lymphoma, NOS Primary cutaneous anaplastic large cell Lymphomatoid papulosis Borderline lesions Subcutaneous panniculitis-like T-cell Primary cutaneous gamma-delta T-cell Hydroa vacciniforme lymphoma Primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell Primary cutaneous small/medium CD4+ Tcell lymphoma (provisional) Use of Term PTCL Peripheral T-cell lymphoma is a mature T-cell lymphoma Cutaneous T-cell lymphoma: Largely (but not always) indolent Peripheral T-cell lymphoma::Mostly aggressive, in general poor prognosis with a few exceptions Peripheral T-cell lymphoma-NOS: Most common subtype of PTCL NOS = not otherwise specified Peripheral T-cell Lymphomas, PTCL refers to mature T-cell lymphomas (Pathology Definition) PTCL “Systemic T-cell Lymphoma” Peripheral T-cell lymphoma NOS “CTCL” Angioimmunoblastic T-cell lymphoma Mycosis Fungoides Sezary syndrome Subcutaneous panniculitis-like Primary cutaneous ALCL Lymphomatoid papulosis Primary cutaneous small/medium CD4+ Tcell lymphoma Primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma Anaplastic Large Cell-ALK-1 negative Anaplastic Large Cell-ALK-1 positive Enteropathy-type intestinal lymphoma Extranodal NK/T-cell lymphoma-nasal Adult T-cell leukemia/lymphoma Hepatosplenic T-cell lymphoma (may be derived from an immature T-cell) Cancers of Immature T-cells lymphoblastic lymphoma and acute lymphoblastic leukemia Peripheral T-cell Lymphomas, PTCL refers to usually aggressive systemic T-cell lymphomas (Clinical Definition) “Usually Aggressive Systemic Tcell Lymphoma (PTCL)” Peripheral T-cell lymphoma NOS* Angioimmunoblastic T-cell lymphoma* Anaplastic Large Cell-ALK-1 negative* Anaplastic Large Cell-ALK-1 positive Enteropathy-type intestinal lymphoma Extranodal NK/T-cell lymphoma-nasal* Adult T-cell leukemia/lymphoma* “Aggressive CTCL” “Usually Indolent CTCL” Mycosis Fungoides Primary cutaneous aggressive Sezary syndrome epidermotropic CD8+ Subcutaneous panniculitis-like cytotoxic T-cell lymphoma Primary cutaneous ALCL Lymphomatoid papulosis Primary cutaneous small/medium CD4+ T-cell lymphoma Hepatosplenic T-cell lymphoma (may be derived from an immature T-cell) *skin lesions are common in these entities Cancers of Immature T-cells lymphoblastic lymphoma and acute lymphoblastic leukemia Expert Agreement: Consensus Diagnosis Subtype Agreement Subtype ALCL, ALK+ 97% PTCL, unspecified 75% ATLL 93% Panniculitis-like 75% Nasal NK/T-cell 92% ALCL, ALK- 74% Angioimmunoblastic 81% Hepatosplenic 72% Enteropathy-type 79% Cutaneous ALCL 66% ALCL = anaplastic large-cell lymphoma ATLL = adult T-cell leukemia/lymphoma Vose J, et al. J Clin Oncol. 2008;26:4124-4130. Agreement International PTCL Study Major NHL Types by Region Percent North America Europe Asia PTCL, unspecified 34.4 34.3 22.4 Angioimmunoblastic 16.0 28.7 17.9 Anaplastic, ALK+ 16.0 6.4 3.2 Anaplastic, ALK- 7.8 9.4 2.6 NK/T-cell 5.1 4.3 22.4 ATLL 2.0 1.0 25.0 Vose J, et al. J Clin Oncol. 2008;26:4124-4130. Prognosis: Overall and Failure-free Survival 1.0 Peripheral T-cell Lymphoma-NOS Proportion 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 1 2 3 4 5 6 7 8 9 10 Time Vose J, et al. J Clin Oncol. 2008;26:4124-4130. 11 12 13 14 15 16 17 18 Mature T and NK Lymphomas: FFS of Different Histologies 1.0 0.9 Proportion 0.8 ALCL ALK+ 0.7 0.6 0.5 0.4 ALCL ALK- 0.3 AITL 0.2 PTCL NK/T-nasal type EATCL 0.1 ATLL 0.0 0 1 2 3 4 5 6 7 8 9 10 Time . Vose J, et al. J Clin Oncol. 2008;26:4124-4130. 11 12 Prognosis in Mycosis Fungoides and Sezary Syndrome Disease-Specific Survival by Stage Kim YH, et al. Arch Dermatol. 2003;139:857-866. Risk of Progression by Stage ISCL/EORTC Revisions to the Classification and Staging of Mycosis Fungoides and Sezary Syndrome T (Skin) T1 Limited patch/plaque (< 10% of total skin surface) T2 Generalized patch/plaque (> 10% of total skin surface) T3 Tumors T4 Generalized erythroderma M (Viscera) N (Nodes) N0 No clinically abnormal LNs N1 Clinically abnormal LNs; histopath Dutch Gr 1 or NCI LN0-2 (clone +/-) N2 Clinically abnormal LNs; histopath Dutch Gr 2 or NCI LN3 (clone +/-) N3 Clinically abnormal LNs; histopath Dutch Gr 3-4 or NCI LN4 (clone +/-) Nx Clinically abnormal LNs, no histo info B (Blood) M0 No visceral involvement B0 No significant blood involvement M1 Visceral involvement B1 Low blood tumor burden B2 High blood tumor burden Olsen E, et al. Blood . 2007;110:1713-1722. Spectrum of CD30-Positive Cutaneous Lymphoproliferative Disorders Lymphomatoid papulosis (ALK-) Primary cutaneous ALCL (usually ALK-) Systemic ALCL with skin involvement (ALK+/-) All CD30+ and rearranged TCR genes Primary Cutaneous ALCL 1.0 0.9 0.8 Proportion 0.7 0.6 ALCL, ALK+ 0.5 0.4 ALCL, ALK- 0.3 0.2 0.1 Transformed MF PTCL-NOS 0.0 0 1 2 3 4 5 6 7 8 9 10 11 12 Time PTCL, if CD30+ in > 80% of cells-worse prognosis HTLV-1/ATLL may be CD30+ MF with large cell transformation will be CD30+ Vose J, et al. J Clin Oncol. 2008;26:4124-4130. . 13 14 Case Study A 68-year-old woman presents with swollen cervical lymph nodes Other complaints include low-grade fever and fatigue The only abnormal physical finding was the presence of prominent palpable cervical, axillary, and groin lymph nodes She is prescribed a course of antibiotics Case Study Patient returns reporting no improvement following antibiotic treatment Excision of a left cervical lymph node showed marked proliferation of carbonizing vessels and a diffuse infiltrate of T-cells that was: CD4 positive CD20 positive CD10 positive CD30 weakly positive (5-10% of cells) CD2 negative ALK negative CD5 negative Polling Question 1 The most likely diagnosis is? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. Case Study PET/CT shows diffuse lymphadenopathy (LAN) Bone marrow biopsy shows small T-cells similar to those seen in the nodes Multiple chemistry panels were all normal except LDH 414 U/L; ECOG Performance Status is 1 Prognostic scores: – International Prognostic Index (IPI) score (age, stage, LDH) and Prognostic Index for PTCLU (PIT) score (age, LDH, marrow) are 3 Polling Question 2 What is her estimated 5-year OS with standard-dose CHOP? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. Polling Question 3 She is otherwise healthy and has a left ventricular ejection fraction of 60%. Which of the following is true about initial therapy for her? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. Treatment and Prognosis of Mature T-cell and NK-cell Lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin’s Lymphoma Study Group (DSHNHL) • 7 DSHNHL trials enrolling 343 patients • Most received 6-8 courses of CHOP or CHOEP (Hi-CHOEP, or MegaCHOEP) • 56% ALCL, 8% AITL Histology N 3-yr EFS 3-yr OS ALCL, ALK+ 78 75.8% 89.8% ALCL, ALK- 113 45.7% 62.1% PTCLU 70 41.1% 53.9% AITL 28 50.0% 67.5% Schmitz N, et al. Blood. 2010;116:3418-3425. Treatment and Prognosis of Mature T-cell and NK-cell Lymphoma: Event-free survival Younger patients treated on NHL-B1/Hi-CHOEP trial EFS ALCL, ALK+ Schmitz N, et al. Blood. 2010;116:3418-3425. EFS Other subtypes Autologous stem cell transplantation as first-line therapy in PTCL: Results of a prospective multicenter study N=83 CHOP x 4-6 IF CR/PR mobilized with DexaBEAM or ESHAP PTCL 39% AITL 33% ALCL 16% Med age 46.5 (30-65) AA-IPI L-LI 49% HI-H 51% TBI + CY-ASCT Median F/U: 33 months CR/CHOP 39% PR/CHOP 40% Reimer P, et al. J Clin Oncol. 2009;27:106-113. ASCT 66% POD 29% (22% CHOP) Autologous stem cell transplantation as firstline therapy in PTCL: Survival Disease-free survival53% 3-year DFS: 1 1 0,8 0,8 DFS probability Survival probability Overall survival 3-year OS: 48% 0,6 0,4 0,2 0,6 0,4 0,2 0 0 0 12 24 36 48 Time (months) Time (months) (n=83) (n=83) Reimer P, et al. J Clin Oncol. 2009;27:106-113. 60 0 12 24 36 48 Time (months) (n=55) (n=83) Time (months) 60 Case Study She is treated with CHOP followed by HDTASCT and is in remission for 2 years A follow-up CT scan shows new inguinal lymphadenopathy up to 3 cm Biopsy shows recurrent AITL She is now 70 years old She is having mild fatigue and again develops low-grade fevers You discuss therapeutics options at this time Polling Question 4 What do you recommend? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. PROPEL Pivotal Trial: Pralatrexate in Relapsed/Refractory PTCL N=115 • Single-arm • Phase II • Relapsed or refractory PTCL Pralatexate 30 mg/m² IV x 6 weeks in 7 week cycles* Primary endpoint • Response rate Secondary endpoints • Duration of response • Overall survival • Progression-free survival *No pre-medications were required and patients also received vitamin B12 every 8-10 weeks, and 1 mg of oral folic acid daily. O’Conner OA, et al. J Clin Oncol. 2011;29:1182-1189. PROPEL: Response Analysis by Subsets Number of Patients Proportion of Patients ORR Age • < 65 years • ≥ 65 years 70 39 64% 36% 27% 33% Number prior systemic regimens • 1 • 2 •≥3 23 29 57 21% 27% 52% 35% 24% 30% Prior transplant • Yes • No 18 91 17% 83% 33% 29% Histology • PTCL-NOS • AILT • ALCL • Transformed MF • Other 59 13 17 12 8 54% 12% 16% 11% 7% 32% 8% 35% 25% 38% Factor O’Conner OA, et al. J Clin Oncol. 2011;29:1182-1189. PROPEL Adverse Events ≥ Gr 3 Occurring in ≥ 3% of Patients (n=111) Adverse event Any Grade Grade 3 Grade 4 Mucosal inflammation* 70% 17% 4% Thrombocytopenia** 41% 14% 19%1 Nausea 40% 4% 0% Fatigue 36% 5% 2% Anemia** 34% 16% 2% Neutropenia** 24% 13% 7% Dyspnea 19% 7% 0% Hypokalemia** 15% 4% 1% Abnormal LFTs* 13% 5% 0% Abdominal pain 11% 4% 0% Leukopenia** 11% 3% 4% Febrile Neutropenia 5% 5% 0% Sepsis 5% 3% 2% Hypotension 5% 3% 1% *includes 6 MedDRA preferred terms **includes 2 MedDRA preferred terms ***includes 3 MedDRA preferred terms 1- Only 5 patients had platelet count < 10,000 μL O’Conner OA, et al. J Clin Oncol. 2011;29:1182-1189. Pivotal Trial of Romidepsin in Relapsed/Refractory PTCL N=131 • Single-arm • Phase II • PCTL failing ≥1 prior systemic therapy • Systemic disease Romidepsin 14 mg/m2 IV on Days 1,8,15 every 28 days T-cell lymphoma subtypes (n): PTCL-NOS (53) AITL (21) ALCL (ALK-1-neg) (16) Other (10) Primary endpoint • CR rate by independent review Secondary endpoints • CR rate by investigator assessment • ORR • Duration of response • Time to first response • Time to progression • Safety, tolerability Median age: 61 years (range, 20-83) Median of 2 prior regimens (range, 1-8) 38% refractory to most recent therapy Coiffier B, et al. J Clin Oncol. 2012;30:631-636. Romidepsin in Relapsed/Refractory PTCL ORR (by IRC): 25% (33/130) 15% CR Median duration of response: 17 months (<1 to 34.0+ months 89% of patients in CR/CRu had no disease progression after median follow-up of 13.4 months Safety profile consistent with CTCL studies – Most common grade ≥3 AEs: thrombocytopenia (24%); neutropenia (20%), and infections (19%) Coiffier B, et al. J Clin Oncol. 2012;30:631-636. IRC-Assessed PFS with Romidepsin in Relapsed/Refractory PTCL All patients: 4 months Patients in Cr/CRu: 18 months Patients in PR: 7 months Patients in SD: 6 months ©2012 by American Society of Clinical Oncology Coiffier B, et al. J Clin Oncol. 2012;30:631-636. Treatment-Related Adverse Events in ≥ 20% of Patients (N = 131) At least one TEAE Nausea Infection Fatigue Vomiting Thrombocytopenia Diarrhea Pyrexia Neutropenia Constipation Anorexia Overall Anemia Dysgeusia Events with a missing toxicity grade are included. ≥ Grade 3 Brentuximab Vedotin (SGN-35) in ALCL 3 components: – Chimeric antibody SGN-30 – Synthetic analog (MMAE) of the antitubulin agent dolastatin 10 – Stable drug linker Proposed mechanism of action – – – – Binds to CD30 Internalized into the tumor cell MMAE is released Tumor cell undergoes G2/M phase cell cycle arrest and apoptosis G2/M cell cycle arrest and apoptosis Preclinical activity observed both in vitro and in vivo ADC=antibody-drug conjugate; MMAE= monomethylauristatin E. Reproduced with permission from Seattle Genetics, Inc.; Pro. 2009 ASCO Educational Book. Alexandria, VA: American Society of Clinical Oncology. 2009;486; Younes. EHA. 2009 (abstr 0503). Brentuximab Vedotin in Relapsed/ Refractory Systemic ALCL N=58 • Single-arm • Phase II • Relapsed or refractory systemic ALCL Brentuximab vedotin 1.8 mg/kg IV every 21 days Median age: 52 years (range, 14-76) Median of 2 prior regimens (range, 1-6) 62% refractory to frontline therapy Shustov AR, et al. ASH 2010. Abstract 961. Primary endpoint • ORR by independent review Secondary endpoints • CR rate • Duration of response • PFS • OS Responses to Brentuximab Vedotin in Relapsed/ Refractory Systemic ALCL N=58 Overall response rate (95% CI) IRF 86% (75, 94) Complete remission 53% Partial remission 33% Stable disease 3% Progressive disease 5% Histologically ineligible 3% Not evaluable 2% Outcomes Median duration of OR (95% CI) 12.6 months Median duration of CR (95% CI) 13.2 months Median PFS (95% CI) 13.3 months Median OS Not reached Shustov AR, et al. ASH 2010. Abstract 961. Polling Question 5 What do you see as the greatest barriers to successful treatment of your patients with PTCL? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. Case Study A 41-year-old man presents with stage IA mycosis fungoides He is treated with topical NM He has some response but then progresses and changed to narrow-band UVB phototherapy Management of Stage IB/IIA Disease (Generalized Patch/Plaque, T2) CR rate 45-90% Therapy CR Rate ORR Mechlorethamine (HN2) 45-70% 75-90% Psoralen + ultraviolet A (PUVA) 50-80% 55-95% 1. Querfeld C, et al. Arch Dermatol. 2005;141:305-311. 2. Gathers RC, et al. J Am Acad Dermatol. 2002;47:191-197. Case Study The patient does reasonably well on/off NB-UVB for about 2 years then develops a tumor lesion on the eyelid Case Study Biopsy shows tumor but no evidence of large cell transformation (<25% large cells) No other tumors or extracutaneous disease Polling Question 6 What do you do now? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. TSEBT + Chemotherapy (cyclophos, dox, vp-16, vincristine) VS Sequential topical therapies (NM- +/- MTX- PUVA-TSEBT-Chemo) N=103 CR 38% vs 18% Conservative N=51 Stage IA-IIA 31 DFS-ND NM=51 Stage IIB 12 OS-ND MTX-16 Stage III 2 PUVA-26 Stage IV 58 TSEBT-13 Chemo-14 vs Topical therapy Percent Surviving EBRT + Chemotherapy No survival difference 100 90 80 70 60 50 40 30 20 10 0 ALL No of Total Deaths Combination 52 Conservative 51 21 19 P=.72 12 24 36 48 60 72 84 96 108 Survival (mo) Percent Surviving Low Risk (IA–IIA) Higher Risk (≥IIB) Overall survival—All pts 100 90 80 70 60 50 40 30 20 10 0 Overall survival—Advanced No of Total Deaths P=.74 12 Kaye FJ, et al. N Engl J Med. 1989;321:1784-1790. 12 12 Combination 28 Conservative 28 24 36 48 60 72 Survival (mo) 84 96 108 Selected Systemic Therapies for MF Selected Systemic Therapies for Mycosis Fungoides Agent Response Rate CR Comments 45–55% 6% ≥Stage IIB 29.5% 2% ≥Stage IIB Denileukin diftitox 36% 12% 18ug/kg Romidepsin 38% 7% ≥Stage IIB Gemcitabine 68% 8% 1000 mg/m2, 3–4 wk CAVE + TSEB 88% 31% ≥Stage IIB Pralatrexate 53% 6% Stage IIB Bexarotene Vorinostat Horwitz SM. Clin Lymphoma Myeloma. 2008;8(suppl 5):S187 Case Study He undergoes radiation local electron beam therapy followed by maintenance low-dose bexarotene Case Study He is well for 2 years but then develops new plaques that fail to respond to increased dose of bexarotene and addition of phototherapy Polling Question 7 What is your next step? Please see the multiple answer options on the right and select an answer. Once you submit your answer, your answer selection will be compared with your peers’ responses. The best answer(s) will be discussed in the subsequent slides and commentary. DISCUSSION Please click on the supplemental tab below to listen to Dr. Horwitz’s response to this case study question. Pralatrexate Response by CTCL Subtype and Stage N = 54 Optimal dose = 15 mg/m2 Response rate Rate at Optimal CTCL Subtype at ≥ 15 mg/m2 Stage Dose/Sched (per Investigator) 3/4 weeks % (n/N) % (n/N) MF All patients IB IIB III IVA IVB Overall Response Rate % (n/N) 60% (3/5) 67% (4/6) 50% (1/2) 60% (3/5) 0% (0/1) 63% (5/8) 67% (8/12) 50% (1/2) 60% (3/5) 0% (0/1) 50% (5/10) 53% (9/17) 50% (1/2) 50% (3/6) 0% (0/1) 45% (13/29) 51% (21/41) 41% (22/54) Horwitz SM, et al. Blood. 2012 Mar 6 [Epub ahead of print]. Pralatrexate for CTCL: Progression-Free Survival Cohort >15 mg/m2 N=41 Median PFS: 388 days Horwitz SM, et al. Blood. 2012 Mar 6 [Epub ahead of print]. Bendamustine in T-cell lymphoma (BENTLY Trial) N=60 • Multicenter, single-arm, phase II study • Relapsed or refractory Tcell lymphoma • ≤ 3 prior lines chemotherapy Bendamustine 120 mg/m2 IV on Days 1,2 every 3 weeks for 3 cycles T-cell lymphoma subtypes (n): AILT (24) PTCL-NOS (17) ALCL (4) EATL (1) MF (1) Damaj G, et al. 11th ICML; Lugano 2011. Abstract 126. If no PD: Additional 3 cycles bendamustine Primary endpoint • ORR (IWC 1999 criteria) Secondary endpoints • Safety, tolerability • Duration of response • PFS • OS Bendamustine in Relapsed/Refractory T-cell Lymphoma ORR: 42%; CR: 23% Median DOR: 5.5 months – Median duration of CR: 11.9 months Most common grade 3/4 adverse events: – Neutropenia (49%) – Thrombocytopenia (36%) – Infections (34%) Damaj G, et al. 11th ICML; Lugano 2011. Abstract 126. Phase II Trial: Lenalidomide in Relapsed/Refractory TCL N=24 • T-cell lymphoma (other than MF) • WHO PS ≤3 • Previously treated or untreated but not suitable for standard therapy Lenalidomide 25 mg PO QD on days 1-21 of each 28-day cycle Until disease progression, death, or unacceptable toxicity MF=mycosis fungoides. Dueck G, et al. Cancer. 2010;116:4541-4548. Primary endpoint • ORR Secondary endpoints • PFS • OS • Safety Lenalidomide in Relapsed/Refractory TCL ORR=30% (7/23) Median PFS = 96 days Median OS = 241 days (range, 8-696+ days) Common AEs – Grade 4: thrombocytopenia (33%) – Grade 3: neutropenia (20.8%), febrile neutropenia (16.7%), pain NOS (16.7%) Histology No. CR PR ORR, % ALCL 5 0 2 40 AITL 7 0 2 29 EATCL 1 0 0 0 HSTCL 1 0 0 0 PTCL 9 0 3 33 Dueck G, et al. Cancer. 2010;116:4541-4548. Phase II Trial of Belinostat in Relapsed/Refractory T-Cell Lymphomas CR/PR/SD Belinostat 1000 mg/m2, IV days 1-5, q 21 days x 2 cycles PODPD Outcome Response ORR Stable disease Median response duration Grade 3/4 adverse events Grade 2 QTcF Prolongation Belinostat up to 6 more cycles or until PD Off study CTCL PTCL (N = 21) (N = 29) (n = 19) (n = 29) 6 (32%) 4(14%) 4 18 268+ days 273 days pruritis, cytopenias (4-6%) 7 Pohlman et al. ASH 2009; abstract 920 Pohlman B, et al. ASH 2009. Abstract 920. Pivotal Trial >100 pts is accrued, awaiting data (Early 2012) Aurora Kinase Inhibitor Alisertib (MLN8237) in Aggressive B-cell, T-cell NHL Relapsed/refractory, aggressive B-cell or Tcell NHL (N=48) Alisertib 50 mg PO BID x 7 days in 21-day cycles Multicenter, phase II trial Median age: 67 years (range, 32-85) T-cell lymphoma: 17% Median number prior regimens: 3 Friedberg JW, et al. ASH 2011. Abstract 95. Efficacy of Alisertib by Histology Category Response (PR+CR) n (%) B-cell lymphoma DLBCL 3 (20%) Mantle cell lymphoma 3 (23%) Transformed follicular 2 (40%) Burkitt lymphoma 1 (100%) T-cell lymphoma (PTCL) 4 (57%) Friedberg JW, et al. ASH 2011. Abstract 95. Common Serious Adverse Events with Alisertib Patients (N = 48) Event Number Percent Neutropenia* 30 65 Thrombocytopenia 15 31 Stomatitis 7 15 Fatigue 3 6 *7 cases of febrile neutropenia • Four patients died on study during cycle 1: – 2 of progressive DLBCL – 1 of sepsis on day 14 (DLBCL) – 1 of likely cardiac arrest—cause unknown (T-cell NHL) Friedberg JW, et al. ASH 2011. Abstract 95. Phase II Study of SMILE Chemotherapy in Extranodal NK/T-cell Lymphoma, Nasal Type • SMILE = Steroid (dexamethasone), Methotrexate, Ifosfamide, L-asparaginase, Etoposide • Patients with newly diagnosed stage IV or relapsed/refractory ENKL (N=38) ORR 79%; CR 45% after 2 cycles 1-year OS: 55% Highly myelosuppressive – Grade 3/4 neutropenia: 8%/92% – Grade 3/4 infection: 61% – Lymphocyte count ≥ 500/mm3 added to eligibility criteria after first 2 patients died from infection Yamaguchi M, et al. J Clin Oncol. 2011;29:4410-4416. Can we move new therapies upfront to change standard treatment paradigms? •Incorporating new therapies •Adding to existing regimens may be limited (very active single agent) •Otherwise novel approaches •Novel ways to incorporate new drugs-can be done now •Completely novel regimens-will take time CHOP New Drug Combination SGN-35 or similar New Drug New Drug Etc. Alternating or Maintenance Supplemental Information Please click on the Supplemental Tab below to view case study photos provided by Dr. Horwitz.