Chronic Aortic Regurgitation
advertisement

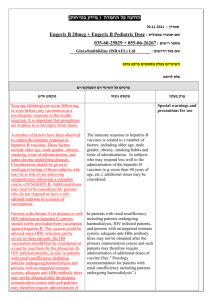
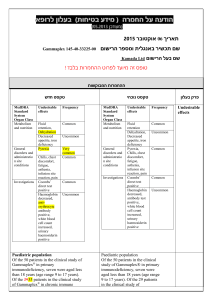
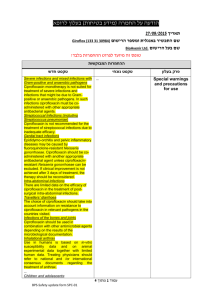
Aortic Regurgitation 2007 Chronic Aortic Regurgitation Definition • Failure of aortic leaflet cooptation in diastole Chronic Aortic Regurgitation - Etiology • Cusps Disease • Aortic Root Disease Chronic Aortic Regurgitation - Etiology Cusps Disease • Endocarditis • Bicuspid AV (10% pure AR). • Rheumatic Heart Disease (usually with MV disease but sometimes can be the dominant lesion). • Calcification of cusps (Degenerative). Chronic Aortic Regurgitation - BAV Chronic Aortic Regurgitation - Etiology Aortic Root Disease • Atherosclerosis • Marfan’s syndrome (dilatation of sinotubular ridge lifts the cusps). • Aortic dissection. • Syphilitic aortitis. • Ankylosis spondilitis. • Systemic lupus. Chronic Aortic Regurgitation Aortic Regurgitation Aortic Regurgitation - Pathophysiology • Initially chronic AR leads to a small increase in LV end diastolic volume and a small increase in stroke volume. • Large regurgitant volume increases LV end diastolic pressure (pulmonary congestion). • If developed slowly, AR enters a chronic phase of eccentric hypertrophy and progressive LV dilatation and increased stroke volume (pulse pressure) a combined pressure and volume overload), and may remain compensated for many years till LV dysfunction eventually develops. Aortic Regurgitation - Pathophysiology • In AR there is not only volume overload but also an increase in afterload and systolic wall stress. • This distinguishes AR from mitral regurgitation where systolic wall stress is normal or even low, since the regurgitant blood is ejected into the low pressure left atrium. • Thus valve surgery in MR usually results in an increase in afterload and commonly in worsening of the LV ejection fraction, correction of AR results in a decrease in afterload and frequently an improvement of the ejection fraction. Post op, if performed on time remodeling occur and LV dimensions become smaller, without LV dysfunction.. Aortic Regurgitation Chronic Aortic Regurgitation – Clinical Symptoms Congestive Heart Failure • After a long compensated phase (many years), LV decompensation proceeds symptoms of dyspnea, orthopnea and peripheral edema . Angina • Diastolic hypotension can impair coronary flow. • Increase demand on coronary flow d/t increased LV mass. • Less common than in aortic stenosis. Chronic Aortic Regurgitation – Physical Findings • Bounding pulses (chronic AR). • Diastolic decrescendo murmur (length correlates with severity when LV function is good) in left sternal border. • Systolic murmur due to relative aortic stenosis. • Mitral rumble (Austin Flint murmur), jet impinging the mitral valve. • Systolic hypertension and wide pulse pressure (mod-sev AR). • Signs become less apparent with decompensation and S3 appears. Chronic Aortic Regurgitation - Signs Signs of aortic insufficiency Sign Finding Corrigan’s pulse Rapid forceful carotid upstroke followed by rapid decline Quincke’s sign Systolic plethora and diastolic blanching in nail bed when nail is slightly compressed De Musset’s sign Bobbing of head Duroziez’s sign Systolic and diastolic bruit heard over femoral artery when compressed by bell of stethoscope Hill’s sign Augmentation of systolic blood pressure in the arm by 30 mmHg compared to the leg Chronic Aortic Regurgitation - Echocardiography • LV size and function , aortic root and cusps motion. • Typical cusps morphology in different etiologies. • Color Doppler interrogation of regurgitant flow in LVOT, jet width to estimate severity (semi quantitative). • Descending aortic flow reversal in the aorta in diastole. • Pressure half time of aortic regurgitant flow, more rapid in severe cases. • When echocardiography is not available or clear MRI is an alternative for assessment of valve morphology and flow, and LV function and nuclear angiography can be used for serial assessment of LV function. Chronic Aortic Regurgitation Chronic Aortic Regurgitation Chronic Aortic Regurgitation Echocardiographic Criteria of Severity of Aortic Regurgitation (color flow jet width) Severity Jet / LVOT Jet width (vena contracta) Mild <25% < 3 mm Moderate 25%-65% 3-6 mm Severe >65% > 6 mm Chronic Aortic Regurgitation Chronic Aortic Regurgitation – Cardiac Catheterization • For controversial cases and patients above 40 and those with risk factors with suspected coronary artery disease. • Aortography visualizes flow of contrast media (not velocities like echocardiography), the denser the ventricle opacification the worse is the regurgitation. Chronic Aortic Regurgitation - Management Exercise Testing • Assessment of functional capacity and symptomatic response when with history of equivocal symptoms. • Before participation in athletic activities • For prognostic assessment before AVR in patients with LV dysfunction. Chronic Aortic Regurgitation - Management • A diminished LV ejection fraction (below 50– 55%) is associated with reduced prognosis even in asymptomatic patients (A). • LV enlargement in and of itself also constitutes an indication for surgery (B). Chronic Aortic Regurgitation - Management Surgery Recomended • After symptoms and before dysfunction is irreversible. • With evidence of contractile dysfunction even if asymptomatic. Ecocardiographic Criteria for surgery with Severe AR • Simple measures of contractility: shortening fraction (<27%) and ejection fraction (<55%). • LV end systolic diameter (>5.0 cm). • LV end-systolic volume >55 mL/m2 • A window of 18 months is available once those limits are crossed. Repeat measures (LVEDD <4.0 – 2 y, 4.0-5.0 1 y, >5.0 – 6 m). Chronic Aortic Regurgitation - Management • The overall operative mortality for isolated AVR is about 4.3%. • In patients with marked cardiac enlargement and prolonged LV dysfunction experience an operative mortality rate of approximately 10% and a late mortality rate of approximately 5% per year due to LV failure despite a technically satisfactory operation. • Because of the very poor prognosis with medical management, even patients with LV failure should be considered for operation. Chronic Aortic Regurgitation - Management AV replacement (with/without root replacement) AV repair: (annular dilatation, valve perforation, non calcified leaflets with prolapse) Medical Therapy • Vasodilators; Nifedipine, hydralazine, ACE inhibitors are used to delay progression of AR in asymptomatic patients. (more compelling data is available with nifedipine). Chronic Aortic Regurgitation Acute Aortic Regurgitation Background • Medical emergency (mortality 75% with medical therapy, 25% with surgery). Etiology • Endocarditis • Aortic dissection • Trauma Aortic Regurgitation - Diagnosis Echocardiography • • • • Early closure of mitral valve. Diastolic mitral regurgitation. Vegetation, intimal tear. Consider TEE (for vegetations, abscess, aortic dissection). Management • Blood culture, antibiotics, vasodilators • AVR (10% risk of reinfection). Aortic Regurgitation - Guidelines AHA ACC 2006 European 2007 ARקשה ,חולים סימפטומטים דרגה תפקודית 2-4 I I ARקשה ופגיעה בחדר שמאל )(LVEF<50% I I ARקשה ,מתוכנן ניתוח /CABGמסתם אחר/האורטה העולה I I IIa LV>75/55 IIb IIa LV>70/50 - ARקשה ,חולים אסימפטומטים עם LVEF מעל ,50%חדר מאד מורחב ARקשה ,חולים אסימפטומטים עם LVEF מעל ,50%חדר מורחב במידה בינונית ( 70-75/50-55מ"מ) Aortic Regurgitation - Guidelines קוטר האורטה העולה European AHA ACC 2007 2006 ARבכל דרגה ,האורטה מורחבת: מרפאן 45מ"מ מסתם דו-עלי 50מ"מ שאר המסתמים < 55מ"מ מעל 50ממ בכל האטיולוגיות I IIa IIa NATURAL HISTORY OF AORTIC REGURGITATION Asymptomatic patients with normal LV systolic function: • Progression to symptoms and/or LV dysfunction <6%/yr • Progression to asymptomatic LV dysfunction <3.5%/yr • Sudden death <0.2%/yr Asymptomatic patients with LV systolic dysfunction: • Progression to cardiac symptoms >25%/yr Symptomatic patients: • Mortality rate >10%/yr LV = left ventricular. From Bonow RO, Carabello B, de Leon AC Jr, et al: ACC/AHA Guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol 32:1486, 1998.