Laboratory Rounds Is this a Septic Joint?
advertisement
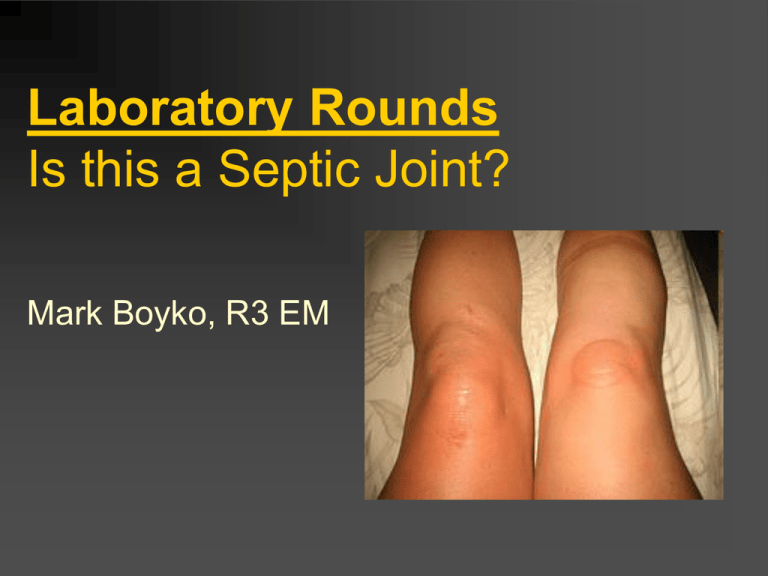
Laboratory Rounds Is this a Septic Joint? Mark Boyko, R3 EM Case 53 yo female comes in with 2 day history of increasing R knee pain, now giving her a limp. Does not recall injuring it That knee is always ‘a little sore’ from running injuries years ago Case PMHx: HTN GERD Smoker Gout (toes, L ankle) – hasn’t had a flare in years Meds Allopurinol Ramipril Ranitidine Case Phx No fever, normal vitals Knee looks swollen, no cellultis Joint warm, ROM is painful but patient can do it Labs Serum WBC 14 ESR 32 CRP 17 Uric Acid 400 Synovial Fluid WBC 36 x109/L, PMN’s 65% Low glucose Negative for crystals Labs Gram Stain Negative What do you want to do?? Overview Value of serum labs Value of synovial fluid analysis Gram’s Stain & Cultures Prosethetic Joints Course of Action for Dry Taps Review – The Swollen Joint Non-inflammatory Trauma OA Inflammatory RA Crystal arthropathies Seronegative arthropathies Septic joint Why is this Important? Joint destruction can occur within 2-3 days if untreated infection Patients can become systemically septic from a joint infection rather easily We need to make decisions before cultures come back We Love Prediction Tools Can anything help us rule this out?? Serum Labs Serum WBC >10 x 109/L sensitivity of 50% for infection LR 1.4 Many sterile but inflammatory joints give elevated serum WBC Bottom Line: Not sensitive Serum Labs Serum ESR ‘Elevation’ in most studies >30 mm/h Sensitive but not specific LR 1.3 Bottom Line: Only useful to track resolution of the infection over time Serum Labs Serum CRP ‘Elevated’ in most studies >100 mg/L Sensitivity 75%, poor specificity LR 1.6 Bottom Line: Although CRP shows promise, there is insufficient evidence for its sensitivity to be high enough to rule out septic arthritis. -Best Bets 2008 Synovial Fluid What’s Normal? Normal knee has avg 4cc synovial fluid Normal synovial WBC <0.2x109/L Glucose same as plasma Uric Acid same as plasma Protein <25% of plasma Synovial Fluid Normal – amber, transparent Synovial Fluid Inflammatory Cells - opaque Synovial Fluid Hemarthrosis Hemarthrosis Trauma #1 cause Anticoagulation therapy Hemophilia Synovioma Rarely, infection and hemarthrosis coexist. If concerned, send for culture. Synovial Fluid Findings Normal Non-Inflamm Inflammatory Septic Colour Clear Yellow Yellow Yellow Clarity Transparent Transparent Opaque Opaque WBC (x109/L) <0.2 0.2 - 2 2 - 150 20 - 200 PMN’s <25% >50% >75% <25% Synovial Fluid Glucose and Protein Synovial / Serum Glucose <0.5-0.75, low sensitivity Synovial Glucose <1.5 mmol/L sensitivity 38-64% Synovial Protein >25% of plasma, low sensitivity Bottom Line: Glucose and Protein levels have no role in the work up of a septic joint Synovial Fluid LDH Lactic Acid >250 U/L was 100% sensitive in retrospective study on 8 confirmed cases, prospectively was not as strong 90-97% NPV, but low powered studies Bottom Line: Insufficient data to date Synovial Fluid Tumour Necrosis Factor – α Jeng et al, Am J Emerg Med 1997 Prospective, n=75 Synovial TNF-α >36.2 pg/mL sens 95%, spec 50% for bacterial infection Bottom Line: Needs more study before routine order Synovial Fluid WBC <25 LR 0.32 >25 LR 2.9 >50 LR 7.7 >100 LR 28.0 Margeretten et al, JAMA 2007 Synovial Fluid 30% of immunocompetent people with culture confirmed septic joint have synovial WBC <50 - McGillicuddy et al, Am J Emerg Med. 2007 50% of immunocompromised people with culture confirmed joint infection had WBC <28 -McCutchan et al, Clin Orthop Relat Res 1990 Synovial Fluid PMN’s <90% LR 0.34 >90% LR 3.4 Margeretten et al, JAMA 2007 Synovial Fluid WBC Bottom Line Cut-off of 50 x109 /L too insensitive rule-out infection Use in clinical context The diagnostic cut-off that maximized the sensitivity / specificity was a synovial WBC count of 17.5 x109/L (Sens 83%, Spec 67%) - Li et al, Emerg Med J 2007 Synovial Fluid Eosinophilia Parasitic infection Allergy Fungal Neoplasm Lyme disease Combined Value? Li et al, Emerg Med J 2007 Retrospective chart review 156 patients Combined Sensitivity 100% if: Serum WBC <11 Serum ESR <20 Synovial WBC <50 Bottom Line: Not powered enough, not prospectively validated, cannot use to rule out septic joint Synovial Fluid Crystals Gout - Monosodium Urate, 90% sensitive, LR 14 Pseudogout – PPDC, 80% sensitive, LR 2.6 Cholesterol crystals – seen in chronic inflammatory conditions Crystals & Infection Crystals do not rule out infection! Retrospective study n=265 patients with crystals, 1.5% had septic joint -Shah et al, J of Emerg Med 2007 Literature ranges from 1-20% of infectious joints co-exist with crystals Microbio Review ALL AGES: #1 cause still Staph Aureus <30, sexually active: Neisseria Gonorrhea Elderly: Gram Negatives Prosthetics: Careful of Pseudomonas Gram’s Stain Guides your antibiotic therapy while awaiting cultures Need roughly 3-5cc for stain & culture Only 65% sensitive for non-gonococcal infections Only 25% sensitive for gonococcal infections Bottom Line: A negative Gram stain means nothing. A positive Gram stain means you should start treatment. Cultures ‘Gold standard’ ? Gonococcus difficult to culture Negative 50% of the time Requires chocolate agar Non-gonococcus will culture 90% of time If you only have enough fluid for one test, this is what you do Blood cultures reveal pathogen 25-50% of the time Gonococcal Arthritis Synovial WBC often <50 Gram stain Positive only 25% of the time Culture Positive only 50% of the time If you suspect it, culture at 3 mucosal sites (pharynx, genitals, anus) will increase your chance of positive culture to 80% Generally less destructive to the joint versus other pathogens Gram Stain Positive, Culture Negative In reality, this is retrospective Go with your Gram Stain treat these patients while awaiting cultures How does this happen? Antibiotics already on board Organism difficult to culture Was infected, now clearing Prosthetic Joints <3mos since surgery likely Staph Epiderm >3mos since surgery Staph, Strep, Gram Neg Should always call Ortho before tapping these in ER Prosthetic Joints Trampuz et al, Amer J of Med 2004 Prospective, n=133, 34 had septic joint Synovial WBC >1.7 x109/L , sens 94% spec 88% Synovial PMN’s >65%, sens 97% spec 98% Mason et al, J of Arthroplasty 2003 Retrospective n=86 knees Ideal sensitivity 98% for synovial WBC 2.5 x109/L and PMN’s 60% What About Those Dry Taps? Dry Tap? Makes a septic joint unlikely usually a large enough effusion for tap, but never been validated Options U/S guided in the department Consult Ortho Fluoroscopy guided BOTTOM LINE: You need a sample of that fluid if you are worried about infection Hot Joint, No Organism Fastidious organism Antibiotics begun before cultures sent Wrong Diagnosis Help increase your yield? Use blood culture bottles for synovial fluid (aerobic and anaerobic) - Joint, Bone, Spine 2006 Relevance to Pediatrics? No good studies specifically on synovial fluid analysis in the pediatric population Most use numbers from adult data How Many Use Kocher’s Criteria? Kocher et al, J of Bone Joint Surg 2004 TAKE HOME MESSAGE Cannot rely on serum values to rule out septic joint If you believe there’s an effusion, get that fluid somehow Unfortunately, nothing has a strong NPV TAKE HOME MESSAGE Synovial fluid: WBC & PMN is helpful WBC <18 is low risk but not zero WBC >50 is high likelihood PMN’S >90% is high likelihood Glucose, Protein useless TAKE HOME MESSAGE ‘Gold Standard’ is clinical suspicion of an experienced physician, not laboratory tests (Current Opinion Rheumatology 2008) Prosthetic Joints Lower WBC & PMN threshold Don’t feel bad - 30% of the time reason for effusion remains ‘unknown’ Thanks Feel free to ask for any references