Neoadjuvant Therapy For Rectal Cancer:
Mature Results From NSABP Protocol R-04
A Collaborative National NCI Protocol Conducted by
NSABP, NCCTG, ECOG, CALGB, and SWOG
CJ Allegra, G Yothers, MJ O’Connell, MS Roh, RW Beart,
NJ Petrelli, S Lopa, S Sharif, and N Wolmark
Disclosures
• I have no relevant conflicts of interest to disclose
Goals of NSABP R-04
• Designed at the start of the millennium to address the questions:
– Can the oral fluoropyrimidine, capecitabine be substituted for the standard
of care in the curative setting of Stage II & III rectal cancer namely, CIV 5-FU,
during neoadjuvant RT?
• CIV 5-FU became the SoC based on a US cooperative group study (O’Connell et al; NEJM
August, 1994) showing superiority over bolus administrations of 5-FU
• Capecitabine was shown to be non-inferior to 5-FU in the palliative & adjuvant colon
settings and does not require a central venous catheter or infusion pump
• Small retrospective studies support similar outcomes with 5-FU and capecitabine in the
rectal neoadjuvant setting
– Can the addition of oxaliplatin enhance the activity of fluoropyrimidine
sensitized RT?
• Oxaliplatin was shown to have radiation sensitizing properties in preclinical models
• Oxaliplatin was shown to enhance the activity of 5-FU in the palliative and adjuvant colon
settings
NSABP R-04
• July, 2004
– 2-arm study comparing 5-FU and Cape
ACTIVATION
• October, 2005
AMENDMENT
– Added oxaliplatin
– 2 x 2 factorial design
– 5-FU and Cape reduced from 7 days/wk to 5 days/wk during RT
• August, 2010
CLOSED
– 1,608 accrued patients; 1595 (99.2%) Eligible
NSABP R-04
Rectal AdenoCa < 12 cm from anal verge
STRATIFICATION
Gender; Clinical Stage II/III; Intent for Type of Surgery (sphincter saving v. APR)
RANDOMIZATION
Group 1
5-FU (CIV 225mg/m2 5d/wk) +
RT (46Gy over 5 wks + boost)
Group 2
5-FU (CIV 225mg/m2 5d/wk) +
Oxaliplatin 50 mg/m2/wk X 5 + RT
Group 3
Capecitabine 825 mg/m2 PO BID + RT
Group 4
Capecitabine 825 mg/m2 PO BID +
Oxaliplatin 50 mg/m2/wk X 5 + RT
NSABP R-04
– Primary Endpoint –
• Local-regional control with 3 years minimum follow-up
– Time from randomization to first L-R failure
– Inoperable patients or those with positive margins are
considered L-R failures at the time of surgery
– Patients without documented clinical CR who do not
undergo surgery will be considered a L-R failure at the
time they should have had surgery
• “Local” – Anastomotic and pelvis
• “Regional” – Pelvic or retroperitoneal LNs at or below L5
NSABP R-04
– Secondary Endpoints –
– Rate of pathologic CR
– Number of pts undergoing sphincter-saving
surgery
– Disease free and overall survival
– Quality of Life
– Toxicity
– Correlating genetic patterns and specific tissue
biomarkers with response and prognosis
NSABP R-04
Statistical Design
• Comparison of cape and 5-FU
Comparable if 0.86 < HazRatio < 1.17
Roughly corresponds to 3yr L-R rate of +/- 2%
• Superiority for the addition of oxaliplatin to
fluoropyrimidines
>80% power for HazRatio = 0.59
Roughly corresponds to 4% increase in L-R 3yr rate
Patient Demographics
Regimen
# Eligible Pts
FU
461
FU+Ox
321
Cape
463
Cape+Ox
322
Total
1567
Age (%)
≤ 59
≥ 60
56
44
61
39
56
44
61
39
58
42
Gender
Male
Female
67
33
68
32
68
32
68
32
68
32
Clinical Stage
II
III
59
41
62
38
58
42
62
38
60
40
SS Surg
74
74
73
74
74
Non-SS Surg
26
26
27
26
26
NSABP R-04 pCR Rates (%)
P = 0.14
P = 0.42
* No significant fluoropyrimidine by oxaliplatin interaction
3 Year Overall & L-R Recurrences
P = 0.98
P = 0.70
P = 0.52
* No significant fluoropyrimidine by oxaliplatin interaction
P = 0.22
5 YEAR OUTCOMES (%)
P = 0.70
P = 0.34
P = 0.61
* No significant fluoropyrimidine by oxaliplatin interaction
P = 0.38
NSABP R-04
Primary Endpoint: Local-Regional Control
L/R Recurrence Free (%)
20
40
60
80
L/R Recurrence Free (%)
20
40
60
80
100
No Oxali vs. Oxali
100
5-FU vs. Cape
No Oxali 641 Pts, 81 L/R Recurrence
Oxali
643 Pts, 76 L/R Recurrence
HR = 0.94, 95% CI (0.67-1.29)
P = 0.70
0
0
5-FU 782 Pts, 95 L/R Recurrence
Cape 785 Pts, 97 L/R Recurrence
HR = 1.00, 95% CI (0.75-1.32)
P = 0.98
0
1
2
3
4
Years from Randomization
5
6
0
1
2
3
4
Years from Randomization
5
6
NSABP R-04
Overall Survival
No Oxali vs. Oxali
Alive (%)
40
60
Alive (%)
40
60
80
80
100
100
5-FU vs. Cape
No Oxali 641 Pts, 116 deaths
Oxali
643 Pts, 103 deaths
HR = 0.94, 95% CI (0.68-1.16)
P = 0.38
0
0
20
20
5-FU 782 Pts, 141 deaths
Cape 785 Pts, 138 deaths
HR = 1.00, 95% CI (0.74-1.19)
P = 0.61
0
1
2
3
4
Years from Randomization
5
6
0
1
2
3
4
Years from Randomization
5
6
Treatment Compliance
• At least 80% of treatment completed per
protocol
–FU – 90% alone; 84% with Oxali
–Cap – 97% alone; 96% with Oxali
–Oxali – 69% with FU; 62% with Cap
–RT – 96-98% depending on the arm
NSABP R-04 Mortality &
Adverse Events (%)
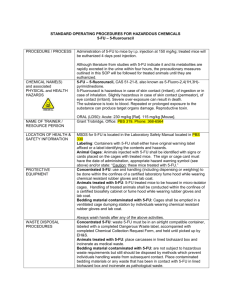
Toxicity (Grade)
5-FU
Capecitabine
5-FU +
Oxaliplatin
Overall (3+)
26.5
30.1
39.9
42.2
7
7
16
16
0.3
1.3
0.3
1.6
Diarrhea (3/4)
Death (5)
Capecitabine
+ Oxaliplatin
NSABP R-04 Summary
• Capecitabine with preop RT achieved rates similar to CIV 5-FU for:
– L-R Failure – Primary Endpoint
– pCR
– DFS
– OS
• Oxaliplatin did not improve outcomes but added significant toxicity
(diarrhea) and is therefore not indicated in combination with RT in the preop
rectal setting
• Establishes capecitabine as a standard of care in the preop rectal setting
• NSABP R-04 supports pCR & neoadjuvant rectal cancer (NAR) score as
surrogates for overall survival (Yothers G ASCO GI, 2014; Abst #384)
• Fully annotated tissue samples available for molecular studies