Chronic Apical Periodontitis: Etiology, Diagnosis, & Treatment
advertisement

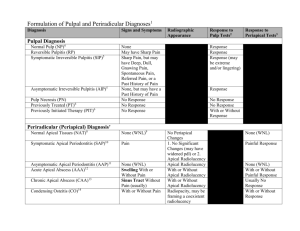
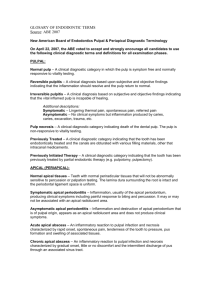
Chronic apical periodontitis ( parodontitis apicalis chronica ) Etiology, classification, clinical features, dg., diff. Dg. PERIAPICAL DISEASE Classified as: – Acute Apical Periodonitis – Acute Apical Abscess – Chronic Apical Periodontitis (Diffuse, Suppurative Apical Periodontitis with sinus tract, Apical cyst) – Condensing Osteitis Definition • The fundamental lesion of chronic periapical inflammation is known as ´´chronic apical periodontitis´´ • While this designation is the preferred one, most dentists know it by the term ´´dental granuloma´´ • The lesion is not a granuloma at all because it is not composed of granulomatous chronic inflammation. Etiology • The etiology of apical periodontitis is an infection of the tissues in the root canal system and of the surrounding dentin, in some cases also of tissues outside the apical foramen or other portals of entry • Typically,the lesion is located at the root apex, but communications may exist at various levels along the root surface,and lesions may develop at lateral and furcal locations • One or more of the clinical symptoms pain, swelling, redness, increased temperature and impaired function»characterize acute apical periodontitis. • Chronic apical periodontitis shows replacement of adjacent tissue with an inflammatory cell infiltrate. Due to the encasement of the root in bone and the relatively greater resistance of the root to resorption, the production of an inflammatory infiltrate usually occurs at the expense of the surrounding bone. • The changes in mineralization and structure of the bone adjacent to the site of inflammation form the basis of radiographic diagnostic procedures for the detection and monitoring of chronic apical periodontitis • Apical periodontitis develops as a response to infection and in the chronic form a granuloma is formed with characteristics peculiar to the location and anatomy. • In addition to the inflammatory cells, it typically contains fibrous tissue and often cholesterol crystals, as well as proliferating strands of epithelium derived from the cells of Malassez. It may or may not develop a cyst cavity, which is lined in part or in full by epithelium. If the lumen of this radicular cyst is continuous with the infectious source at the pulpal entry, it may not be self-sustained (a ‘bay’ or ‘pocket’ cyst) and will heal following elimination of the infectious source. • On the other hand, if the cyst is completely encased by epithelium and removed from the source of infection, it may be self-sustained (a‘true’ cyst) and refractory to treatment except by surgical excision. • The stages in development and also in healing of chronic apical periodontitis, granulomas and cyst are to a degree, reflected by changes in the radiographic appearance of the periapical area • These changes are of decisive importance in diagnosis and choice of treatment. Chronic apical periodontitis • The lesion is present over long time of periode • Mild state of symptoms • Histologic picture of chronic inflammation Classification • 1) Diffuse type: - small, recurrent amount of tissue damage - cellular infilltration with lymphocytes, plasma cells, phagocytic mononuclear cells, fibroblasts which produce granulation tissues for repair of damaged area GRANULOMA: formation of large nodule of granulation tissue that is slowly increase in size Resorption of hard tissue, granulation tissue around apex (outlined by capsule of fibrous tissue) • 2) Chronic suppurative periodontitis - central cavity which is accompanied with fistula and stroma - its known as chronic apical abscess ( chronic alveolar abscess) • 3) Apical cyst - true cyst: pathologic cavity which contain fluid or semi-fluid substance that is lined by epithelium and surrounded by connective tissue capsule Clinical features • CAP is generally without symptoms that may stay in the mouth with no-pain untill its revealed by x-ray • The patient may rarely complain symptoms, slight pain, some amount of swelling, a sinus may be found in buccal sulcus or in skin ( fistula ) mucosa over swelling may be bluish. • CAP is usually associated with long standing restorations such as prosthetic crowns, extensive bridge work, composite or amalgam filling Diagnosis • • • • History Vitality test – no response of pulp Percussion- slightly tender to percussion X-ray – diffuse or demarcated radiolucency around the apex of the tooth, root resorption, loss of bone, granuloma or cyst→ with sclerotic margin to the bone Diff. Dg. • Chronic Pulpitis Case 1,fig.1a 21-years old woman-non successful endodontic treatment tooth N.22,apical clear radiolucency confirming an established lesion bigger than 3mm,it shows features of lamina dura disruption and bone structural changes Case 1,fig.1b Measurement of the tooth canal length Case 1,fig.1c Final endodontic treatment Foredent and gutapercha Case 1,fig.1d 5 months after the endodontic treatment without any surgical procedure,intraoral x-ray shows chronic apical periodontitis, partial restitution of the periapical region Case 2,fig.2a Orthopantogram image,unsuccessful endodontic treatment d.N.22, Cystis radicularis D.N.22 Case 2,fig.2b Intraoral image D.22-Cystis radicularis processus alveolaris maxillae reg.frontalis purulenta Case 2,fig.2c 3months after the therapyCystectomio sec.PARTSCH II. et resectio apicis dentis N.22 Retrograde root canal endodontic therapy with amalgam Egalisatio,suturae Fig.B Granuloma periapicalis and infection transmission paths Chronic apical periodontitis. Extensive tissue destruction in the periapical region of a mandibular first molar occurred as a result of pulpal necrosis. Lack of symptoms together with presence of a radiographic lesion is diagnostic. Periapical radiolucencies associated with mandibular incisors. These teeth were vital, and a diagnosis of cemental dysplasia was made. Periodontitis chronica circumscripta d.41 Periodontitis chronica circumscripta d.14