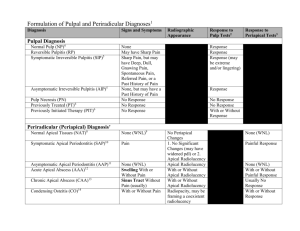
periradicular lesions
advertisement
PERIRADICULAR LESIONS of pulpal origin Definition Apical periodontitis is an inflammatory disorder of the periradicular tissue caused by a persistent microbial infection of the root canal system of the affected tooth In other words Apical periodontitis (AP) is a host response to infections by microbes and the subsequent inflammatory response Apical periodontitis includes the infection and inflammation of the lateral and furcal locations. The root canal and the pulp chamber are niche environments for the causative organism Biofilms Bacteria form biofilms and these pathological bacteria are embedded in the biofilms Biofilms protect the bacteria from antibiotic attack and make them a X 1000 more resistant to the effects. Infection portals Pulp becomes infected by Carious exposure Leaking restorations Dentinal tubules Fractures or cracks Inflammatory response The antigens and bacterial toxins percolate into the surrounding tissue Most likely anaerobic bacteria invade that provoke an inflammatory response i.e. Chemotaxis Enzymatic breakdown with the subsequent release of antigens The host mounts a immune response consisting of several classes intercellular messengers and antibodies. This response destroys much of the peripical tissue This results in the formation of various types of apical periodontal lesions. The defence reaction minimises the spread of infection. It cannot eliminate the microbes entrenched in a necrotic root canal , and biofilm. Treatment is required via surgical or non surgical endodontic therapy as biofilms protect the bacteria from the host defenses. Classification of AP Apical periodontitis is an inflammatory disease and classification is based on symptoms , aetiology or histopathology. Nomenclature and Classification Numerous terms are used such as Apical granulomas Apical cysts Periapical lesions Periapical osteitis Three main clinical groups symptomatic(acute) apical periodontitis asymptomatic(chronic) periodontitis apical abscess apical Symptomatic(acute) Apical Periodontitis The principal causes are irritants diffusing from an inflamed or necrotic pulp. Negative vitality test not always accurate Pain!!!(WHY?) Asymptomatic(chronic) Apical Periodontitis Preceded by an acute episode lesion frequently develops and enlarges without any subjective signs and symptoms Causes 1. Inadequate endodontic procedure 2. Low grade pathogenicity/ irritant 3. Pathosis is a long-standing “smoldering” lesion Asymptomatic(chronic) Apical Periodontitis(Cont) Non vital respnse Radiographic evidence is the key Called a peri radicular granuloma or periradicular cyst. Periradicular Granuloma. Nobuhara and del Rio(JOE1993;19:315) showed that 59.3% of the periradicular lesions were granulomas, 22% cysts, 12% apical scars, and 6.7% other pathoses Histologically, the periradicular granuloma consists predominantly of granulation inflammatory tissue with many small capillaries, fibroblasts, numerous connective tissue fibers, inflammatory infiltrate, and usually a connective tissue capsule Apical periodontitis (granuloma) with contained epithelium. Epithelial cells of periodontal ligament have proliferated within new inflammatory tissue. The epithelium tends to ramify in a reticular pattern (straight arrow) toward receding bone. It also may, as in this case, apply itself widely to the root surface (curved arrow). Infiltration of epithelium by round cells is everywhere apparent. Human tooth. Reproduced with permission from Matsumiya S.Atlas of oral pathology. Tokyo: Tokyo Dental College Press; 1955. Periradicular Cyst. Periradicular cyst shows a central cavity lined by stratified squamous epithelium This lining is usually incomplete and ulcerated The lumen contains a pale eosinophilic fluid and occasionally some cellular debris Apical cyst with marked inflammatory overlay. Round cells permeate both the epithelium and the connective tissue immediately deep to it. Spaces indicate where crystalline cholesterol has formed within the cyst. Bone formation is evident (arrow). This may reflect narrowing of the width of the connective tissue zone, as occurs in some apical cysts. Human tooth. Reproduced with permission from Matsumiya S. Atlas of oral pathology. Tokyo: Tokyo Dental College Press; 1955. Condensing Osteitis Inflammation of periradicular tissues of teeth usually stimulates concurrent osteoclastic and osteoblastic activities. Osteoclastic (resorptive) activities are usually more prominent than osteoblastic (formative) Condensing osteitis is associated with predominant osteoblastic activity Condensing Osteitis (CONT) attributable to a special balance between host tissues and the root canal irritants. Condensing osteitis, or chronic focal sclerosing osteomyelitis, is a radiographic variation of AAP and is characterized as a localized overproduction of apical bone. usually observed around the apices of mandibular posterior teeth with pulp necrosis or chronic pulpitis Condensing Osteitis (CONT) The tooth associated with condensing osteitis may be asymptomatic or sensitive to stimuli. Apical condensing osteitis that developed in response to chronic pulpitis. Additional bony trabeculae have been formed and marrow spaces have been reduced to a minimum. The periodontal ligament space is visible, despite increased radiopacity of nearby bone. APICAL ABSCESSES An abscess is a localized collection of pus in a cavity formed by the disintegration of tissue Apical abscesses can be divided into symptomatic or asymptomatic conditions APICAL ABSCESSES Symptomatic Apical Abscess A sudden egress of bacterial irritants into the periradicular tissues severe sequelae, acute osteitis and cellulitis. Accompanied by exudate formation within the lesion May occur without any obvious radiographic signs infection and rapid tissue destruction arising from within AAP( Phoenix abcess) APICAL ABSCESSES/clinical May or may not have swelling Swelling may be localized or diffuse Varying degrees of sensitivity to percussion and palpation No pulp reaction to cold, heat, or electrical stimuli as the involved tooth has a necrotic pulp Radiographic features of the SAA vary from a thickening of the periodontal ligament space to the presence of a frank periradicular lesion Radiographic features of symptomatic apical abscess. The patient developed sudden symptoms of pain and facial swelling. Radiographically, a lesion is apparent apically to the maxillary left lateral incisor, that did not respond to vitality tests, confirming pulpal diagnosis of necrosis. Asymptomatic Apical Abscess Asymptomatic apical abscess (AAA), also referred to as suppurative apical periodontitis, is associated with a gradual egress of irritants from the root canal system into the periradicular tissues and formation of an exudate. The quantity of irritants, their potency, and their host resistance are all important factors in determining the quantity of exudate formation and the clinical signs and symptoms of the lesion. Asymptomatic apical abscess is associated with either a continuously or intermittently draining sinus tract. WHO uses a symptomatic classification based on clinical signs Acute apical periodontitis Chronic apical periodontitis Periapical abscess with sinus Periapical abscess without sinus Radicular cyst Histopathological classification (Nair PNR: Pathology of Apical Periodontitis) In order to understand the disease process a histopathological classification is used: 1. 2. 3. 4. The distribution of pathological cells in the lesion Presence or absence of epithelial cells Transformation of a lesion into a cyst The relationship of the cyst cavity to the affected root Histopathological classification Acute apical periodontitis - an acute inflammation of endodontic origin . A distinct focus of neutrophils have to be present Primary or initial short lived inflammation in a healthy periodontium. secondary or exacerbating when an acute episode occurs on a preexisting chronic lesion *also called a phoenix abcess Histopathological classification Established chronic apical periodontitis Long standing inflammation presence of granulomatous tissue Cells are lymphocytes , plasma cells and macrophages Lesion may be epithelialised or nonepithelialised Histopathological classification Periapical true cyst is an apical inflammatory cyst with a distinct pathological cavity completely enclosed in an epithelial lining so that NO communication to the root canal exists Histopathological classification A periapical pocket cyst is an apical inflammatory cyst containing a saclike epithelium lined cavity that is open and continuous with the root canal Histopathologically the lesions of AP can be classified as acute, chronic ,or cystic .AAP may be (A.) primary or secondary(B) and is characterized by a focus of PMN, (C) major component are lymphocytes plasma cells and macrophages, (D) true cysts enclosing the lumina and pocket cysts (E)cavity is open to the root canal. Arrows indicate the direction of in which the lesion can change. Important points Bacteria are anaerobes Bacteria have to be present There has to be a portal for infection to occur i.e. Caries Clinical procedures Fractures Dentinal tubules To treat or not to treat? Anatomic considerations Root shapes? Can you remove infected hard and soft tissue Give disinfecting agents access to the apical canal space Create space for the delivery of medicaments and subsequent obturation Retain the integrity of the radicular structures To treat or not to treat? Is the tooth restorable? Is there an adequate ferule, the amount of remaining tooth structure Is root decay present Vertical fractures Post preparations in teeth Anatomical positions of the tooth Occlusal forces on the tooth To treat or not to treat? Restorative requirements of the tooth Aesthetic requirements Sclerotic canals Surgical Posterior part of mandible Inferior dental nerve Thickness of mandible Mental foramen Facial artery PDL Consider alternative Surgical Posterior Sinus perforation with infected root fragments Palatal access Anterior part of Maxilla maxilla / mandible Long roots Inclinations (mandible) and mental protuberance Prepared teeth are anatomically more difficult to treat Endodontic and periodontal relationships Vascular connections exist between the pulp and periodontal ligament. Pulp and periodontal problems are responsible for more than 50% of tooth mortality. There is no doubt that an interrelationship exists in diseases that affect both the pulp and periodontium When the pulp necroses for whatever reason products from pulp degeneration reach the supporting periodontium. This is characterised by bone loss, tooth mobility , and sometimes sinus tract formation. Apically if this occurs , a periradicular lesion forms which can extend crestally (Reverse pocket is formed) Periodontal disease may have a gradual , atrophic effect on the pulp. Periodontal treatments such as deep root planing or curettage, or localized irritants e.g. acids may cause pulpal irritation.is Apical foramina have been shown to be the most direct root of communication to the periodontium. In addition lateral or accessory canals with 28% at the furcation. Periradicular periodontitis Acute, painful to biting or percussion, the vitality may or may not be positive. No periradicular radiolucency and widened PDL, Apical 1/3 of root Chronic , no clinical symptoms, negative vitality test , periapical radiolucency , altered patient sensation Periradicular abcess Acute, sensitive to pressure and palpation, negative vitality test , increased mobility , increased pdl space, associated temperature Chronic, no clinical symptoms, no vitality response periradicular radiolucency on radiograph, suppurative lesion(pus drainage ) Periodontal considerations Channels exist between pulp and periodontal tissue These include neural pathways, lateral canals dentinal tubules, palato-gingival grooves periodontal ligament alveolar bone , apical foramina and vascular and lymphatic pathways Endodontic / Periodontic Relationships Primary endodontic -lesions lateral aspects of the root sinus tract along the root – gutta-percha trace Primary endodontic with secondary periodontal involvement –accumulation of plaque / calculus apical migration of tissue Endodontic / Periodontic Relationships Primary periodontal lesions -deposit in sulcus migrates apically. Vital pulp got to distinguish this from previous both look the same. Primary periodontal secondary endodontic involvement-accentuated pain from lesion. Hard to separate from endo perio Endodontic / Periodontic Relationships True combined lesion- damage to pulp and periodontium at the same time that may coalesce classic ‘J’- lesion Treatment can include the resection of roots (multirooted) , but lesions associated with cracked roots , older patients and posts. Regeneration procedures. NONENDODONTIC PERIRADICULAR LESIONS Got to differentiate between pulpal pathology and nonendodontic origins of alterations in bone morphology. 38 radiolucent lesions and other abnormalities of the jaws.Three of these lesions, dental granuloma, radicular cyst, and abscess, are categorized as being related to necrotic pulps. In addition,16 radiopaque lesions of the jaws, 3 of which, condensing osteitis, sclerosing osteomyelitis, and Garré’s osteomyelitis, are also related to pulpal pathosis Never assume a radiolucency is pulpal pathology. NONENDODONTIC PERIRADICULAR LESIONS Lesions of the jaws categorized as odontogenic or nonodontogenic in origin Odontogenic lesions arise from remnants of odontogenesis (or the tooth-forming organ), either mesenchymal or ectodermal in origin. Nonodontogenic lesions trace their origins to a variety of precursors and therefore are not as easily classified. Differentiating between lesions of endodontic and nonendodontic origin is usually not difficult. Pulp vitality testing, when done with accuracy, is the primary method of determination; nearly all nonendodontic lesions are in the region of vital teeth, whereas endodontic lesions are usually associated with pulp necrosis, giving negative vitality responses. Except by coincidence, nonendodontic lesions are rarely associated with pulpless teeth. Odontogenic Cysts Dentigerous Cyst Lateral Periodontal Cyst Odontogenic Keratocyst Residual Apical Cyst. Lateral periodontal cyst.Well-circumscribed radiolucent area in apposition to the lateral surfaces of the lower premolars (black arrows demarcate the extent of lesions). No clinical signs or symptoms were noted. Pulps tested vital. Bone Pathology: Fibro-osseous Lesions Periradicular Cemental Dysplasia Osteoblastoma and Cementoblastoma Cementifying and Ossifying Fibroma. A, Periradicular cemental dysplasia (osteofibrosis), initial stage. Pulps in both teeth are vital. B, Transition to the second stage is developing. C, Biopsy of periradicular osteofibrosis, initial stage. Fibrous connective tissue lesion has replaced cancellous bone. Cementoblastoma. The lesion is a fairly well-defined radiopaque mass surrounded by a thin radiolucent line. It has also replaced the apical portions of the distal root of the first molar Ossifying fibroma. The patient presented with pain. The pulp was vital, indicating that this was not an endodontic pathosis. Root canal treatment was followed by root end removal and excision of the lesion. Biopsy confirmed the diagnosis Odontogenic Tumors Ameloblastoma. Two examples of ameloblastoma. A, Surgical specimen of infiltrating ameloblastoma of mandible. B, “Unicystic” ameloblastoma. This solitary lesion has displaced teeth much as an apical cyst would do. The teeth are vital. Nonodontogenic Lesions Central Giant Cell Granuloma. Nasopalatine Duct Cyst Simple Bone Cyst. Globulomaxillary Cyst Enostosis. Malignancies Carcinomas or sarcomas of various types are found in the jaws, rarely as primary but usually as metastatic lesions Carcinoma. Generally found in older patients, involvement of the jaws (usually the mandible) is by metastasis from a primary lesion elsewhere Carcinoma lesions of the jaw may also manifest pain and swelling, loosening of teeth, or paresthesia, similar to endodontic pathosis Radiolucent jaw malignancies have been mistaken for periradicular lesions. Radicular cyst Residual cyst Paradental and mandibular infected buccal cysts Mandibular Infected Buccal Cyst Lateral periodontal cyst Glandular odontogenic cyst Odontogenic keratocyst Gorlin syndrome