Case report template
advertisement

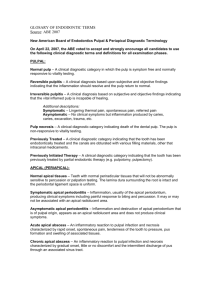
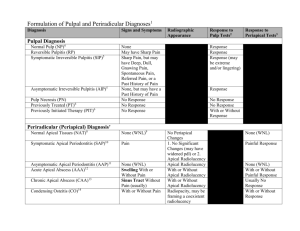
ROOTS CYBERCOMMUNITY - SUMMIT V Gettin’ on the same page Gettin’ on the same page Aetiology, classification and pathogenesis of pulp and periapical disease Dental pulp is a richly vascularized and innervated tissue, enclosed by surrounding tissues that are incapable of expanding, such as dentin. It has terminal blood flow and small-gauge circulatory access the periapex. All of these characteristics severely constrain the defensive capacity of the pulp tissue when faced with the different aggressions it may be subjected to. Pulp tissue can also be affected by a retrograde infection, arising from the secondary canaliculi, from the periodontal ligament or from the apex during the course of periodontitis. Due to the fact that periapical disease is almost inevitably preceded by pulp disease, we shall begin by describing the causes of pulp disease and will then proceed to a discussion of the causes of periapical disease. The course of illness and classification of these pathological entities will depend on the aetiology involved. We will analyse pulp necrosis and pulp degeneration that are capable of triggering reversible apical periodontitis or irreversible apical periodontitis. Warm Up Chief complaint • intermittent pain, sense of pressure, pain on biting, hard to localize, patients answers for the most part are vague, seems to be focused on distal proximal aspect of quadrant • level of agitation is such that accuracy of responsiveness in question • taking penicillin for two days (irregular dosing) Case #1 Factoids Chief complaint • positive response to thermal challenge • hyperaemic or engorged pulp • w/o periapical extension • treated in a single visit • RCT or HealOzone? • post treatment medication recommendations? • restorative considerations? Case #2 Factoids Chief complaint • generalized discomfort on chewing in maxillary right quadrant • strong focus on 1.6 • degenerating pulp with periapical extension • one visit • expectation of mild post-tx pain • NSAIDS, analgesics prescribed? • system or method of instrumentation • apical terminus – Rosenberg Technique - Discuss • irrigation routine – discuss • Comprehensive Care Considerations - discuss J Calif Dent Assoc. 2004 Jun;32(6):493-503 The success of endodontic therapy: healing and functionality. Friedman S, Mor C. University of Toronto Faculty of Dentistry, Canada. Based on selected follow-up studies that offer the best evidence, the chance of teeth without apical periodontitis to remain free of disease after initial treatment or orthograde retreatment is 92 percent to 98 percent. The chance of teeth with apical periodontitis to completely heal after initial treatment or retreatment is 74 percent to 86 percent, and their chance to be functional over time is 91 percent to 97 percent. Thus there does not appear to be a systematic difference in outcome between initial treatment and orthograde retreatment. is less consistent The outcome of apical surgery than that of the nonsurgical treatment. The chance of teeth with apical periodontitis to completely heal after apical surgery is 37 percent to 85 percent, with a weighted average of approximately 70 percent. However, even with the lower chance of complete healing, the chance for the teeth to be functional over time is 86 percent to 92 percent. Case #3 Factoids Chief complaint • masticatory sensitivity • RCT done prior – time indeterminate • apical periodontitis in evidence • 2 visits – interim calcium hydroxide procedure • NSAIDS, analgesics NO antibiotics prescribed • irrigation routine – citric acid and CHX • CLP considerations J Endod. 2004 Oct;30(10):689-94. An evidence-based analysis of the antibacterial effectiveness of intracanal medicaments. Law A, Messer H. Postgraduate Endodontics, School of Dental Science, University of Melbourne, Melbourne, Australia. The authors reviewed the literature evaluating the antibacterial effectiveness of intracanal medicaments used in the management of apical periodontitis. A PICO (problem, intervention, comparison, outcome) strategy was developed to identify studies dealing with calcium hydroxide, phenolic derivatives, iodinepotassium iodide, chlorhexidine, and formocresol. The final inclusion/exclusion criteria eliminated all papers except five that evaluated calcium hydroxide. The total sample size in the included studies was 164 teeth. Microbiologic sampling was performed before endodontic treatment (S1), after instrumentation and irrigation (S2), and after intracanal medication (S3). At S2, 62% of canals were positive. After medication, 27% still showed detectable growth. Of cultures that were positive at S2, 45% were still positive at S3. Most studies did not address issues of culture reversals or false positive and false negative cultures. The main component of antibacterial action appears to be associated with instrumentation and irrigation, although canals cannot be reliably rendered bacteria free. Calcium hydroxide remains the best medicament available to reduce residual microbial flora further. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 Nov;96(5):618-24. Efficacy of chlorhexidine- and calcium hydroxide-containing medicaments against Enterococcus faecalis in vitro. Basrani B, Tjaderhane L, Santos JM, Pascon E, Grad H, Lawrence HP, Friedman S. Dalhousie University, Endodonic Division, Department of Dental Clinical Sciences, Halifax, Nova Scotia, Canada. OBJECTIVE: We sought to assess the efficacy of chlorhexidine (CHX) and calcium hydroxide, Ca(OH)(2), against Enterococcus faecalis in vitro. STUDY DESIGN: The effect of CHX (0.2% and 2% in gel or solution) and Ca(OH)(2) (alone or with 0.2% CHX gel) was evaluated by using the agar diffusion test and an in vitro human root inoculation method, to measure zone of inhibition or bacterial growth with optical density analysis, respectively. For optical density analysis, samples from infected root canals were collected after 7 days of medication and were cultured for 24 hours in brain-heart infusion to detect viable bacteria. RESULTS: In the agar diffusion test, CHX was effective against E faecalis in a concentration-dependent fashion, but Ca(OH)(2) alone had no effect. In the root canal inoculation test, CHX was significantly more effective against E faecalis than Ca(OH)(2) was (P < .05), but there were no significant differences between the modes of medication or concentrations of CHX. CONCLUSIONS: CHX is effective against E faecalis in vitro. Further in vivo studies are needed to confirm the value of CHX in clinical treatment. • • • • • • Chief complaint • localized, nodular swelling over maxillary first molar history of RCT, CAP evident retx chosen as tx option CHX and Ca(OH)2 used as interim treatment dressing NSAIDS, analgesics prescribed Primary focus of failure – undetected MBx canal Pulp and Periapical Disease Oral microorganisms Root Canal Therapy Mechanical Instrumentation Irrigation Intra-canal medication Microbial Control Phase R.C. Filling Effect of Ca(OH)2 on Microorganisms in Necrotic Pulps Control of Endodontic Infection Card et al. JOE 2002 Sjøgren U et al. IEJ 1997 Ørstavik D et al. IEJ 1991 Bystrøm et al. EDT 1987 Kerekes et al. JOE 1979 Volume of Microbial Contents 1. Mech. preparation #25 #30 #35 #40 Apical Preparation Control of Endodontic Infection 1. Mech. preparation #25 #10 #40 Courtesy Dr. Richard Walton Control of Endodontic Infection 1. Mech. preparation #25 #25 #25 Courtesy Dr. Richard Walton Apical Periodontitis Prevalence Increases with age • Age 50: 50% experience the disease • Age > 60: 62% exhibit the condition • US Census data: 420 million root filled At 90% success: 42 million failing At 80% success: 84 million failing At 60% success: 168 million failing • Eriksen 1991, 1998; Figdor 2002 No lesion (%) 40 20 0 60 Cross-sectional studies Lupi-Pegurier et al. 2002 Hommez et al. 2002 Dugas et al. 2002 Tronstad et al. 2000 Kirkevang 2000 De Moor et al. 2000 Sidaravicius et al. 1999 Marques et al. 1998 Weiger 1997 Saunders 1997 Eriksen et al. 1995 Buckley & Spangberg 1995 Ray & Trope 1995 Petersson 1993 De Cleen et al. 1993 General Population 100 80 Treatment OutcomeS Variability 50% to 95% Status quo or change? Effects of four Ni-Ti preparation techniques on root canal geometry assessed by micro-computed tomography Peters OA, Schonenberger K, Laib A. Int Endod J. 2001 Maxillary molars ....all instrumentation techniques left 35% or more of the canals' surface area unchanged. ….a strong impact of variations of canal anatomy was demonstrated.. Principles Functions of The Root Canal Filling #1.Entomb Entombexisting existingbacteria bacteria Prevent coronal and apical leakage Strengthen the root Bacteria and Prognosis Success by culturing results +ve culture -ve culture Engstrom et al (1964) 89% If bacteria were76% entombed, Zeldkow & Ingle (1963) 83% 93% Oliet & Sorin (1969) 80% 91% Sjögren et al. (1997) 68% 94% there would be NO difference in the healing of teeth with PA lesions 95% Bystrom et al (1987) “State of The Art” Gutta-Percha + Sealer ..stopping influx of periapical tissue Entomb existing bacteria derived fluid from reaching residual Prevent coronal andsystem apical bacteria in the root canal acting as a barrier, preventing releakage leakage infection of the root canal Strengthen the root (Sundqvist and Figdor, 1998) Before Completed endodontic procedure Permaflo Purple Final polished restoration Endo/Coronal Status GE & GR N % API (periapical inflamn) 330 91.4 GE & PR 164 44.1 PE & GR 302 67.6 PE & PR 188 18.1 Overall 1010 61% Good root filling and coronal restoration Coronal Leakage Swanson et al. 1987 - Dye leakage to apex 3 days: dye leakage to apex Khayat et al. 1993 - Bacteria to apex 30 days: bacteria to apex Trope et al. 1994 – Endotoxins to apex 20 days: endotoxin to apex Control of Endodontic Infection Smear Clear 1. Mech. preparation Ca(OH) 2 2. Canal disinfection ZZY-VAC 3. Obturation CHX 4. Top filling Heal Ozone BioPure™MTAD™ Adhesion Endodontics Case #3 Factoids Chief complaint • pain in maxillary right quadrant • pre-existing RCT and CAP • calcium hydroxide placed in #1.5 • NSAIDS, analgesics, no antibiotics • patient had persistent pain…swelling appeared • sinus tract traced to mesial root of #1.6 • #1.6 retreated with calcium hydroxide • case obturated and transitionalized for 90 days Maxillary Molar Teeth Relocation of the canal orifices Maxillary Molar Teeth Courtesy of Dr. Cliff Ruddle Relocation of the canal orifices Composite finishing burs Brasseler H274-016 Never be surprised Ancillary MB canals Gingival Sulcus .5-2.0mm Epithelial Attachment .75mm Conn Tiss. Attachment 1.25mm Case #4 Factoids Chief complaint • pain on chewing • inadequate RCT #3.6 • deficient margins • patient unable to identify source account for • always to review occlusion / facial typethe high incidence of • opposing fractured restorations mandibular molars: the Hiatt proposed the lever principle second molar is nearer the fulcrum of mandibular closure and thus receives the greatest force. If 4 canals in an upper molar panics you…………………