Dr Michael Barrington - Australian and New Zealand College of
advertisement

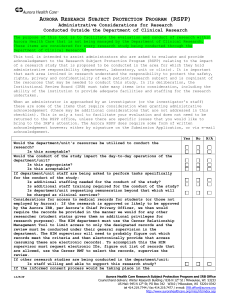
Development of a Registry of Regional Anaesthesia - the AURORA study St Vincent’s Hospital, Melbourne Dr Michael Barrington St Vincent’s Hospital, Melbourne Overview Registries as tools of evidenced based medicine AURORA Results June 1st 2008 January 31st 2011 Experience in development of AURORA Future direction Registries • Systematically and uniformly collect information from people who undergo a procedure, are diagnosed with a disease or use a health care resource “The term clinical registry is defined here as an observational database where there are: 1.No registry-mandated approaches to therapy 2. Relatively few inclusion or exclusion criteria” “The focus of clinical registries is to capture real-world clinical practice in large patient populations” Monitoring what we do and measuring our results and what happens to our patients are essential for improvement in the quality of care Do we (anaesthesiology) need registries of clinical care? “There are widespread gaps in our ability to rigorously define best practices. An astonishing number of recommended practices are based on expert consensus” • “We lack a precise and accurate portrayal of the clinical spectrum of LAST and its optimal treatment. This deficiency begs the development of a prospective data collection tool in the form of a robust, comprehensive registry of LAST events designed to avoid the many shortcomings of a retrospective literature review” Australian and New Zealand Registry of Regional Anaesthesia (AURORA) Hospitals involved in 2010 • The Alfred • Bendigo Shepparton • Ballarat St Vincent’s Hospital • Geelong Sir Charles Gairdner • Gold Coast University of Malaya Medical Centre • Lismore • Royal North Shore Hospital Wellington Waikato Hospitals involved in 2010 • The Alfred • Bendigo Shepparton • Ballarat St Vincent’s Hospital • Geelong • • • Sir Charles Gairdner AURORA currently a ANZCAofResearch Malaya Gold Coast supported by University Medical Centre grant Lismore Wellington Royal North Shore Waikato Hospital Australian and New Zealand Registry of Regional Anaesthesia (AURORA) AURORA June1st 2008 to January 31st 2011 Patients n 10, 461 PNB n F/M % 13, 648 49/51 Age Weight ASA (I/II/III/IV), % 58 ±19 80 ± 19 20/39/36/5 AURORA, June1st 2008 to January 31st 2011 80% of peripheral nerve blockade (PNB) US or US + NS Australian and New Zealand Registry of Regional Anaesthesia (AURORA) Local anaesthetic toxicity Incidence Period 2006 - 2008 2008 - 2011 n:1000 (95% CI) 0.98 (0.42 - 1.9) 0.4 (0.2 - 1.0) Local anaesthetic toxicity Incidence Period 2006 - 2008 2008 - 2011 n:1000 (95% CI) 0.98 (0.42 - 1.9) 0.4 (0.2 - 1.0) 2006 - 2011: Total of 14 cases LAST, 1 case severe LAST 20, 000 PNB Local anaesthetic toxicity Incidence Period 2006 - 2008 2008 - 2011 n:1000 (95% CI) 0.98 (0.42 - 1.9) 0.4 (0.2 - 1.0) 2008 - 2011, ropivacaine 78% PNB, 1.7 ± 0.9 mg/kg Local Anaesthetic Systemic Toxicity (LAST) AURORA, June1st 2008 to January 31st 2011 Nerve localization technique (results expressed as n:1000 (95% CI) Complication Nerve stimulation Ultrasound Total Late neurological deficit 0.8 (0.1 - 2.9) 0.2 (0.05 - 1.1) 0.4 (0.08 - 1.1) the risk of nerve damage is 0.4: 1000 Definitions: http://www.regional.anaesthesia.org.au/def_delayedfu.html Ultrasound guidance has not reduced nerve injury? % NS % US Ultrasound guidance has not reduced nerve injury? and ? Expectations Technology Rarity of the event Limitation of study design Nature of the outcome Clinical registries Complete inclusion of all eligible patients Capture ALL episodes of peripheral regional anaesthesia performed by ALL practitioners on ALL patients Reduce selection bias Business as usual No cherry picking Include good and bad outcomes Process Regular communication Train data collectors Online interface Followup defined Outcomes are defined Definition of RA related neurologic complication ✤ New onset of sensory/motor deficit consistent with nerve/plexus distribution area without other identifiable cause ✤ AND ✤ One of the following ✤ electrophysiologic evidence of nerve damage ✤ new neurological signs ✤ new onset of neuropathic pain in the nerve distribution ✤ paraesthesia in the affected nerve distribution area Schulz-Stubner S, Kelly J, Regional Anesthesia Surveillance System: First Experiences with a quality assessment tool for regional anesthesia and analgesia. Acta Anaesthesiol Scand. 2007; Important feature Systematic postoperative contact with all patients Investigation of all potential neurological deficits Allows separation of PNB-related deficits from those unrelated to PNB Results of neurological evaluation (2006 -08) Australian and New Zealand Registry of Regional Anaesthesia (AURORA) Late neurological deficit Period 2006 - 2008 2008 - 2011 n:1000 (95% CI) 0.4 (0.08 - 1.1) 0.4 (0.2 - 1.0) Complications 2008 - 2011 Outcome LAST Cardiac arrest Late neurological deficit n 6 1 6 n:1000 (95% CI) 0.4 (0.2 - 1.0) Comment Mild in severity 0.07 Paravertebral block (0.002 - 0.4) 0.4 (0.2 - 1.0) 5/6 comorbidities Complications 2008 - 2011 Outcome Wrong-site PNB Respiratory depression n 4 3 n:1000 (95% CI) Comment 0.3 (0.08 - 0.8) Lower limb, language 0.2 (0.05 - 0.6) Phrenic nerve paralysis (2) Neuraxial spread (1) Complications n:1000 (95% CI) Outcome Pneumothorax 2008 - 2011 0.9 (0.1 - 3.9) Comment Infraclavicular block (1) Supraclavicular block (1) Training Learn sonography skills on patients (independant of invasive procedures) Core skill Learn needling skills (principles) before performing blocks Pre-procedural training Procedure specific Use of phantoms is evidenced-based The Future n = 3056 n = 3505 n = 4710 n = 6609 % 2007 2008 2009 2010 New database www.anaesthesiaregistry.org Future Patient-rated outcomes Rotating data sets Develop research infrastructure Widen analytical techniques Collaboration interdisciplinary epidemiologists In conclusion - registries Are valid tools of evidenced based medicine Measure and report outcomes from routine practice Much of what we do and what happens to our patients is not documented or reported health care issue Improve the quality and safety of care In conclusion - AURORA Serious complications of PNB are infrequent Neurologic outcomes complex Serious LAST rare in our practice Wrong-site avoidable Debate role of supraclavicular block Training needs to be improved - workplace Thank you for your attention