Gastrointestinal Bleeding PCOM Internal Medicine Residents 2004
advertisement

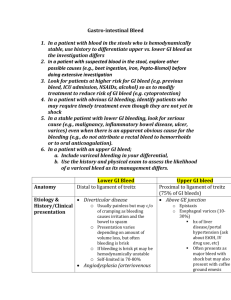
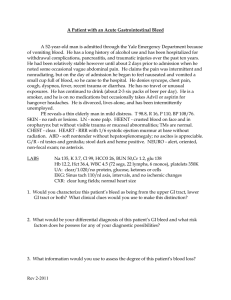
Gastrointestinal Bleeding PCOM Internal Medicine Residents 2004 GI Bleeding • • • • • • • • Initial Evaluation Approach to the Patient Sources Upper GI Bleeds Lower GI Bleeds Etiology Management Admission Orders Initial Evaluation • History and Physical points to Source/Etiology • History of Present Illness • Attention to PMHx, Social Hx, Medications History • • • • • Hematemesis (coffee grounds vs. bright red) Hematochezia Melena - dark, tarry stool Pain symptoms Medications – NSAIDs, steroids, ASA, Plavix, Coumadin, Lovenox, Heparin, Iron • PMHx - arthritis, ulcer disease, EtOH Good Thorough Physical Exam Including: • • • • • • • • • HR, BP, tilt test, RR, O2 saturation General appearance, Mental status Neck veins, oral mucosa Skin temperature and color Abdominal exam Rectal Stigma of Cirrhosis NG Tube findings (upper vs. lower g.i. source) Urine output Approach to the patient • Labs • CBC • Serial HgB • Platelets • BMP • BUN, Cr • Type and Crossmatch • Coagulation studies • Imaging studies? Sources of GI Bleeding • Upper GI Tract • • Proximal to the Ligament of Treitz 70% of GI Bleeds • Lower GI Tract • • Distal to the Ligament of Treitz 30% of GI Bleeds Localization of Bleeding • • • • • • History NG Tube EGD Colonoscopy Tagged RBC Scan Angiography Upper GI Bleed • 50% present with hematemesis • NGT with positive blood on aspirate • 11% of brisk bleeds have hematochezia • Melena (black tarry stools)—this develops with apporximately 150-200cc of blood in the upper GI tract. – Stool turns black after 8 hours of sitting within the gut. Upper GI Bleed • Risk Factors • NSAID use • H. pylori infection • Increased age • Upper GI Bleeding accounts for approximately 350,000 hospitalizations per year. Upper GI Bleed • Etiology of Upper Bleeds • • • • • • • • • Duodenal Ulcer-30% Gastric Ulcer-20% Varices-10% Gastritis and duodenitis-5-10% Esophagitis-5% Mallory Weiss Tear-3% GI Malignancy-1% Dieulafoy Lesion AV Malformation-angiodysplasia Duodenal Ulcer Varices Esophagitis GI Malignancy • Esophageal Tumor GI Malignancy • Gastric Carcinoma Angiodysplasia Lower GI Bleed • • • • • Hematochezia Blood in Toilet Clear NGT aspirate Normal Renal Function Usually Hemodynamically stable Only 1/3 of patients with lower GI bleeds have positive orthostatics (tilt test). Lower GI Bleed • Etiology of Lower Bleeds • • • • • • • • Diverticular-20% AVM-10% Malignancy-2-26% Inflammatory Bowel Disease-10% Ischemic Colitis Acute Infectious Colitis Radiation Colitis/Proctitis Aortoenteric Fistula Diverticulosis Diverticulitis-NOT A CAUSE OF GI BLEEDING Colonic Polyps Malignancy • Colon Carcinoma Hemmorrhoids Management of GI Bleed • Oxygen • IV Access-central line or two large bore peripheral IV sites • Isotonic saline for volume resuscitation • Start transfusing blood products if the patient remains unstable despite fluid boluses. • Airway Protection • Altered Mental Status and increased risk of aspiration with massive upper GI bleed. Management of GI Bleed • ICU admit indications • Significant bleeding with hemodynamic instability • Transfusion • Brisk Bleed, transfusing should be based on hemodynamic status, not lab value of Hgb. • Cardiopulmonary symptoms-cardiac ischemia or shortness of breath, decreased pulse ox • 1 unit PRBC increases Hgb by 1mg/dL and increase Hct by 3% • FFP for INR greater than 1.5 • Platelets for platelet count less than 50K Basic Admission Orders • • • • • • • • Admit to ICU/intermediate care/telemetry s/o … Dx: Upper/Lower G.I. Bleed Condition: VS: Allergies: Activity: Bedrest Nursing: Is/Os, ? Foley Diet: NPO Basic Admission Orders (Cont.) • IVF: NSS @ ?cc/h • Medications: I.V. Protonix, convert medications to i.v., hold anti-hypertensives • Labs: serial H/H, type and cross, coags, Chem 7, LFTs • Consults: g.i., surgery? References • Harrison’s Principles of Internal Medicine 14th edition • Gastrointestinal Atlas.com endoscopy photos THE END