A Blueprint to Develop a Companion Diagnostic Assay, Jeff Allen, PhD
advertisement

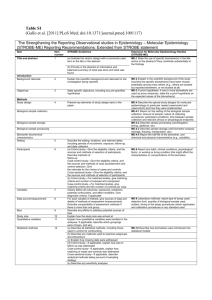
A Blueprint to Develop a Companion Diagnostic Assay Jeff Allen, PhD Executive Director, Friends of Cancer Research Draft Guidance for Industry and FDA Staff: In Vitro Companion Diagnostic Devices July 2011 • Goals: – Define IVD companion diagnostic devices – Clarify the need for FDA oversight and approval for safe and effective use – Provide direction for both industry and FDA staff on possible developmental pathways and the approval requirements for labeling of therapies that require IVD companion diagnostic devices • Guiding Principle: “Ideally a therapeutic and its corresponding IVD companion diagnostic device would be developed contemporaneously with the clinical performance and clinical significance of the IVD companion diagnostic device established using data from the clinical development program of the corresponding therapeutic product” A Blueprint to Develop a Companion Diagnostic Assay • Goals: Address key issues not raised in the 2011 Guidance Document and propose approaches for drug-Dx co-development that introduce flexibility and options in today’s drug development – Development strategy for Dx-selected populations – Defining selected population given Phase III data – Multi-marker diagnostic development • Guiding Principle: Although the different types of diagnostics used to identify the patient population will face different issues and requirements for analytical validation, with some biomarkers and assays being more challenging for co-development than others, the core principles regarding clinical validation and clinical utility will be similar. A Blueprint to Develop a Companion Diagnostic Assay • Workgroup 1- A Blueprint for Future Drug/Diagnostic Co-development Rich Buller, Vice President of Translational Oncology, Pfizer, Inc. Liz Mansfield, Director of Personalized Medicine, U.S. Food and Drug Administration (FDA) Rick Pazdur, Director of the Office of Hematology and Oncology Products, U.S. Food and Drug Administration (FDA) Nancy Roach, Chair, Fight Colorectal Cancer Howard Scher, Chief, Genitourinary Oncology Service, Memorial Sloan-Kettering Cancer Center Rich Simon, Chief, Biometric Research Branch, National Cancer Institute (NCI) Jane Fridlyand, Senior Statistical Scientist, Genentech (SSF) • Workgroup 2- Creating an Environment for Personalized Medicine Keith Flaherty, Director of Developmental Therapeutics, Cancer Center, Massachusetts General Hospital Pat Mahaffy, President and CEO, Clovis Oncology, Inc. Vince Miller, Senior Vice President, Clinical Development, Foundation Medicine Jeff Roche, Medical Officer, Center for Medicare and Medicaid Services (CMS) Jeff Shuren, Director Center for Devices and Radiation Health, U.S. Food and Drug Administration (FDA) Deb Rasmussen, Global Head of Regulatory Affairs, Janssen Diagnostics Janet Woodcock, Director Center for Drug Evaluation and Research, U.S. Food and Drug Administration (FDA) Development Strategy for Dx-Selected Populations • In general, development decisions are guided by the aim to maximize exposure of patients who are likely to benefit from a drug and minimize exposure of patients who are not, or who are at increased risk for serious adverse events. • Proposed decision-making strategy for determining whether and how evaluation of diagnostically negative patients could be undertaken • Analytical performance of the diagnostic assay must have been characterized before it is used in any clinical registration trial • If not, evaluation of marker-positive patients only is not possible, and an all-comers trial design must be used Factors that influence evaluation of marker-negative patients Provides support for restricting efficacy evaluation to Dx-selected patients only Key Factors and their categories Evidence supporting clear definition of diagnostically selected population Mechanism of action (MOA) Pre-clinical efficacy (in-vitro/in-vivo) Compelling evidence supporting threshold for definition of Dx-positive population (e.g., mutation; complete loss of expression; high-level amplification). Yes Threshold for Dx-positive population uncertain (e.g., continuous or ordinal biomarker). No Dx marker is an immediate drug target or a measure of activation of a pathway of the drug target. Yes Dx marker is less clearly related to drug target. No Dx has high sensitivity and specificity for drug activity. Yes Dx has high sensitivity and lower specificity for drug activity. No Class effect (i.e., knowledge of behavior Established class effect in Dx selected of existing drugs with similar populations. MOA/multiple MOAs (or First in Class (FIC). targets)/chemical structure or known pharmacological effects) Yes No If an all-comer approach was chosen: Recommended Phase III evaluation of Dx-negative patients, given Phase II outcome and the biomarker type Observed Clinical Risk-Benefit in Phase II (or Phase I if no Phase II) Clinically meaningful benefit/risk in Dxselected patients; detrimental benefit/risk in Dxnegative patients Clinically meaningful benefit/risk in Dxselected patients; no clinically meaningful benefit/risk in Dxnegative patients (a) Clear binary definition of Dxpositive population (e.g., mutation, complete loss of expression, highlevel amplification) No additional efficacy evaluation should be required of Dx-negative patients No or very limited benefit/risk evaluation of Dxnegative patients (b) Threshold for Dxpositive population uncertain (e.g., continuous or ordinal biomarker such as RT-PCR expression or IHC) Limited safety assessment of the patients with the biomarker value borderline with the proposed Dx threshold, dependent on severity of detriment Dx-selected population definition Clinically meaningful benefit/risk in all patients; biomarker shows better benefit in Dx-selected patients Fully assess benefit/risk in allcomers If there is concern with the strength of the marker/outcome relationship, gated or full benefit/risk evaluation of Dxnegative patients to define best threshold Development Strategy for Dx-Selected Populations • Staged clinical development • could be appropriate in cases where the treatment is expected to have activity in marker-positive patients • Biomarker information in label when Phase III trial is not diagnostically restricted • When restricted to test-positive, labeling is straight forward • When (+) and (-) are included a pre-specified analysis plan is needed and labeling can be more difficult – One approach might stipulate that such inclusion could be considered provided the following conditions are met: • Pre-specified primary endpoints are met (e.g., Dx-positive and all-comers). • Clinically meaningful difference in benefit estimate between Dx-positive and Dxnegative patients with no observed detriment in Dx-negative patients. Defining the Dx-Selected Population given Phase III Data • Situations in which sponsor may need to re-define the Dxselected patients – Readjusting the threshold on the biomarker prospectively specified in the trial – Evaluating the Phase III trial with regard to a biomarker not specified in the protocol • Proposal for planned threshold re-adjustment • Timing of threshold pre-specification for primary analysis • New marker specification after trial initiation or completion Multi-marker Diagnostic Development • Several biomarkers may be necessary to identify the patients likely to benefit from a therapy • For composite biomarkers such as scores that combine gene expression values, it is the score that is the biomarker that is used and that must be validated • For the case of gene mutations, if the sponsor is proposing to use as a biomarker the presence of any mutation of the gene or any of a pre-specified set of mutations, then it is that composite biomarker which must be validated in the Phase III trial. • Provided there is appropriate pre-clinical evidence and scientific rationale, clinical validation of each biomarker separately should not be required; rather, it should be sufficient to validate the combination of markers, essentially treating the pool of biomarkers as one DNA Sequencing and Companion Diagnostics • Next-generation sequencing (NGS) and screening platforms have multiple advantages over the current single-test, single-drug paradigm • Sponsors could obtain an Investigational Device Exemption (IDE) for the entire platform prior to the start of clinical testing. • The presence of a particular predictive biomarker in the platform could enable the entire platform to be adequate for selecting patients • If the new drug demonstrated acceptable clinical benefit, the biomarker could be reviewed and given FDA clearance for diagnostic use, along with approval for the drug • Much like composite assays, if the platform used multi-markers for selection, the platform should not require separate clinical validation for each component Breakthrough Therapies Advancing Breakthrough Therapies for Patients Act of 2012 – Senators Bennet (D-CO) Hatch (R-UT) and Burr (R-NC) – Representatives DeGette (D-CO) and Bilbray (R-CA) • Breakthrough Therapy Designation – Expedite drug development process for products that show remarkable clinical activity early – Minimize the number of patients exposed to a potentially less efficacious treatment A Blueprint for Drug/Diagnostic Co-development: Breakthrough Therapies September 6, 2013 • A forum to bring together researchers, sponsors, advocates and regulators to discuss the recognized opportunities and challenges associated with contemporaneous development of drugs and diagnostics, with a focus on how development of the diagnostic component can also be expedited in the instance of a Breakthrough Therapy designation. Forum Goals • Identify data elements that are essential for analytical validation that need to be prioritized early in development • Propose potential modifications for data elements that could be postponed until the post-market setting Supplementary Slides MASTER PROTOCOL CNB/CLIA Biomarker Profiling Biomarker A TT A CT* Endpoint (Interim PFS) OS Biomarker Β TT B CT* Endpoint (Interim PFS) OS Biomarker C TT C+CT CT* Unkn-Neg biomarker CT* Endpoint (Interim PFS) OS Anti PD1 Biomarker D TT D+E E* Endpoint (Interim PFS) OS TT=Targeted therapy, CT=chemotherapy (docetaxel or gemcitabine), E=erlotinib Courtesy of: Vali Papadimitrakopoulou