The Future of Clinical Trials: New Model to Enhance Efficiency, Jeff
advertisement

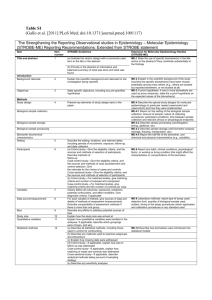
THE FUTURE OF CLINICAL TRIALS: NEW MODEL TO ENHANCE EFFICIENCY Jeff Allen, PhD Executive Director Friends of Cancer Research Current Challenges • Each potential new therapy is typically tested independently from other therapies seeking to treat the same condition • For every new trial, the protocol must be reviewed by a number of oversight entities • new phase III trials requires an average of 36 administrative or regulatory approvals and averages more than 2 years • Approximately 4% of adult cancer patients enroll in clinical trials • inability to meet accrual goals is a frequent factor causing trials to close, wasting time, money, and limited patient resources • New therapies molecularly targeted against specific mutations may be present in only a fraction of the patient population Design of a Disease-Specific Master Protocol 2012 Conference on Clinical Cancer Research http://www.focr.org/events/design-lung-cancer-master-protocol Major elements • Setting: Squamous cell carcinoma (SCCA), advanced stage, 2nd line therapy • Agents: Candidate drugs must demonstrate biologic activity against a measurable target with a proposed predictive biomarker • Study design: Multi-arm randomized, controlled phase II/III master registration protocol. Each arm able to open and close independent of other arms Screening • Archival FFPE tumor-common broad testing analytically validated platform suitable for registration purposes • Molecule–specific tests, to include IHC, fresh core needle biopsy as appropriate • Protocol arm powered for central test+ cases, with subsequent bridging studies as per FDA clearance. • Goal is to develop each molecule with a companion diagnostic to support clinical use Trial Structure • Primary Endpoint: Each arm independently powered for OS; interim analysis for PFS. Positive results at “rolling” interim analysis (no temporary closure) determine if a protocol arm proceeds to phase III portion. • Goal: minimum of 4 arms open at any time, to ascertain a reasonable chance for patients to be “biomarker positive”. • Marker-negative patients enter common control group treated with SoC (vs anti-PD1 agent) to establish annotated repository Trial operations • Operations Management: Neutral 3rd party - FNIH in collaboration with NCI Cooperative Groups • Independent Drug Selection Committee: evaluates each drug-marker pair for suitability • Oversight Committee: Comprised of leaders from NCI, Academia, FDA, industry, advocates, to ensure operational efficacy MASTER PROTOCOL CNB/CLIA Biomarker Profiling Biomarker A TT A CT* Endpoint (Interim PFS) OS Biomarker Β TT B CT* Endpoint (Interim PFS) OS Biomarker C TT C+CT CT* Endpoint (Interim PFS) OS CT* Unkn-Neg biomarker Anti PD1 Biomarker D TT D+E E* Endpoint (Interim PFS) OS TT=Targeted therapy, CT=chemotherapy (docetaxel or gemcitabine), E=erlotinib Courtesy of: Vali Papadimitrakopoulou Study Design Within Each Biomarkerdefined Subgroup R a n d o m i z a ti o n Phase II Analysis 56 PFS events Phase III Interim Analyses Based on OS Futility established Complete Accrual Final Analysis 210 OS events 12 months follow-up Stop Courtesy of: Mary Redman Master Protocol over time Additional drug/biomarker combinations dropped and added to study Trial Start Patient Accrual/ Patient Screening for initial biomarkers Marker/Drug A treatment arm starts A – HR=.84, Trial continues A -- 100%? eventsOS analysis A -- 30% eventsInterim analysis for OS Master Protocol Trial Timeline Marker/Drug B treatment arm starts Marker/Drug C apply to trial Marker/Drug C reviewed by steering committee Marker/Drug C added to trial B -- 30% eventsInterim analysis for OS Marker/Drug C treatment arm starts B– HR= .87Trial continues C--30% eventsInterim analysis for OS Benefits of a Master Protocol • Enrollment Efficiency: Grouping these studies under a single trial reduces the overall screen failure rate • Operational Efficiency: single master protocol can be amended as needed as drugs enter and exit the study • Consistency: every drug entered into the trial would be tested in the identical manner • Predictability: If pre-specified efficacy and safety criteria are met, the drug and accompanying companion diagnostic will be approved • Patient Benefit: offers the advantage of bringing safe and effective drugs to patients sooner than they might otherwise be available. Expert Working Group • Roy Herbst – Yale University • David Gandara – UC Davis • Vali Papadimitrakopoulou – MD Anderson • Fred Hirsch – University of Colorado • Mary Redman - Fred Hutchinson Cancer Center • Jeff Abrams – National Cancer Institute • Jack Welch – National Cancer Institute • Shakun Malik – Food and Drug Administration • David Wholley – Foundation for the NIH • Vince Miller – Foundation Medicine • Eric Rubin - Merck