Telemonitoring for Heart Failure Evidence
advertisement
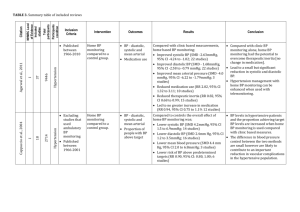
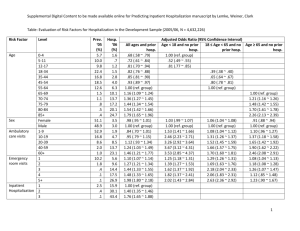
Telemonitoring for Heart Failure Evidence & Practice Professor John G.F. Cleland Department of Cardiology, Hull York Medical School University of Hull Kingston-upon-Hull UK Conflict of Interest: I have received honoraria and/or research support from Philips, Bosch, GE, Alere and St Jude 1.00 Survival of Patients with a Primary Discharge Diagnosis of Heart Failure England & Wales 2009-2010 Audit 0.75 • 0.00 0.25 0.50 About 1 million people affected in the UK ~450,000 admissions per year (65,000 in first diagnostic position) N = 19,240 (about 30% of all expected cases) 0 90 Median age 79 years <65 years ~3,000 65-75 years ~4,000 75-85 years ~7,000 >85 years ~5,000 180 Survival time (days) 55-64 years 75-84 years 270 65-74 years >=85 years 360 Cleland et al HEART 2011 TeleHealth Why is it Likely to Become Essential? 1. More patients with long-term conditions – – – More older people Longer survival with illness Better primary & secondary prevention 2. Fewer professionals to provide health-care – – – Smaller proportion of population of working age Loss of migrant workforce as economies rival UK Better paid or more attractive / less stressful jobs 3. More monitoring required – – – Higher expected standards of care More treatments that need to be monitored More things that can be monitored TeleHealth Why is it Likely to Become Essential? 4. Patient preference & Convenience – Patients, Carers, Staff 5. Reduced Costs – Buildings, Staff, Transport 6. Environmental impact – – – Transport Parking Buildings 7. Better record keeping !!!!!!!!!!!!!!!!!!!!!!! The Opportunity of Chronic Illness • Most patients soon learn routines – Or have relatives / friends that do • Most patients are interested in maintaining or improving their health • Patients are an ‘inexpensive’ but neglected healthcare provider opportunity • Invest in patients – Education – Active Partnership – Empowerment TeleHealth - What Might it Achieve? Ultimate Intermediate Titration of therapy Compliance Detection of exacerbation Cause of exacerbation Treatment of WHF Selection for Admission Discharge planning Patient Reassurance ReDuration Mortality Patient Costs admission of adm. Experience of care TEN-HMS The Trans-European Network–Home-Care Management System Patients about to be discharged from hospital after an exacerbation of chronic heart failure 54% of Patients Aged >70 years (Published JACC 2005) Mortality TEN-HMS Reduction in Mortality NTS or HTM v UC Absolute 16.4% Relative 36 % p < 0,05 Cleland et al JACC 2005 TEN-HMS “ How do you feel about your health since receiving Telemonitoring? “ 48.9% 38.9% 7.8% 3.3% much safer safer no change more anxious 1.1% much more anxious Undef . TEN-HMS Achieving Therapeutic Target 100 UC *** 95 *** NTS 90 HTM 85 *** 80 % 75 70 65 60 55 50 ACEi BB Spirono 120 Days Patient Clinical Status 70 60 50 40 30 20 10 0 . I/II ACEi IV or Dead III BB Spirono 240 240 Days Days *** differences between HTM and other groups. No difference between UC and NTS TEN-HMS: Total Patient Contacts Contacts Per 1,000 Days Alive and Out of Hospital 80 Telephone Contact 70 Office Visits 60 Home Visits 50 Hospitalisation 40 # 30 20 10 0 UC NTS # under-reporting of events likely in this group HTM P<0.01 HTM v NTS Structured Telephone Support n = 5,563 (Cochrane Review) Mortality New Trials • Tele-HF • TEHAF All-Cause Hospitalisation HR 0.88 (0.76-1.01); p=0.08 Inglis et al 2010 HR 0.77 (0.68-0.87.01); p<0.0001 Home Telemonitoring n = 2,710 (Cochrane Review) Mortality New Trials • TIM-HF • COMPASS • CHAMPION • SENSE-HF All-Cause Hospitalisation HR 0.66 (0.54-0.87); p<0.0001 HR 0.91 (0.84-0.99); p=0.02 Inglis et al 2010 Major Problems with RCTs of Service Delivery • Technology differs – Telephone Support including Voice Activated Systems – Physiological telemonitoring • Implanted or Not • Care usually improves if it is the focus of attention – Effect in control group – Beware: “before v after” comparisons • Lack of integration into existing services – Puts innovative interventions at a disadvantage • Selection of patients at low risk with modern treatment Percent of Days Lost To Hospitalisation or Death TEN-HMS (15 months) 37.0% 21.3% 22.6% 40 1.7 2.4 40 TIM-HF (26 months) 8.9% 8.4% TEHAF (12 months) 40 35 35 30 30 30 25 25 25 20 20 35 20 15 10 32.9 2.6 2.3 16.4 2.1 1.9 18.5 15 15 10 10 5 5 0 0 UC NTS HTM Death WHF Hosp Other Hosp 2 1.1 5.8 2.1 1.3 5 UC NTS HTM Death WHF Hosp Other Hosp 4.5% 6.1% 0.9 1.2 0.5 0.4 3.1 4.5 5 0 UC NTS HTM Death WHF Hosp Other Hosp What Have We Done for TeleHealth in Hull? • Established – International reference site (LifeLab) for HF epidemiology & research – International reputation for research excellence in telehealth – A model telehealth service • Grants – TEN-HMS – Four FP7 grants relating to telehealth & heart failure – EDRF • Industry Partnerships – Philips, GE, Bosch, Cardiomems, St Jude + others • Publications – >500 PubMed citations in related fields – TEN-HMS, Concept Papers, Editorials – Systematic Reviews (EJHF, BMJ & Cochrane) • Inventions – Dynamic risk analysis – Complex management algorithms The Hull Model for TeleHealth MEMS-based pressure sensor Device Implant Non-Invasive Home Monitoring Community TeleKiosks Screening Long-Term Conditions Services for Patients with Heart Failure The Kingston-upon-Hull Model Heart Failure Discharge Nurse Heart Failure Telemonitoring Nurse Community Heart Failure Specialist Nurses Voluntary Patient-Support Organisations Patients in Hospital Patients at Home Family Doctor (NT-proBNP) Specialist Clinics Hull Telemonitoring Service Outcomes Compared to Historical Data, Surveys & Trials 40 35 30 Observed HEY 2007 Surveys Trials 25 20 15 £350,000 10 £300,000 5 £250,000 Cost-Effectiveness of TeleHealth (Hull) Total gross savings Total service cost £200,000 0 £311,573 £224,416 Total net savings £150,000 B H ed Ap r-1 Ma 0 y-1 0 Jun - 10 Jul -1 Au 0 g-1 Se 0 p-1 0 Oc t- 1 No 0 v-1 De 0 c-1 0 Jan - 11 Fe b-1 Ma 1 r-1 1 To ta l 10 s/ £0 ns io ed lis at lis ta pi os £50,000 £87,157 y Da H ta pi os s hs t ea Pt D £100,000 Where Next? • Interactive TV • New monitoring technologies • Implanted devices • More intelligent use of the patient data • Investing in patients as health-care providers The Hull Heart Failure Life-Lab 30,000 patient-years of follow-up Largest, Longest Follow-up, Epidemiologically-Representative Cohort of Heart Failure in the World Rich in phenotyping, serial biomarker and outcome data 50 Probability of Death (%) 45 50 40 40 35 30 30 20 25 10 20 0 15 10 NT -p 2 10 r oB NP ( pm ol/L 10 10 ) 1 10 0 1 5 g/L) 0 (m CRP HeartCycle Programme • Shift from crisis detection to health maintenance • Health Maintenance Envelope – More ‘optimistic’ – Better way to engage/motivate patients – More active management – More activity likely to hold ‘actors’ attention – Clinical calibration – Addresses the issue of false alerts • Personalised Careplan – Treatments – Ideal monitoring envelope Motivation: feedback on measures and trends, what they mean and what to do about them Health-Care Provider Secondary Loop Analysis Intelligent, integrated, multimeasure (time & type) personalised analysis Education: on healthy lifestyle, reasons for treatments, self management Patient / Carer Primary Loop 70% of Care Decisions Communication System ‘Monitor’ Opportunities for TeleHealth • Change in Philosophy • Investment in patients (rather than experts) • Patients as first and possibly main tier of healthcare • Communication • Patient, community health & social services, specialists • Common health record • Checked (at least in part) by the patient themselves • Decision support analysis • Patient & professional support • Research potential +++ • Healthcare innovation • Pharmaceutical industry especially • Route to faster (ethical) adoption • Convenience & Preference • Patient, Carer, Health Professional • Environmental impact Conclusion • The first era of telemonitoring is over • Time to move from – Crisis Detection to – Health Maintenance