Document
advertisement

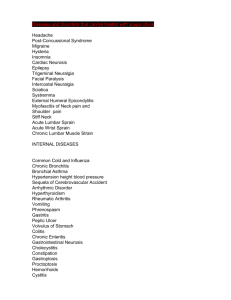
Nursing Care of Clients Experiencing Pain Pain Pathway • A-delta fibers: transmit pain quickly, associated with acute pain • C-fibers: transmit pain more slowly, diffuse burning pain and chronic pain • Inhibitory mechanisms: the analgesia system stimulates a pain inhibitory center in the dorsal horns of the spinal cord (the exact mechanism is unknown) • Endorphins: naturally occurring opioid peptides present in the neurons in the brain Pain Pathway Pain Pathway Pain Pathway Acute, Chronic, Central, Phantom, and Psychogenic Pain • Acute Pain – Somatic Pain • May be sharp or diffused • May be accompanied by nausea and vomiting – Visceral Pain • Arises from the body organs • Usually dull and poorly localized • May be referred or may radiate – Referred Pain • Perceived in an area distant from the site of the stimuli Acute, Chronic, Central, Phantom, and Psychogenic Pain Acute, Chronic, Central, Phantom, and Psychogenic Pain • Chronic Pain – Recurrent Acute Pain • Well-defined episodes of pain • Migraine headaches, sickle cell crisis – Ongoing Time-limited Pain • Persists for a definite time period • Ends with control of the disease, rehabilitation, or death Acute, Chronic, Central, Phantom, and Psychogenic Pain • Chronic Pain – Chronic Nonmalignant Pain • Not life-threatening but persists past expected time for healing – Chronic Intractable Nonmalignant Pain Syndrome • Client unable to cope well with the pain • Pain may be mild to severe • The pain itself becomes the pathologic process Acute, Chronic, Central, Phantom, and Psychogenic Pain • Central Pain – May be caused by a vascular lesion, tumor, or inflammation • Phantom Pain – Thought to be due to stimulation of severed nerves at the amputation site • Psychogenic Pain – Involves a long history of severe pain – The pain is real and can lead to physiologic changes Factors Affecting Pain Response • • • • • • Age Sociocultural influences Emotional status Past experiences with pain Meaning associated with the pain Lack of knowledge Myths and Misconceptions Concerning Pain • Pain is a result, not a cause • Chronic pain is really a masked form of depression • Narcotic medication is too risky to be used for chronic pain • It is best to wait until a client has pain before giving medication • Many client’s lie about the existence or severity of pain • Pain relief interferes with diagnosis Collaborative Care for Pain • Medications – NSAIDs: analgesic, antipyretic, and antiinflammatory action – Narcotics: opioids – Antidepressants: act on the retention of serotonin, thus inhibiting the pain sensation – Anticonvulsants: used for headache and neuropathic pain – Local anesthetics: blocks the transmission of nerve impulses, therefore blocking pain Collaborative Care for Pain Collaborative Care for Pain • Surgery – Cordotomy: an incision into the anterolateral tracts of the spinal cord to interrupt the transmission of pain – Neurectomy: removal of part of the nerve – Sympathectomy: destruction of the ganglia by incision or injection – Rhizotomy: surgical severing of the dorsal spinal roots – Transcutaneous electrical nerve stimulation (TENS): electrodes stimulate the A-beta touch fibers to close the “pain” gate Collaborative Care for Pain Collaborative Care for Pain • Complementary Therapies – Acupuncture – Biofeedback – Hypnotism – Relaxation – Distraction – Cutaneous stimulation Nursing Process for Clients with Pain • • • • • Assess the client’s pain level Establish a nursing diagnosis Plan and implement a care plan Educate the client Evaluate the patient’s response to the care plan Nursing Process for Clients with Pain Resources • Evidence Report/Technology Assessment Pain assessment and management of cancer pain. • American Cancer Society Principles of pain management in the treatment of acute and chronic pain. • Department of Veterans Affairs Pain as the 5th vital sign. Resources • The Joint Commission Type in “pain management standards” in the search box. Be sure to use quotation marks. • American Society for Pain Management Nursing Provides information for nurses on pain management through education, standards, advocacy, and research. Resources • American Pain Foundation Handles the undertreatment of pain. • American Pain Society A wide range of resources on pain at this professional site, including bulletins, journals, advocacy/policy, events and guidelines. • American Academy of Pain Management Serves professionals and clients in pain, including an online forum, local resources, programs, and a pain management databank. Resources • American Chronic Pain Association Offers support and information for people with chronic pain through support and education. Includes FAQs, links, and resources. • Agency for Healthcare Research and Quality Offers pain management guidelines, resources, and research citations.