Pathophysiology.of.retinal.vein.occlusion
advertisement

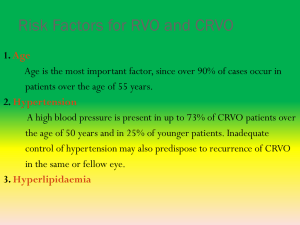
In the name of god Pathophysiology of retinal vein occlusion Hamid Fesharaki MD Eye department Isfahan University of medical sciences Types of retinal venous occlusion Central retinal vein occlusion Branch retinal vein occlusion Hemi retinal vein occlusion Branch Retinal Vein Occlusion • The ophthalmoscopic findings of acute BRVO include : • superficial hemorrhages, retinal edema, and often cotton-wool spots (NFL infarcts) in a sector of retina drained by the affected vein . Branch retinal vein occlusions occur most commonly at an arteriovenous crossing. • The degree of macular involvement determines the level of visual impairment. • When the occlusion does not occur at an arteriovenous crossing, the possibility of an underlying retinochoroiditis should be considered Branch Retinal Vein Occlusion The mean age for patients at the time of occurrence is their sixties. The obstructed vein is dilated and tortuous, and, with time, the corresponding artery may become narrowed and sheathed. The quadrant most commonly affected is the superotemporal (63%); nasal vascular occlusions are rarely detected clinically. A variant of BRVO based on congenital variation in central vein anatomy may involve either the superior half or inferior half of the retina (hemispheric or hemi central retinal vein occlusion Branch Retinal Vein Occlusion The Eye Disease Case-Control Study identified the following abnormalities as risk factors for the development of BRVO: . history of systemic arterial hypertension . cardiovascular disease . increased body mass index at 20 years of age . history of glaucoma. Diabetes mellitus was not a major independent risk factor. Branch Retinal Vein Occlusion • Histologic studies suggest that: • common adventitia binds the artery and the vein together at the arteriovenous crossing and that thickening of the arterial wall compresses the vein resulting in turbulence of flow, endothelial cell damage, and thrombotic occlusion. Branch Retinal Vein Occlusion • The thrombus may extend histologically to the capillary bed. • Secondary arterial narrowing often develops in the area of occlusion. • Visual prognosis in BRVO is most closely related to the extent of capillary damage and retinal ischemia in the macula Non-perfused BRVO Branch Retinal Vein Occlusion • . Fluorescein angiography is used to assess the extent and location of retinal capillary nonperfusion. • The integrity of the parafoveal capillaries is an important prognostic factor for visual recovery. • Vision may be reduced in acute cases from macular edema, retinal hemorrhage, or perifoveal retinal capillary occlusion. • The hemorrhage resolves over time, and capillary compensation and collateral formation may permit restitution of flow with resolution of the edema and improvement in visual function. • In other eyes, however, progressive capillary closure may occur. Ischemic BRVO with Neovascularization Branch Retinal Vein Occlusion • Extensive retinal ischemia (greater than 5 disc diameters) results in neovascularization from the retina or optic nerve • in approximately 40% of eyes, and 60% of such eyes will develop preretinal bleeding if laser photocoagulation is not performed. • Overall, approximately 50%60% of patients with all types of BRVO will maintain visual acuity of 20/40 or better after 1 year. Ischemic BRVO with neovascularization Retinal vasculitis with BRVO Retinal Vasculitis with Hemorrhages and Cotton Wool Spots Central retinal vein occlusion Dilated and tortuous Retinal veins swollen optic disc intraretinal hemorrhages Retinal edema Type 1 CRVO: A mild, nonischemic form sometimes referred to as partial, perfused, or venous stasis retinopathy Nonischemic CRVO • Mild (nonischemic) CRVO is characterized by • good visual acuity, a mild afferent pupillary defect, and mild visual field changes. • Funduscopy shows mild dilation and tortuosity of all branches of the central retinal vein as well as dot-and-flame hemorrhages in all quadrants of the retina Nonischemic CRVO • Macular edema with decreased visual acuity and mild optic disc swelling may or may not be present. • If disc edema is prominent in younger patients, a combined inflammatory and occlusive mechanism may be present that has been termed papillophlebitis. • Fluorescein angiography usually demonstrates prolongation of the retinal circulation time with breakdown of capillary permeability but minimal areas of nonperfusion. • Anterior segment neovascularization is rare in mild CRVO. Nonischemic CRVO Fluorescein Angiography A mild increase in retinal circulation time. marked delay in arteriovenous transit time, which is longer than 20 seconds, masking by retinal haemorrhages vessel wall staining. Late staining along the large retinal veins is a characteristic finding in moderate and severe degrees of central retinal vein obstruction. Partial Central Retinal Vein Occlusion V Papillophlebitis OD Pathophysiology of CRVO • Histologic studies suggest that most forms of CRVO have a common mechanism: • thrombosis of the central retinal vein at and posterior to the level of the lamina cribrosa. • In some instances, an atherosclerotic central retinal artery may impinge on the central retinal vein, causing turbulence, endothelial damage, and thrombus formation. • central retinal artery and vein share a common adventitial sheath as they exit the optic nerve head and pass through a narrow opening in the lamina cribrosa. Type 2: Ischemic CRVO is characterized by at least 10 disc areas of retinal capillary nonperfusion on posterior pole view fluorescein angiography also known as nonperfused, complete, or hemorrhagic retinopathy Ischemic CRVO Ischemic CRVO Ischemic CRVO is characterized by rapid onset venous obstruction resulting in decreased retinal perfusion severe visual loss usually less than 20/400 marked afferent pupillary defect Ischemic CRVO • Variable numbers of cotton-wool spots are frequently found as well • The visual prognosis is generally poor in ischemic CRVO, with approximately 10% of eyes achieving vision better than 20/400 • The incidence of iris neovascularization is high (up to 60%) Ischemic CRVO Pathophysiology of CRVO Because of this narrow entry in the lamina cribrosa, the vessels are in a tight compartment with limited space for displacement. This anatomical position predisposes to thrombus formation in the central retinal vein by various factors: Ocular compression of the vein: changes in lamina cribrosa glaucomatous cupping inflammatory swelling in optic nerve orbital compression Virchow's triad for vascular occlusion 1.Hemodynamic disturbances : hyperdynamic or sluggish circulation 2. Vessel wall changes: vasculitis, endothelial damage, arteriosclerosis 3. Changes in the blood: deficiency of thrombolytic factors, increase in clotting factors Pathophysiology of CRVO Occlusion of the central retinal vein leads to: backup of the blood in the retinal venous system and increased resistance to venous blood flow. stagnation of the blood and ischemic damage to the retina. It has been postulated that ischemic damage to the retina stimulates increased production of vascular endothelial growth factor (VEGF) in the vitreous cavity. Increased levels of VEGF stimulate neovascularization of the posterior and anterior segment (responsible for secondary complications of CRVO). It has been shown that VEGF causes capillary leakage leading to macular edema which is the leading cause of visual loss in both ischemic CRVO and nonischemic CRVO. Pathophysiology of CRVO • Unusual diseases that affect clotting mechanisms and blood viscosity may be associated with a CRVO-like picture • Examples include: • blood dyscrasias (polycythemia vera), dysproteinemias, and causes of vasculitis (eg, sarcoidosis, systemic lupus erythematosus), and such hypercoagulable conditions as hyperhomocysteinemia, protein S deficiency, and protein C deficiency. • Oral contraceptives and diuretics have been implicated in CRVO. IschemiC RVO CRVO Systemic risk factors • Patients may have premonitory symptoms of transient • • • • obscuration of vision prior to overt retinal manifestations. Systemic associations noted in the Eye Disease Case-Control Study include : systemic arterial hypertension diabetes mellitus open-angle glaucoma • Increased intraorbital pressure is a • rare but potentially important cause of central vein • hyperlipidemia ? Pathophysiology of CRVO • hyperviscosity retinopathy can mimic a typical CRVO. However, the retinal findings in hyperviscosity retinopathy are generally bilateral and usually related to dysproteinemia such as Waldenstrom macroglobulinemia or multiple myeloma Diagnostic testing includes serum protein electrophoresis and measurements of whole blood viscosity. • In many cases, the hyperviscosity can be reversed by plasmapheresis. Ischemic CRVO Persistent cystoid macular edema in CRVO Hemi retinal vein occlusion Hyperviscosity retinopathy of high altitude Hyperviscosity retinopathy CRVO due to Retinal vasculis Toxoplasma Fulminate retinochoroiditis Retinal vasculitis due to lupus Shaken Baby Syndrome Hematological disorders and other systemic conditions Conditions that lead to increased blood viscosity such as myeloproliferative disorders are uncommon but known to be associated with CRVO. Similarly, a number of rare systemic inflammatory disorders causing systemic vasculitis (such as Behçet’s disease and polyarteritis nodosa) also cause retinal vasculitis leading to RVO, especially in the younger age group. The cause and management of the RVO here is closely linked to the underlying systemic disease and its management. Thrombophilia refers to the propensity to develop thrombosis (usually venous) due to an abnormality in the coagulation system. This can be congenital (eg, Factor V Leiden, hyperhomocysteinemia or protein C, protein S and antithrombin deficiencies) or acquired (eg, antiphospholipid syndrome), and its importance is potentially greater in the younger age group. However Fegan’s review on CRVO and thrombophilia14 suggested that there was a lack of consistency between studies in showing a valid association between CRVO and protein C, protein S and antithrombin III deficiency, and factor V Leiden/activated protein C resistance. In the antiphospholipid syndrome (APS) antibodies to phospholipid activate the coagulation cascade leading to both arterial and venous thrombosis. Tests can be done to either detect the antibody (using the anticardiolipin antibody assay) or its effect on coagulation using a test for lupus anticoagulant. Up to 8% of patients with APS have ocular manifestations and 4 of 8 studies reviewed by Fegan14 showed a significant association of APS in CRVO. Further studies are required to determine the strength of association between APS and RVO. Homocysteine is a naturally occurring amino acid not found in protein. There are many causes for hyperhomo-cysteinemia (including rare enzyme deficiencies leading to homocystinuria) which predisposes to both arterial and venous thrombosis.14 Several studies have questioned the validity of carrying out exhaustive tests for thrombophilia in RVO in the absence of a suggestive medical history. However their results have shown notable evidence of an association of hyperhomocysteinemia with CRVO sufficient to recommend the benefit of checking for hyperhomocysteinemia, which is correctable with folic acid and vitamins B6 and B12 supplements.14–17 On current evidence it would be reasonable to not recommend general thrombophilia screening for all patients with RVO, but to reserve it for older patients with a past history of thromboembolic events and in young patients without any other general risk factors. Conclusion • • • • • • • • The Exact mechanism is nor known Systemic: 1. Vessel wall 2. Hemodynamic 3. Blood Ocular: Glaucoma Anatomical Submit wrt 60 utf-8 hypervisco Types 3 CRVO An intermediate form also exists, but more • than 80% of these eye progress to the severe ischemic form. Pathophysiology of RVO Thrombosis within a retinal vein as described earlier will lead to a partial obstruction of blood flow within the vein and from the eye. The subsequent increased intraluminal pressure, if sufficiently high, will cause transudation of blood products into the retina according to Starling’s law. This will result in increased interstitial (retinal) fluid and protein. The latter will increase the interstitial oncotic pressure which will impede capillary perfusion and lead to ischemia. As stated by Campochiaro et al21 this ischemia is not an all or none dichotomy, as those patients classified as nonischemic will still have varying degrees of retinal ischemia. It is well recognized that inflammation affects the progression and outcome of vitreoretinal disease including retinal vein occlusion.22 Yoshimura et al22 have found significantly elevated vitreous levels of the soluble cytokines interleukin (IL) 6 and 8, monocyte chemoattractant protein-1, and vascular endothelial growth factor (VEGF) in RVO, and especially in CRVO. Funk et al23 have also demonstrated elevated aqueous levels of these same factors in patients with CRVO when compared with control samples. The exact interaction of these factors remains speculative but an understanding of the roles that VEGF fulfils is increasing. It is induced by tissue hypoxia such as retinal ischemia and acts as an angiogenic and vasopermeable factor on endothelial cell membrane bound receptors with tyrosine kinase activity.24 Ozaki et al25 have demonstrated that the implantation of slow release pellets of human recombinant VEGF into the vitreous cavity of rabbits and primates leads to retinal vessel dilatation, breakdown of the blood retinal barrier and retinal new vessel formation. Noma et al have reported elevated aqueous and vitreous levels of VEGF and IL-6 in patients with BRVO26,27 and CRVO,28,29 compared to controls. The levels of VEGF and IL-6 correlated with both the severity of macular edema and extent of retinal ischemia (capillary nonperfusion). It is likely that the sudden retinal ischemia that occurs in BRVO and more so in CRVO will induce excessive VEGF production. VEGF is produced by the retina from retinal pigment epithelial cells, endothelial cells, and Muller cells, as well as other types of ocular tissue.22 Boyd et al found a close correlation between aqueous VEGF levels and the course of iris neovascularization and vascular permeability in patients with ischemic CRVO.30 The excessive vascular permeability induced by VEGF will likely contribute to the macular edema that also occurs according to Starling’s law as described above. It is tempting to theorize that even if the primary venous obstruction was overcome (eg, via collateral formation), the macular edema can persist for much longer due to a self perpetuating cycle of VEGF-induced vascular permeability leading to macular edema, capillary damage, and retinal ischemia, stimulating further release of VEGF and other inflammatory cytokines leading to chronic macula edema. cca c Fundus autofluorescence can detect, in patients with recent-onset CRVO, a perivenular hypoautofluorescence with a fern-like appearance. Retinal Vasculitis due to Lupus stemic Lupus Erythematosis - Vasculitis