Management of Retinal Vascular Occlusions
advertisement

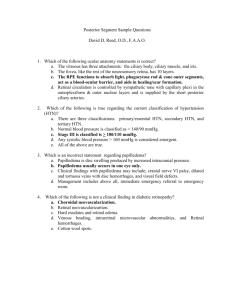
Retinal Vascular Occlusions Joseph Sowka, OD, FAAO, Diplomate Retinal Vascular Occlusive Disease Second most prevalent retinopathy (behind diabetic retinopathy) Strongly associated with systemic disease Prominent morbidity and mortality Anatomy Central retinal vein Single trunk in nerve, but may bifurcate within the substance of the nerve to a dual trunk. Constrict within the lamina cribrosa in order to enter the globe. Drains the retina through 4 tributaries Central retinal artery Feeds the inner 2/3rds of the retina A branch of the ophthalmic artery Parallels the venous arcades Cilioretinal artery is truly a branch of the posterior ciliary artery and not a branch of the central retinal artery as most people think. This is why the cilioretinal artery fills before the central retinal artery on fluorescein angiography. Venous Occlusive Disease Central retinal vein occlusion (CRVO) Hemi-retinal vein occlusion (HRVO) Branch retinal vein occlusion (BRVO) Central Retinal Vein Occlusion Thrombotic phenomenon: Some property of the blood and central retinal vein act in concert to cause thrombotic occlusion. Causes partial or complete blockage of venous return Vein inflammation Vascular flow and/or vessel wall abnormalities stimulate vein thrombosis Hypercoagulability states, elevated viscosity, and systemic states of decreased thrombolysis promote thrombus formation. (i.e., changes in blood constituents) Turbulent blood flow causing thrombus formation at lamina Laminar constriction site is the nidus for occlusion. Intraluminal pressure of the vein decreases, rendering it susceptible to collapse. Compression by an arteriolosclerotic CRA further affects flow and thrombus formation. CRV and CRA share common sheath passing through lamina cribrosa. External factors such as increased IOP in POAG and papilledema (causing increased pressure in the optic nerve sheath) may cause further compression and contribute to occlusion. Other factors that result in compression include: orbital tumor and abscesses, cavernous sinus thrombosis, and retrobulbar intranerve sheath injection. Systemic diseases influence thrombus formation through: 1 1. External compression 2. Primary thrombus formation (Antiphospholipid antibodies) 3. Degenerative or inflammatory disorders of the vein itself Central Retinal Vein Occlusion: Symptoms Blurred vision Loss of visual field Photopsia, in rare cases Asymptomatic (rare: more likely to have asymptomatic BRVO or HRVO) Central Retinal Vein Occlusion: Clinical Signs Dilated, tortuous veins Deep and superficial hemorrhages Disc edema Macular edema Posterior and anterior segment neovascularization Collateral vessels Pre-existing vascular anastomoses in vascular area Collateral circulation is present to some degree in all organ systems. The extent to which collateral circulation prevents ischemia depends upon the time frame of the occlusion and the extent of collateral circulation for that organ and that individual. Bypasses vascular bed occlusion Beneficial- does not leak NaFl on FA Larger caliber than neovascularization Most commonly involves a communication between the retinal veins and the choroidal veins in response to retinal vascular occlusion Clinical Pearl: Acute CRVO may cause angle closure glaucoma due to hemorrhagic choroidal expansion. Central Retinal Vein Occlusion: Causes of Vision Loss Macular edema: this is the prime cause of vision reduction in CRVO. Potentially reversible or treatable RPE atrophy: occurs secondary to chronic macular edema and results in permanent vision reduction. Macular ischemia: presents with severe, irreversible vision loss. This is often the cause when the vision loss is much more dramatic than the clinical picture. Retinal hemorrhage (common) Vitreous hemorrhage (rare) Tractional retinal detachment (rare) Neovascular glaucoma (common) Central Retinal Vein Occlusion: Non-ischemic Majority of cases (about 70%) 2 Acuity >20/200- low risk for neovascularization unless converts to ischemic form Good prognosis 5-20% progress from non-ischemic to ischemic CRVO 83% of ‘indeterminate’ CRVO convert to ischemic CRVO over 4 months Over 3 years, 34% of perfused eyes progressed to ischemic CRVO Central Retinal Vein Occlusion: Ischemic Minority of cases (about 30%) Acuity < 20/200- high risk for neovascularization Initial VA is typically count fingers Extensive superficial hemorrhages Multiple CWS Poor capillary perfusion (10 or more cotton wool spots or 10 DD capillary non-perfusion on fluorescein angiography) Turbid, orange, edematous retina (+) RAPD Poor prognosis Very high risk of neovascularization or the iris and angle and a low/ moderate risk of disc/ retinal neovascularization. Central Retinal Vein Occlusion: Ischemic Vs. Non-ischemic Non-ischemic CRVO will have more dot & blot hemorrhages whereas ischemic will have retinal details obscured by flame-shaped hemorrhages. The presence of cotton wool spots indicates areas of retinal infarct and ischemia. The retina in non-ischemic CRVO will be relatively normal whereas it will be orange, turbid, edematous, and sick looking in ischemic CRVO. Fluorescein angiography: 10 or more disc diameters of retinal non-perfusion on FA define ischemic CRVO. This does not guarantee that the patient will develop neovascular complications, but the odds are that they will. Pupil defects: the ischemic CRVO will have a relative afferent pupillary defect due to destruction of the retina due to non-perfusion. Non-ischemic CRVO will typically not have an APD. Visual acuity: Non-ischemic CRVO typically has acuity > 20/200; ischemic CRVO typically has acuity worse than 20/200 (i.e., finger counting at 2 feet). Clinical Pearl: Most clinicians generally equate an ophthalmoscopically visible CWS with one DD of non-perfusion. Clinical Pearl: Ischemic CRVO typically has vision in the CF range and an afferent pupil defect. If vision is better than 20/200, and there is no APD, then it most likely is nonischemic. Brain teaser: Why is neovascularization of the anterior segment so prevalent in ischemic CRVO while posterior segment neovascularization is so rare? 3 Central Retinal Vein Occlusion: Systemic Considerations Hypertension* Diabetes mellitus* Elevated homocystein levels* Cardiovascular disease (some studies feel that the CRVO pt. has no greater incidence of cardiovascular disease than age matched controls) Hyperviscosity syndromes: Hypergammaglobulinemia, paraproteinemia, hyperfibrinogenemia, cryofibrinogenemia Hyperviscosity states: Malignancy, paraproteinemia, nephrotic syndrome, chronic lung disease, Behcet's disease. AIDS: Infectious vasculitis Collagen vascular disease: Lupus and lupus-like diseases- Antiphospholipid antibodies, common in these diseases, interfere with endothelial cells and prevent interaction with platelets and anticoagulants, thus increasing thrombus formation. Primary antiphospholipid antibody syndrome Same reasons as collagen vascular disease, but phenomenon is primary entity This is the most common cause of CRVO in young healthy adults (under age 50) Syphilis: Infectious vasculitis Sarcoid: Localized vein inflammation Polycythemia (hyperviscosity) Leukemia (blood dyscrasia-hyperviscosity) Autoimmune disease: Infectious vasculitis and antiphospholipid antibodies Oral contraceptive use (causes a potentially hyperviscosity state) Head injuries Carotid artery disease: Slow flow and increased viscosity Hyperlipidemia Mitral valve prolapse Migraine Pressure profusion abnormalities at ONH Retrobulbar compression Sickle cell disease (blood dyscrasia- hyperviscosity) - elevated hematocrit Increased erythrocyte aggregation Decreased plasma volume (causing increased viscosity and erythrocyte aggregation) *Most experts feel that only these conditions must be examined for in the typical elderly vein occlusion patient and that more detailed evaluations should be reserved for special cases such as bilateral cases or in patients who are young (<50 yrs). In younger patients, testing for antiphospholipid antibodies is important. 4 Central Retinal Vein Occlusion: Management Fluorescein angiography: questionable usage. Not appropriate early in the course as fluorescein is blocked by hemorrhage. Pupil testing Retinal photography Gonioscopy to rule out angle neovascularization IOP measurements Co-management with primary care physician to identify and treat any underlying systemic disease Referral to retinologist if NVD, NVE, NVI, NVG (for PRP), or unremitting macular edema develops. Prophylactic PRP to prevent neovascularization inappropriate; therapeutic PRP once neovascularization develops very effective Anti-angiogenic drugs such as Avastin being used successfully off label Laser photocoagulation of macular edema (as for diabetic macular edema) not beneficial in cases of CRVO and hence not done Newest treatment: intravitreal injection of steroids and anti-VEGF drugs (Avastin) for macular edema. Stabilizes vascular membranes and reduces vascular permeability. Very effective Radial optic neurotomy – surgically cutting the nasal disc to decompress this “compartment syndrome” – very radical Clinical Pearl: The main cause of vision reduction in CRVO is macular edema. Clinical Pearl: The most common causes of severe, permanent vision loss in ischemic CRVO are macular infarct and neovascular glaucoma. Clinical Pearl: Ischemic CRVO most commonly forms neovascularization of the iris and angle, and only rarely the posterior segment. Clinical Pearl: A non-ischemic CRVO (or BRVO, HRVO) can convert during their clinical course from a non-ischemic event to an ischemic event. Clinical Pearl: Intravitreal injections of steroids and anti-VEGF drugs are being investigated and used for edema secondary to vascular occlusions, diabetes, cystoid macular lesions, and wet age related macular degeneration. Clinical Pearl: New understanding of autoimmunity suggests that young patients with CRVO be tested for primary antiphospholipid antibody syndrome, especially if there are no other concurrent conditions present Hemi- Retinal Vein Occlusion Historically has been considered a variant 5 of branch retinal vein occlusion. Pathophysiologically, it most closely resembles CRVO. In terms of natural history and neovascular complications, it most closely resembles BRVO. Involves superior or inferior drainage only May be ischemic (23%), non-ischemic (67%), or indeterminate (10%) Photograph and monitor q1mos until resolution Fluorescein angiography: Not useful early in the course because fluorescein is blocked by the hemorrhage. Questionable usefulness. Directed internal medicine consultation to evaluate systemic health. If patient has diseases known to be associated with vascular occlusive disease and patient is already being managed medically, send internist a letter detailing patient's ocular status. Non-ischemic HRVO has very little propensity to develop neovascularization Ischemic HRVO has a high propensity to develop neovascularization of the disc/ retina and a low/ moderate risk to develop neovascularization of the iris and angle. Clinical Pearl: HRVO develops most like CRVO, but behaves most like BRVO. Brain Teaser: Ischemic HRVO most typically develops neovascularization of the disc and retina and only rarely of the iris. Why is anterior segment neovascularization so rare in HRVO, while posterior segment neovascularization is much more so common? Clinical Pearl: The main cause of vision reduction in HRVO is macular edema. Clinical Pearl: The most common causes of severe, permanent vision loss in patients with HRVO are macular infarct and tractional retinal detachment. Branch Retinal Vein Occlusion Occurs at arteriovenous crossing Most commonly superiotemporal Arteriolosclerotic etiology: as the arteriole becomes sclerotic, it compresses the underlying venule leading to thrombus formation and leakage from the capillary beds draining into the venule. At no time in vascular occlusion does the vein or venule ever leak. All leakage is from the capillaries. Vein compression will lead to turbulent blood flow, which damages the endothelium and sets the stage for platelets, thrombin, and fibrin to form a thrombus. May present with loss of acuity and/or field, but may be asymptomatic There are three location classification for BRVO 1. Hemispheric Before the first bifurcation. Technically HRVO 2. Intermediate After the first bifurcation. Typical BRVO appearance 3. Twig Macular area only 6 Branch Retinal Vein Occlusion: Ischemic 20-30% of cases VA < 20/200 typically Both blot and flame shaped hemorrhages Cotton wool spots Macular edema (this is the most common cause of vision loss in BRVO) NVD; NVE; vitreous hemorrhage: tractional retinal detachment common (as cause of permanent severe vision loss). NVI, NVG are rare in BRVO (for the same reasons as in HRVO). Macular capillary non-perfusion may occur with devastating vision reduction which is irreversible Ischemic BRVO is defined as 5 disc diameters of retinal capillary non-perfusion on fluorescein angiography. Branch Retinal Vein Occlusion: Non-ischemic 70-80% of cases VA > 20/200 typically Blot, flame shaped hemorrhages Rare CWS Mild macular edema Collateral vessel formation Branch Retinal Vein Occlusion: Causes of Vision Loss Macular edema (most common cause and typically reversible)-any form Macular capillary non-perfusion (perifoveal capillary loss) - ischemic Vitreous hemorrhage- ischemic Tractional retinal detachment- ischemic Rarely NVG- ischemic In terms of neovascularization, BRVO behaves most like HRVO in that the neovascularization is predominately in the posterior segment and rare in the anterior segment. BRVO Study Group: Findings Macular edema: 3-18 month window of opportunity to treat Do not treat macular hemorrhage Treat only if VA < 20/40 and due to macular edema Prophylactic treatment to avoid neovascularization not indicated- only treat with PRP after neovascularization forms. As mentioned earlier, macular edema secondary to BRVO is increasingly being addressed by intravitreal steroid and anti-VEGF injections. Clinical Pearl: The main cause of vision reduction in BRVO is macular edema. 7 Clinical Pearl: Ischemic BRVO most typically develops neovascularization of the disc and retina and only rarely of the iris. Clinical Pearl: The most common causes of severe, permanent vision loss in patients with BRVO are macular infarct and tractional retinal detachment. Clinical Pearl: You can have an ischemic BRVO (and possibly HRVO) with good acuity and no RAPD (but they aren’t common). Branch Retinal Vein Occlusion: Systemic Associations Hypertension: 70% of cases- most commonly associated medical condition Diabetes Atherosclerosis Hyperlipidemia Blood hyperviscosity Carotid artery disease Coronary artery disease Branch Retinal Vein Occlusion: Management Referral to internist for directed work-up Monitor q1mos until resolution of hemorrhages Monitor q4-6 months for the next three years 50%-60% will have 20/40 or better vision without treatment Possible fluorescein angiography Retinal photography Retinologist only if complications develop (neovascularization or unremitting macular edema with vision loss) Laser photocoagulation for macular edema Steroid/ anti-VEGF injection for macular edema PRP/ anti-VEGF injection for neovascularization Arteriovenous sheathotomy The overlying artery is separated from the vein with a microvitreoretinal blade. A pars plana vitrectomy is first performed (surgical removal of the vitreous). An incision is then made in the adventitial sheath adjacent to the arteriovenous crossing, and is extended along the membrane that holds the blood vessels in position to the point where they cross. At this point, the blade is used to separate adhesions holding the artery to the vein. The artery is then lifted away from the vein. Cutting the sheath around the vessels and physically separating them where they cross should improve blood flow through the vein. Unanswered questions: Timing? Advantages of sheathotomy vs vitrectomy alone vs intravitreal injections vs natural untreated history? An option for those patients with macular edema unremitting to other treatments 8 Clinical Pearl: There is a window of opportunity of 3-18 months in which to treat macular edema in BRVO and HRVO. Clinical Pearl: In BRVO and HRVO, only treat macular edema if vision is worse than 20/40. The Standard Care Vs. COrticosteroid for REtinal Vein Occlusion (SCORE) Study The SCORE Study will compare the effectiveness and safety of standard care to intravitreal injection(s) of triamcinolone for treating macular edema associated with CRVO and BRVO. Arterial Occlusive Disease Central retinal artery occlusion (CRAO) Ophthalmic artery occlusion Cilioretinal artery occlusion Branch retinal artery occlusion (BRAO) Carotid artery disease (CAD) and Ocular Ischemic Syndrome (OIS) Central Retinal Artery Occlusion: Clinical Picture Painless, sudden loss of monocular vision Vision is count fingers to hand motion to no light perception Retinal edema causing white appearance to fundus Mean age is 60's Cherry red macula due to underlying choriocapillaris perfusion and lack of overlying structures within this area. Optic atrophy ensues eventually Central Retinal Artery Occlusion: Pathophysiology Etiology is typically emboli from carotid artery or heart lodging in central retinal artery at laminar constriction. Emboli of cardiac origin are more likely than emboli of carotid origin to cause artery occlusion Other possible etiologies: Giant cell arteritis (GCA) Intraluminal thrombosis Hemorrhage under atherosclerotic plaque Vasospasm Dissecting aneurysm Hypertensive arteriolar necrosis Circulatory collapse Clinical Pearl: In 2-10% of cases, the cause is thrombosis formation due to giant cell arteritis. If the cause is GCA, bilateral involvement can occur in hours to days. GCA must always be considered as a cause of CRAO in the elderly! 9 Ophthalmic Artery Occlusion: Compare and Contrast to CRAO NLP vision Cherry red spot not present More severe retinal whitening Systemic associations similar to CRAO, but much higher incidence of GCA Cilioretinal Artery Occlusion: Local infarcted area Severe loss of central acuity with preservation of peripheral field Systemic causes similar to CRAO Higher incidence of GCA, especially if concurrent AION exists Central Retinal Artery: Heroic Treatment Paracentesis to reduce IOP and allow less compression on CRA to allow emboli to pass further. Carbogen Patient is hospitalized and breathes Carbogen 5-10 minutes every hour for 24 hours. Using pure oxygen is worse because there will be a reflex constriction of the blood vessels. Carbogen increases CO2 levels, which causes a rebound vasodilation. Digital massage to transiently elevate IOP and have rebound IOP decrease and subsequent arterial dilation Breathing into a brown paper bag in order to increase blood CO2 levels. Fibrinolytic agents (clot-busters: urokinase, streptokinase) 1-24 hour window of opportunity Treatment vs no treatment: 1/4 line difference in Snellen acuity. Overall, heroic measures do not affect final visual acuity (only anecdotal success). If the cause is inflammatory thrombosis from GCA, these heroic measures will do nothing because there is no embolus to dislodge. Clinical Pearl: In patients over the age of 60 years, CRAO may be caused by giant cell arteritis. You must get an ESR and C-reactive protein on every patient over the age of 60 years with CRAO because if the cause is GCA, the patient will progress to bilateral vision loss in hours to days. Clinical Pearl: GCA more commonly causes ophthalmic artery occlusions and especially cilioretinal artery occlusions than CRAO. ESR and C-reactive protein are mandatory in these patients over 60 years. Central Retinal Artery Occlusion: Systemic Considerations General atherosclerosis Arterial hypertension Diabetes Carotid atherosis Cardiac/ cardiovascular disease 10 Giant cell arteritis Infectious endocarditis Cardiac valvular disease Rheumatic heart disease Mitral valve prolapse Mural thrombus after MI Atrial myxoma IV drug use Lipid emboli Pancreatitis Purtscher's retinopathy Head, neck, retrobulbar corticosteroid injections HZV Migraine Malignancy Trauma Hyperlipidemia Syphilis Mucormycosis Hemoglobinopathy Sickle cell disease Oral contraceptives Platelet and clotting factor abnormalities Systemic lupus erythematosus Antiphospholipid antibodies cause prolonged partial thromboplastin time Primary antiphospholipid antibody syndrome Polyarteritis nodosa Homocystinuria Pregnancy Optic disc drusen Prelaminar compression of CRA, leading to turbulence and thrombus formation Associated conditions can cause CRAO through several mechanisms: 1. Contributing to emboli formation 2. Trauma (via compression, vasospasm, or direct vessel damage) 3. Coagulopathies 4. Collagen vasculopathies 5. Inflammation (GCA) 6. Other (idiopathic) Age-related Differences: Abnormalities Associated with CRAO in Patients Under 30 Years: Atherosclerosis very rare Migraine Coagulation abnormalities 11 Primary antiphospholipid antibody syndrome Cardiac abnormalities Trauma Sickling hemoglobinopathies Optic nerve head drusen Central Retinal Artery Occlusion: Complications CVA Myocardial infarction: main cause of death Low survivorship: 9 year mortality of 56% (compared to 17% in age matched group) Neovascularization uncommon (17% of cases and occurs within 4 weeks) Central Retinal Artery Occlusion: Management Stat ESR/ C-reactive protein if over 60 years old Co-management with primary care physician to identify and treat any underlying systemic disease Cardiology referral Monitor for complications Q3mos Heroic measures generally not helpful Branch Retinal Artery Occlusion: Visible retinal emboli lodged in arteriole Cholesterol Calcific Fibrin-platelet Infectious Rarely caused by GCA Acuity 20/20 to hand motion depending upon the degree of involvement (macula) Patients commonly report sudden onset of field loss Whitened retina in distribution of arteriole With resolution, retina becomes more normal in appearance (but not function) Neovascularization is rare Systemic associations same as CRAO, but lower survivorship Cardiology referral Clinical Pearl: BRAO has even lower survivorship than CRVO. Clinical Pearl: BRAO is only rarely caused by GCA because the vessels are too small. Clinical Pearl: Retinal vein occlusions are more likely to cause neovascularization than retinal artery occlusions. The reason is that vein occlusions starve the retina of oxygen, leading to VEGF release while artery occlusions destroy the retinal tissue and VEGF isn’t released nearly as much in response. 12 Arterial Occlusion Conclusion: The good news is that the patient won't have a stroke. The bad news is that they will die of a heart attack first. Vision loss is devastating and irreversible Beware GCA Cardiology referral is most appropriate Low survivorship Clinical Pearl: Retinal artery occlusion management in a nutshell: Stat ESR and Creactive protein if over 60 years, blood pressure measurement, fasting blood sugar and 2 hour post-prandial blood glucose, carotid Doppler and carotid evaluation, cardiology referral. Ocular Ischemic Syndrome (OIS): Internal carotid artery atheromatous ulceration and stenosis at bifurcation of common carotid artery 5% of internal carotid artery stenosis pts. develop OIS Occurs only if stenosis > 90%. With 90% stenosis, you only drop down to 50% perfusion in CRA. Males : females 2:1 Occurs in 50's to 80's ages-most commonly 60's Occurs bilaterally 20% of cases Etiology of findings related to low arterial pressure and flow to the eye. Reduction in blood flow through hemodynamic insufficiency Chronic sx’s: Diminished vision in bright light Choroidal insufficiency causing photoreceptor metabolism compromise Pain Progressive vision loss Ocular Ischemic Syndrome: Posterior Segment Clinical Findings Dilated, but not tortuous, retinal veins. Tortuosity is a sign of venous obstruction (CRVO). Dot/blot hemorrhages Typically in mid-periphery (can extend to posterior pole) Arise from capillary leakage due to ischemic endothelial damage As arterial pressure is abnormally low, there is not sufficient impetus to push blood along vascular system, so blood pools in capillary network Hemorrhages are usually scattered whereas they are more confluent in CRVO Microaneurysms Macular edema Cotton wool spots Possible cherry red spot (due to retinal hypoperfusion, not embolization) Spontaneous arterial pulsation IOP exceeds pressure within CRA 13 If not observed spontaneously, can be induced with light digital pressure 1/3rd of cases have NVD, NVE Vitreous heme and tractional RD may occur from NVD, NVE 90% of cases of OIS who develop NVI have count fingers vision within 1 year Appears similar to a mild CRVO or diabetic retinopathy In differentiating OIS from CRVO: Veins are dilated and tortuous in CRVO. Veins are dilated, but not tortuous in OIS Hemorrhages are patchy and mid-peripheral in OIS. Hemorrhages are closer to posterior pole and more confluent in CRVO In differentiating OIS from Diabetic Retinopathy Diabetic retinopathy is symmetric. OIS is typically unilateral and therefore gives asymmetric retinopathy. Whenever encountering asymmetric retinopathy, think vein occlusion and/or OIS. Exudates are common in DR, rare in OIS Hemorrhages are mid-peripheral in OIS, posterior pole in DM Clinical Pearl: Whenever encountering asymmetric retinopathy, always think carotid occlusive disease and OIS. Ocular Ischemic Syndrome: Anterior Segment Findings Cornea edema Cataract Unilateral or asymmetric Due to prolonged ischemia 20% of cases have anterior chamber reaction- always keep this condition in the back of your mind when you treat uveitis. Don't confuse this with uveitis as uveitis is typically uncommon in an elderly patient Uveitis is typically mild and frequently asymptomatic and associated with low IOP Unilateral/ipsilateral red eye As blood is shunted from the internal carotid to the external carotid system, there is secondary congestion of conjunctival and episcleral vessels. NVI and NVA Seen in 50% of cases of OIS May progress to NVG However, most eyes are often hypotonous due to ischemia and poor perfusion to CB with resultant aqueous hyposecretion Secondary angle closure (without pupil block) and PAS with fibrovascular tissue Clinical Pearl: OIS can be caused by GCA in elderly patients. Clinical Pearl: You can easily diagnose OIS from the anterior segment findings without looking in the posterior segment to see the characteristic retinopathy. In fact, cataract often prevents retinal visualization in these patients. 14 Ocular Ischemic Syndrome: Systemic Considerations High systemic morbidity Arterial hypertension in 73% of cases Diabetes in 56% of cases Ischemic heart disease in 50% of cases Stroke in 25% of cases Peripheral vascular disease in 20% of cases GCA Collagen vascular disease Coagulopathies Hypercholesterolemia Cardiac death is #1 cause of mortality Ocular Ischemic Syndrome: Treatment and Management Optimal treatment is truly unknown PRP will cause regression of anterior segment vessels in 36% of cases- not nearly as good as in diabetic retinopathy. The more closed the angle, the less successful the PRP will be. Endarterectomy (carotid Roto-Routering) if less than 99% stenosed. 1/3 improve 1/3 stable 1/3 worsen 15