Carcinomas - Mammary Gland Tumors

Carcinomas
Wendy Blount, DVM
Carcinomas
• Squamous cell carcinoma (canine & feline)
• Transitional cell carcinoma (canine)
• Mammary Gland Tumor (canine & feline)
• Perianal tumor (canine)
• Anal sac tumors (canine)
Squamous Cell Carcinoma
Feline Squamous Cell carcinoma
• Second most common tumor in the cat
• Oral SCC behaves differently than skin SCC
Canine Squamous Cell Carcinoma
• Similar behavior as SCC in cats, but not as common
Squamous Cell Carcinoma
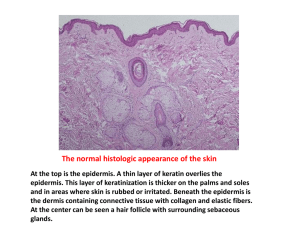
Feline Cutaneous Squamous Cell Carcinoma
• Most frequently on the head
– Pinnae, nose, eyelids
• Caused by sun exposure to light colored skin
• Progression over time
– Solar dermatitis – crusts and scabs
– Actinic dermatitis - plaques
– SCC in situ – noninvasive mass
– Invasive SCC – ulcerative, invasive mass
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
Solar dermatitis
Actinic dermatitis
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
SCC n situ
SCC
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
• Cytology often not helpful
– Very inflammatory
• Dx - histopathology
• Staging not usually necessary, as metastasis is rare
• Tx – early lesions
– Surgery, cryosurgery, Strontium radiotherapy, photodynamic therapy
– immunomodulatory agent imiquimod (Aldara TM ) as a topical cream
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
• Tx – advanced lesions
– Difficult to treat
– Removal of the nasal planum is possible, but disfiguring
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
Partial planectomy
Pinnectomy and planectomy
Squamous Cell Carcinoma
Feline Cutaneous Squamous Cell Carcinoma
Untreated for too long
Squamous Cell Carcinoma
Feline Oral Squamous Cell Carcinoma
• Most common oral tumor in the cat
• Gingiva, tongue/sublingual, tonsil
• Much more aggressive than cutaneous SCC
• Maxillary tumors can mimic tooth abscess
• Surgery often not possible
• Radiation sensitive, but high morbidity – mandatory feeding tube
Squamous Cell Carcinoma
Feline Oral Squamous Cell Carcinoma
• Chemotherapy not effective
• NSAIDs are palliative
• Median survival 44 days + NSAIDs
• 9% survival at one year
• Survival more than a few months even with multimodal therapy is rare
Squamous Cell Carcinoma
Feline Lung Squamous Cell Carcinoma
• Often presents as multiple nail bed tumors
• Primary tumor is found on chest x-rays
• Always take chest x-rays prior to amputating a possibly neoplastic nail bed in a cat
• Animals with systemic neoplasia often do not do well under anesthesia
• Amputation is palliative only
Transitional Cell Carcinoma
• Most common bladder tumor in the dog (90%)
• Most common symptoms are hematuria and stranguria
• Things that increase suspicion
– Atypical transitional cells in the urine sediment
– Mass in the bladder or urethra on imaging
– Thickened urethra on rectal exam
– Ruptured urethra on catheterization
Transitional Cell Carcinoma
Etiology
• Exposure to older topical flea treatments, dips and lawn chemicals (28x)
• Possibly cyclophosphamide therapy
• Neutered > sexually intact
• Scottish terriers 18-20x other dog breeds
– Eating vegetables 3x a week is protective
• Shelties, Westies, beagles 3-5x other breeds
Transitional Cell Carcinoma
Dx – histopath
• Surgery, cystoscopy, traumatic bladder wash
• Percutaneous aspiration can seed tumor cells and should be avoided
• Take care to avoid seeding during surgery
Transitional Cell Carcinoma
Tx
• At one time, radiation therapy was recommended, as TCC is highly responsive
– But resulting permanent incontinence was common
• If at the apex, resection can produce long disease free interval (1-2 years)
• Secondary UTI is common – treat PRN
• Ureteral stents can restore urine flow
• Urethral stents can relieve obstruction if urethral sphincter and continence can be preserved
• Prepubic cystostomy tube can relieve obstruction
Transitional Cell Carcinoma
Tx - NSAIDs
• Mainstay of treatment is medical therapy
• Not curative, but remission is achieved in 15-20% and stable disease is reached in 75% of dogs
• Piroxicam only – median survival 195 days
– 0.3 mg/kg PO SID to QOD
• Deramaxx only - median survival 323 days
– 3 mg/kg PO SID
• Previcox similar success
• Median survival surgery only is 109 days
Transitional Cell Carcinoma
Tx - Chemo
• Mitoxantrone and piroxicam (see chemo section for details)
– 35% remission with minimal toxicity
– Median survival 291 days
• Single agent vinblastine (see MCT notes)
– 36% remission
– 50% stable disease
– Most of these had failed other therapies
– Relatively more toxicity than mitoxantrone + piroxicam
Transitional Cell Carcinoma
Px
• Euthanasia often due to obstruction, metastasis or both
• 50% have metastasis at the time of death
• Some will invade the sublumbar lymph nodes and then the spinal cord and present as acute posterior paralysis, often with urethral obstruction
Canine Mammary Gland Tumor
• 42% of tumors in all intact female dogs
• Rare in dogs less than 5 years old
• duration of exposure to ovarian hormones early in life determines the overall mammary cancer risk (Dorn et al, 1968).
– 0.5% if OHE prior to the first heat
– 8 if OHE prior to the 2 nd heat
– 26% if OHE after the 2 nd heat
• tumor risk increases incrementally each year and plateaus around 11–13 (Schneider, 1970)
• intact females are more likely to have an anaplastic tumor type, compared to dogs spayed early or late in life, prior to MGT (Ogilvie, 2006)
Canine Mammary Gland Tumor
The effect of neutering on the risk of mammary tumours in dogs--a systematic review. J Small
Anim Pract. June 2012;53(6):314-22. W
Beauvais 1 ; J M Cardwell; D C Brodbelt
Due to the limited evidence available and the risk of bias in the published results, the evidence that neutering reduces the risk of mammary neoplasia, and the evidence that age at neutering has an effect, are judged to be weak and are not a sound basis for firm recommendations.
Canine Mammary Gland Tumor
• Review article – not a clinical study at all
• Conclusions:
– 9/13 were judged to have a high risk of bias. The remaining four were classified as having a moderate risk of bias.
– One study found an association between neutering and a reduced risk of mammary tumours.
– Two studies found no evidence of an association.
– One reported "some protective effect" of neutering on the risk of mammary tumours
Canine Mammary Gland Tumor
• 70% have more than one tumor at the time of diagnosis
• Mammary gland tumors can be epithelial, myoepithelial, mesenchymal or mixed
• Complex MGT – epithelial and myoepithelial
• Mixed MGT – epithelial and mesenchymal
Canine Mammary Gland Tumor
MGT Stages
• Stage I – less than <3cm and localized
• Stage II – 3-5 cm and localized
• Stage III - >5cm and localized
• Stage IV – any size, metastasis to lymph node
• Stage V – any size, distant metastasis
Canine Mammary Gland Tumor
MGT Staging
• CBC – check for evidence of infection
• Profile – hypercalcemia
• Aspirate draining lymph node
• Thoracic radiographs – 3 views
• Abdominal US
Canine Mammary Gland Tumor
MGT Staging
• CBC – check for evidence of infection
• Profile – hypercalcemia
• Aspirate draining lymph node
• Thoracic radiographs – 3 views
• Abdominal US
Canine Mammary Gland Tumor
Surgery
• As with all masses removed, label margins so they can be read out
– Describe the location of the lesion
– Mark one end of one direction (e.g., cranial or caudal) with one type suture
– Mark one end of the plane 90 O to above with another type suture, if necessary
– Don’t forget to describe your labeling on the submission form
Canine Mammary Gland Tumor
Surgery – OHE?
• The majority of MGT of epithelial origin express estrogen receptors, suggesting that reproductive hormones may play a role in the pathogenesis
• 755 days median survival - dogs spayed at or within 2 years before MGT surgery
• 286 days median survival – dogs not spayed at MGT surgery
• 301 days median survival – dogs spayed more than 2 years prior to MGT surgery
MGT are uncommon in females spayed more than 2 years prior to MGT, but if it occurs, it behaves more malignantly
Canine Mammary Gland Tumor
Prognosis
• 50-60% of mammary gland tumors are benign
• 98% of tumors <1 cm are benign
• 50% of tumors >3cm are malignant
• Malignant tumors develop from benign masses
• Early removal is usually curative
Canine Mammary Gland Tumor
Inflammatory Mammary Carcinoma
• Acute onset of painful, extensive swelling of the mammary glands
• Fine needle aspiration with a 25g needle can drip blood for days (DIC)
• Rapidly progressive
• Grave prognosis
Perianal Tumors
• “aka” hepatoid tumor
• Most common in older intact male dogs
– And females with testosterone producing adrenal tumors
• Tumor site – perineum > tail, abdomen
• Most often found without symptoms
• Tenesmus can be caused by the lesion or submandibular lymphadenopathy (palpable rectally)
• 60-80% benign
• Those that are malignant often behave as anal sac tumors
Perianal Tumors
• Staging prior to surgery
– Abdominal rads and/or sonography to evaluate sublumbar lymph nodes
• Large tumors >2cm and single tumors should be removed
• If multiple small tumors or coalescing tumors, castrate first (if male)
– Remove any tumors that do not resolve in 2-4 weeks
• Unless males are castrated, new tumors will likely arise
Anal Sac Carcinoma
• Highly malignant
– Locally invasive AND distant metastases
• 90% develop hypercalcemia
– 25-50% are hypercalcemic at diagnosis
• 50-94% have lymph node metastasis at the time of diagnosis
Anal Sac Carcinoma
Presentation
• Found on anal sac expression
• Dyschezia, tenesmus, ribbon-like stools
• Attention to the perineum, scooting
• Perianal bleeding
• PU-PD (hypercalcemia)
• Hind limb weakness or posterior paralysis
• May be bilateral – check the other side
Anal Sac Carcinoma
Staging
• Profile – hypercalcemia, azotemia
• Abdominal rads and/or sonography
– Sonography more sensitive than rectal palpation or rads for finding enlarged sublumbar LN
• Thoracic radiographs – 3 views
• Aspirate popliteal and inguinal lymph nodes
– Sublumbar if large enough and you are comfortable doing this with ultrasound guidance
Anal Sac Carcinoma
Median Survival – no treatment
• 7-9 months
– masses larger than 3cm
– Dogs with hypercalcemia and/or pulmonary metastasis
• 18-19 months
– Masses smaller than 3cm
– Dogs with normocalcemia and no lung mets
Anal Sac Carcinoma
Median Survival
• Surgery only
– 90% survival at 6 months (hypercalcemia often goes into remission, even if incomplete excision)
– 65% survival at one year
– 29% survival at 2 years
– 20% temporary fecal incontinence, some permanent
– Wound infection and sepsis can occur
– 30% perioperative fatality when sublumbar lymph nodes are removed
Anal Sac Carcinoma
Median Survival
• Multi-modal therapy – surgery, radiation of nodes, doxorubicin/carboplatin
– 18-26 months median survival
– 86% survival at 6 months (less than surgery alone)
– 69% survival at one year (same as surgery alone)
– 36% survival at 2 years (more than surgery alone)
– 14% survival at 3 years
• Median survival 22 months with radiation alone
– 15% rectal structure
Acknowledgements
• Jane M. Dobson, MA, BVetMed, DVetMed, DECVIM-
CA&Onc, MRCVS
Department of Veterinary Medicine, University of
Cambridge, Cambridge, UK
• Deborah W. Knapp, DVM, DACVIM (Oncology)
Purdue University, West Lafayette, IN, USA
• Karin Ulrikke Sorenmo, DVM, DACVIM, DECVIM-CA
(Oncology)
Veterinary Hospital of the University of Pennsylvania
Philadelphia, PA, USA
Acknowledgements
• Erik Teske, DVM, PhD, Dip ECVIM-CA
Clinical Sciences, Companion Animals
Utrecht University, THE NETHERLANDS
• Katherine Skorupski, DVM, DACVIM (Oncology)
Assistant Professor of Clinical Medical Oncology
University of California, Davis
• Greg Ogilvie, DVM, DACVIM (Oncology)
Director, Angel Care Cancer Center, California