FEES
advertisement

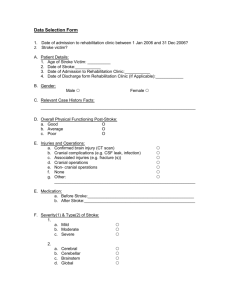
STROKE AND FIBEROPTIC ENDOSCOPIC EVALUATION OF SWALLOWING (FEES) IN A CANADIAN ACUTE CARE SETTING AJAY MYSORE NARASIMHA Key Learning Goals 1. Appreciating the benefits of FEES in an acute care setting 2. Usefulness of FEES in acute stroke 2 London Health Sciences Centre: Did You Know? • One of Canada’s largest acute care teaching hospitals • Serves the needs of the London- Middlesex community • Provides the broadest range of patient services of any hospital in Ontario • More than one million patient visits each year 3 LHSC: Speech-Language Pathology (S-LP) • 12.5 FTE S-LPs at two sites University Victoria Hospital Hospital 4 Pre-FEES: Assessment of Adults with Dysphagia • Clinical Assessment • Instrumental Assessment: Modified Barium Swallow (MBS) 5 MBS: Challenges • Exposure to radiation • Environmental Factors: Use of barium ? Naturalistic • Patient factors: Transportation Medical fragility Positioning Education • Reports 6 MBS: Challenges • Number of appointment times 12 Victoria Hospital 11 University Hospital • Wait times • Limited times • Physician consent 7 NPO: A Tough Sell • For the patient: Patient quality of life Tube feeding and equipment Nursing time “Burden” of care Discharge destination and timing • For the team: “This is holding up discharge” “How are we going to give medications?” “If he is aspirating, can it be tolerated?” 8 How were we going to solve this? 9 10 Systems Thinking “Systems thinking organizes complexity into a coherent story that illuminates the causes of problems and how they can be remedied in enduring ways” ~ Peter Senge 11 Systems Thinking 101 “Integrative thinkers build models rather than choose between them • Consider customers, employees, competitors, capabilities, cost structures, industry evolution, and regulatory environment • View the problem as a whole, rather than breaking it down and farming out the parts • Creatively resolve tensions without making costly trade-offs, turning challenges into opportunities" http://www.rotman.utoronto.ca/ • 12 So How Does this FEES Initiative Fit With “Systems Thinking”? 13 Systems Thinking and FEES Complex Situation Shared Reality – Shared Vision Surfaced Assumptions Leveraged Actions Significant Change 14 FEES: The Proposal • Capital equipment proposal • Collaboration with Otolaryngology and Respirology Dr. Kevin Fung Dr. David Leasa • Potential benefits of FEES 15 Approval…What Next? • Finding equipment Request for tender Review of equipment Procurement of a FEES system • Establishing a process Nasendoscopy (Delegation vs. Directive) Nasendoscopy training…where, when, how, with whom FEES: procedures and documentation format • Executing the training Use of and transition to independence • Selecting the paradigm Autonomy and efficiency 16 Medical Directive • Education and skills to complete nasendoscopy • Indications and contraindications • Risks, complications and solutions 17 Where Are We Now? • All SLPs achieved competency between September 2012 - January 2013 • Continued use of FEES in the clinical setting 18 THE STROKE JOURNEY 24 ER SWALLOWING SCREEN WITHIN 24 HRS HOURS FAIL PASS 72 SLP CONSULT HOURS ORAL DIET BEDSIDE SWALLOWING AX FEES MBS 19 ACUTE STROKE DYSPHAGIA SCREENING TOOL 20 CANADIAN BEST PRACTICE STROKE GUIDELINES Patient has to be screened within first 24 hours of admission (Evidence Level C) Instrumental assessment should be performed on all patients with high risk for aspiration or based on bedside swallowing assessment , stroke location (brainstem stroke etc.) or other clinical features (e.g., multiple strokes etc.) (Evidence Level B) The decision to proceed with tube feeding should be made within 72 hours/3 days of admission in collaboration with patient, family or Substitute Decision maker and inter-professional team. (Evidence Level B) 21 FEES IN ACUTE STROKE DYSDYSPHAGIA AND PNEUMONIA The reported incidence of dysphagia in acute stroke with instrumental assessment is 64% to 78% . (Martino et.al 2005) Incidence of pneumonia in acute stroke 16% to 19% (Martino et.al 2005) The risk of pneumonia dysphagia > without dysphagia, dysphagia +confirmed aspiration > dysphagia without aspiration (Martino et.al 2005) > 3 fold increase in pneumonia risk in stroke patients with dysphagia (Martino et.al 2005) 22 FEES IN ACUTE STROKE SENSITIVITY AND SPECIFICITY Good inter- and intra-rater reliability between FEES and MBS on Rosenbek Penetration and Aspiration Scale (Kelly et al, 2007) Incidence of pneumonia was significantly lower with FEES than MBS in stroke patients (Aviv, 2000) FEES has better outcome (behavioral and dietary) in stroke as it readily identifies fatigue of the pharyngeal phase and effect of fatigue (Aviv, 2000) 23 FEES IN ACUTE STROKE SAFETY FEES could be performed within 48 hours of onset of stroke symptoms >80% of patients reported no or mild discomfort during FEES (Warnecke et.al, 2008) 24 FEES IN ACUTE STROKE AADVANTAGES OF FEES Immediate and repeated assessments Better visualization and information regarding sensory/afferent component compared to MBS (Aviv 2000) Can be used as a bio-feedback tool Able to assess secretion management Visualization of anatomic soft tissue , anomalies (e.g., vocal cord paralysis etc.) Portable to bedside Test patients who are difficult to position or transport 25 FEES Truisms FEES TRUISMS 26 Discharge Facilitated CASE STUDY 1 • 71 year old female with history of kyphosis from NH • Right Middle Cerebral Artery (MCA) stroke, dense left hemiplegia, unilateral Upper Motor Neuron (UMN) dysarthria on Thursday night • Not a TPA candidate • Failed dysphagia screening due to left facial droop • Seen by SLP Friday a.m. for a clinical swallowing assessment inconsistent clinical signs of penetration/aspiration therefore NPO recommended • Kyphosis preclude positioning for an MBS • Also, no MBS slot until Tuesday • FEES completed Friday afternoon – patient initiated on a pureed solids with regular thin liquids • NG tube was avoided • Discharged to stroke rehab – day 5 27 Bio-Feedback Tool in Treatment CASE STUDY 2 • 55-year-old man post brainstem stroke with subsequent tracheostomy due to aspiration of secretions • Admitted to the ICU • Dysphagia managed by nasogastric tube • Able to follow directions and participate in therapy to rehabilitate the swallow • Repeated FEES studies completed with the goal of providing biofeedback/visualization • First step, learning to swallow secretions and utilizing a volitional cough to laryngeal vestibule • Decannulation in one week with improvement in secretion management • Second step, within two week, patient learned chin tuck maneuver and initiated a full fluid diet • Nasogastric tube removed 28 The Story So Far…. 29 Questions 1. How has FEES influenced the number of patients receiving MBSs? 2. How has FEES influenced the number of swallowing referrals? 3. How has FEES impacted the use of instrumental assessments? 4. How has FEES impacted inter-professional care ? 30 Why? Fees fever picture 31 How has FEES impacted interprofessional care ? • Results perceived as more “credible” • Greater agreement with recommendations • Better understanding of the swallowing impairment • Recognition for contributing towards access and flow • “You can do that today?!” • Enhanced professional profile empowerment staff 32 Future Directions for our Department Related to: 1. FEES 2. Clinical Excellence 33 Future Directions Related to FEES: 1. Setting up our tool kit with on site staff training 34 Future Directions Related to FEES: 1. Incorporation into the student placement experience 2. New staff: A different training model 3. Data collection: Trends through statistics 4. Research opportunities 35 Future Directions Related to Clinical Excellence: 1. Carry over to other disorders • Continue case studies 2. Carry over to other projects • Model 36 In Summary • Fees proven to be a useful method of performing instrumental assessments in in and outpatients across multiple patient populations especially in Acute Stroke. • FEES has been found to be an alternative to MBS and can be utilized effectively in the acute care setting • FEES may allow for early optimal assessment for stroke patients with medical fragility, dependence on the ventilator, difficulty with positioning, or fatigability • Quicker instrumental assessment for stroke patients resulting in earlier swallowing/nutrition plans and facilitating discharge to most appropriate medical setting (e.g., rehab) • The initiation of FEES has influenced MBS usage at LHSC • The reduction of MBS usage has the potential to reduce costs for the organization 37 Acknowledgments • Drs. Fung and Leasa who provided tremendous support, expertise, and time in assisting us with the introduction of “FEES” at LHSC • Dr. Vanessa Burkoski for recognizing the impact of FEES on patient care and supporting this significant financial investment • Donna Bandur for seeing the potential in FEES and championing this initiative 38 References • Acceptance of Delegation of a Acceptance of Delegation of a. (2008). Retrieved September 1, 2013, from CASLPO OAOO: http://www.caslpo.com/Portals/0/positionstatements/mpsdeleg.pdf • A Guide to Medical Directives and Delegation. (n.d.). Retrieved September 1, 2013, from Federation of Health Regulatory Colleges of Ontario: http://www.regulatedhealthprofessions.on.ca/WHOWEARE/default.asp • Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110:563-574 • Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: How do videofluroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007; 117:1723-1727. • Leder SB, Sasaki CT, Burrell MI. Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia. 1998;13:19-21 • Lindsay, M. P., Gubitz, G., Bayley, M., & Philips, S. (2013). Canadian Best Practices and Recommendations for Stroke Care. Canadian Stroke Best Practices and Standard Group. Retrived from http://www.strokebestpractices.ca/wpcontent/uploads/2010/10/Ch4_SBP2013_Acute-InpatientCare_22MAY13_EN_FINAL4.pdf. 39 References • Langmore SE, Schatz K, Olsen N. endoscopic and videofluoroscopic evaluation of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100:678-681 • Langmore, S. E. (2001). Endoscopic Evaluation and Treatment of Swallowing Disorders. New York: Thieme NewYork. • Leder, S. A. (2005). Fiberoptic Endoscopic Evaluation of Swallowing (FEES) with and without Blue-Dyed Food. Dysphagia, 157-162. • Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: Incidence, Diagnosis, and Pulmonary Complications. Stroke. 2005;36:2756-2763. • Senge, P. (1990). The fifth discipline: the art and practice of the learning organization. New York: Doubleday. Steele, C. M. (2008). Practice Standards and Guidelines for Dysphagia Intervention by Speech-Language Pathologists. Retrieved September 1, 2013, from CASLPO OAOO: http://www.caslpo.com/Portals/0/ppg/Dysphagia_PSG.pdf Wu CH, Hsaio TY, C CJ, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: Comparison with videofluoroscopic technique. Laryngoscope. 1997;107:396-401 40
![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)