Kim Johnson
advertisement

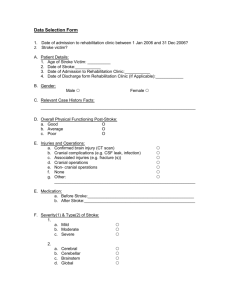
Kimberly Johnson, MD, PGY-2 HPI Middle aged male who presented to the ED with dizziness and was found to have blood pressure of 297/132. He was admitted for hypertensive crisis and started on a nitro drip and later switched to a cardene drip. On HD #1, patient woke with trouble swallowing, feeling dizzy when sitting up and having double vision that improved when he closed one eye On assessment patient was thought to have possible left eye lid droop. Neurology was stat consulted. Cont HPI PMH: Smoking for 25 years ( 1.5 ppd) MEDS: On admission no medications. On transfer to neurology: amlodipine and aspirin, lovenox, Family history: DM, Hypertension Social history: Worked in construction Physical Exam General: Well nourished obese gentleman in no acute distress HEENT: NCAT, Nares Patent, Trachea midline Cardiac: RRR, no murmurs heard Resp: CTA bilaterly Neurological Exam Mental Status: Awake, alert, oriented x4 Speech: Able to name, repeat, comprehend, with moderate dysarthria Cranial Nerves: Significant for right sided miosis, left side equally reactive to light, EOMI, visual field/acuity normal. Decreased temp sensation on right side of face. TRAP/SCM strength 5/5, palate raises symmetrically, tongue midline. Motor Strength: Normal bulk and tone with 5/5 strength throughout in upper and lower extremities. DTRs: 2+ in bicep, tricep,brachielradialis,patellar, 1+ in ankles, toes downgoing bilaterally Sensation: Normal light touch throughout, decreased temperature on left arm Coordination: Finger to nose intact, heel to shin slow, but intact Gait: Feeling unsteady, leaning to the right, able to ambulate with walker Where What MRI findings Wallenberg Syndrome • First described in Dr. Vieusseux in 1808, then by Dr. Adolf Wallenberg in 1895 clinically and 1901 by autopsy. • Caused by occlusion of the posterior inferior cerebellar artery or a branch off the vertebral artery • Most commonly affected arteries in order are Vertebral, PICA, Superior middle and inferior medullary artery. •This is the most common Posterior circulation infarct Lateral medullary syndrome (location) symptoms Vestibular Nuclei Vomiting, vertigo, nystagmus Inferior cerebellar peduncle Ipsilateral ataxia, dysmetria past pointing Central tegmental tract Palatal myoclonus Lateral Spinothalamic tract Contralateral deficits in pain and temperature sensation, limbs and torso Spinal trigeminal nucleus Ipsilateral loss of pain and temp in face Nucleus ambiguus Ipsilateral laryngeal, pharyngeal, palatal hemiparalysis, dyphagia, diminished gag reflex Descending sympathetic fibers Ipisilateral Horner’s syndrome (ptosis, miosis, and anhydrosis) Lateral medullary syndrome (location) symptoms Vestibular Nuclei Vomiting, vertigo, nystagmus Inferior cerebellar peduncle Ipsilateral ataxia, dysmetria past pointing Central tegmental tract Palatal myoclonus Lateral Spinothalamic tract Contralateral deficits in pain and temperature sensation, limbs and torso Spinal trigeminal nucleus Ipsilateral loss of pain and temp in face Nucleus ambiguus Ipsilateral laryngeal, pharyngeal, palatal hemiparalysis, dyphagia, diminished gag reflex Descending sympathetic fibers Ipisilateral Horner’s syndrome (ptosis, miosis, and anhydrosis) Nucleus ambiguus The nucleus ambiguus (literally "ambiguous nucleus") Located dorsal (posterior ) to inferior olivary nucleus in the lateral portion of upper medulla. Recieves UMN innervation directly via corticobulbar tract. Nucleus gives rise to branchial efferent fibers of Vagus N, (Innervating laryngeal, pharyngeal and uvulae muscles) Also efferent motor fibers of Glossopharyngeal N. (Innervating stylopharyngeus muscle) and Accessory N (Laryngeal muscles as well) Wallenberg Syndrome and Dysphagia Dysphagia is a disorder of deglutition. Affects Oral, Pharyngeal, and/or Esophageal phases of swallowing. Estimates of the incidence vary widely from 29% to 81% Specifically for Lateral Medullary infarcts vary from 55 % 100% Aspiration was found to range from 22 – 55%, with nearly half of these being silent aspirations. Nutritional needs post stroke have been shown to have significant affects on recovery. Table 1: Micronutrients and mechanisms through which their deficiencies induce cerebrovascular alterations and increase the risk of stroke. Back to our patient’s dysphagia Patient had Video Swallow Oral Stage Summary*: Patient had significant difficulty with PO intake, coughing, and poor management of secretions. Pharyngeal Stage Summary*: Pharyngeal stage characterized by delayed swallow initiation with the bolus head in the pyriforms for tsp of nectar thick liquid. Overall movements of the swallow were considered inconsistent which may be due to etiology of the stroke (brain stem) but also due to frequent movement, coughing, expectoration due to reduced management of secretions. Prognosis*: Fair Dysphagia Rating*: Moderately-Severe Dysphagia -Not able to swallow safely by mouth for nutrition/hydration but may take some consistency w/ consistent max cues in therapy only. Alternative method of feeding required. Penetration Aspiration Scale*: Material enters laryngeal vestibule, passes below vocal folds & no effort is made to eject PEG tube placed on HOD #7. Continued Speech therapy. Our patient’s story continued. Repeat swallow study on Post stroke day 15 patient was able to take Mechanical soft, with nectar thickened liquids. Taking in <50% of calories to maintain adequate nutrition. Patient discharged home with PEG tube in place, with plan for removal 2 weeks after discharge. Patient will Outpatient Speech therapy but was uninsured and has not been seen yet in follow up. Conclusion Dysphagia is a common consequence of lateral medullary infarcts. Consequence of dysphagia is aspiration, with 50% being silent, with patient’s facing the complication of aspiration pneumonia PEG tube placement vs NG tubes Patient’s will regain their ability to be able to have oral nutrition adequate for their needs Understanding malnutrtion and its role in stroke recovery is critical in our patients returning to their pre-stroke quality of life. References Bath PMW, Bath-Hextall FJ, Smithard D. Interventions for dysphagia in acute stroke (Review). The Cochrane Library 2009, Vol. 1 M Dennis, S Lewis, G Cranswick and J Forbes, on behalf of the FOOD Trial Collaboration. FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke. Health Technology Assessment 2006; Vol. 10: No. 2 ANTHONY J, KAPIL K, A. BARNEY H. Long-term outcome of percutaneous endoscopic gastrostomy feeding in patients with dysphagic stroke. Age and Ageing 1998; 27: 671 -676 Bouziana SD Tziomalos K. Malnutrition in Patients with Acute Stroke. Journal of Nutrition and Metabolism Volume 2011, Article ID 167898, 7 pages Marik PE and Kaplan D. Aspiration Pneumonia and Dysphagia in the Elderly*, Chest 2003;124;328-336 Gloss D, Weisberg L. Neurlogy for the Specialty Boards, 2007, 1st Edition http://www.neuroanatomy.wisc.edu/virtualbrain/BrainStem/09NA.html Frequency of Vascular Occlusive lesions in a registry of posterior circulation infarcts Artery Frequency Innominate artery 0.7% (2) Subclavian artery 1.9% (5) ECVA 43.5% (113) ICVA 41.5% (108) Basilar artery 41.8% (109) PCA 15% (39) Includes only lesions of the first portion of the ECVA. Distal ECVA dissections were not included. Transverse section of the upper medulla