DR.Mohammed Awad
Incidence
The most common cause of cancer mortality
in both sex (1/3 of cancer deaths)
About 90% of lung cancer mortality among
men (and 80% among women) is attributable
to smoking.
Non-small-cell lung cancer (NSCLC) accounts
for 80% of all cases.
Risk Factors
Cigarette, pipe, or cigar smoking.
Exposure to second-hand smoke, radon,
arsenic, asbestos, chromates, chloromethyl
ethers, nickel, polycyclic aromatic
hydrocarbons, radon progeny, other agents,
and air pollution.
Radiation therapy to the breast or chest.
Risk Factors Cont.
For smokers, the risk for lung cancer is on average tenfold
higher than in lifetime nonsmokers.
The risk increases with the quantity of cigarettes,
duration of smoking, and starting age.
Smoking cessation results in a decrease in precancerous
lesions and a reduction in the risk of developing lung
cancer.
Former smokers continue to have an elevated risk for lung
cancer for years after quitting.
Asbestos exposure may exert a synergistic effect of
cigarette smoking on the lung cancer risk
Screening
In patients considered at high risk for
developing lung cancer, no screening
modality for early detection has been shown
to alter mortality.
Studies of lung cancer screening with chest
radiography and sputum cytology have failed
to demonstrate that screening lowers lung
cancer mortality rates.
Screening Cont.
Published studies of newer screening
technologies such as low-dose computed
tomography (CT) scans and biomarker screenings
report primarily on lung cancer detection rates
and do not present sufficient data to determine
whether the newer technologies will benefit or
harm people.
Currently, randomized trials are evaluating lowdose spiral CT scanning.
Squamous cell carcinoma.
Adenocarcinoma.
Large cell carcinoma.
Adenosquamous carcinoma.
Carcinomas with pleomorphic, sarcomatoid, or
sarcomatous elements.
Carcinoid tumor.
Carcinomas of salivary-gland type.
Unclassified carcinoma
Staging and Risk Assessment
Complete history and physical examination,
CT scan of the chest and upper abdomen.
MRI of the brain if abnormal neurologic
findings (can be substituted by CT scan)
Bone scan in the presence of bone pain,
elevated serum calcium, or elevated alkaline
phosphatase levels.
Patients With Potentially Curative
Treatment
Biopsy of mediastinal lymph nodes 1 cm in short axis.
Biopsy of mediastinal lymph nodes can be obtained by
mediastinoscopy, transbronchial needle aspiration, ultrasound-guided
bronchoscopy with fine needle aspiration, and /or endoscopic
esophageal ultrasound-guided fine needle aspiration.
MRI of the brain for clinical stage III patients (to be substituted by CT
scan if MRI not available) planned for definitive local treatment.
Bone scan for clinical stage III patients planned for definitive local
treatment.
In patients with a single metastatic lesion on imaging studies, biopsy
should be attempted to prove metastatic.
Cytology of pleural / pericardial effusions in patients otherwise
curatively treatable.
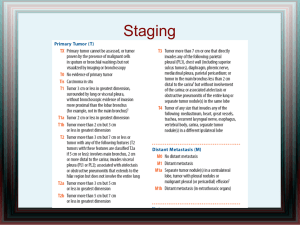
Staging According To The UICC 6
System
Primary tumor (T)
T1: A tumor that is 3 cm or
T2: A tumor with any of the following features:
Larger than 3 cm in greatest dimension
Involves the main bronchus and is 2 cm or
larger distal to the carina
Invades the visceral pleura
Associated with atelectasis or obstructive
pneumonitis that extends to the hilar region
but does not involve the entire lung
T3: A tumor of any size that directly invades any of the
following: chest wall (including superior sulcus tumors),
diaphragm, mediastinal pleura, parietal pericardium; or,
tumor in the main bronchus less than 2 cm distal to the
carina but without involvement of the carina; or,
associated atelectasis or obstructive pneumonitis of the
entire lung
T4: A tumor of any size that invades any of the following:
mediastinum, heart, great vessels, trachea, esophagus,
vertebral body, carina; or, separate tumor nodules in the
same lobe; or, tumor with a malignant pleural effusion
Regional lymph nodes (N)
N1: Metastasis to ipsilateral peribronchial
and/or ipsilateral hilar lymph nodes and
intrapulmonary nodes
N2: Metastasis to ipsilateral mediastinal
and/or subcarinal lymph node(s)
N3: Metastasis to contralateral mediastinal,
contralateral hilar, ipsilateral or contralateral
scalene, or supraclavicular lymph node(s)
Distant metastasis (M)
M0: No distant metastasis
M1: Distant metastasis present [Note: M1
includes separate tumor nodule(s) in a
different lobe (ipsilateral or contralateral).
Stage IA
T1 N0 M0
Stage IB
T2 N0 M0
Stage IIA
T1 N1 M0
Stage IIB
T2 N1 M0
T3 N0 M0
Stage IIIA
T1, T2 N2 M0
T3 N1, N2 M0
Stage IIIB
Any T N3 M0
T4 Any N M0
Stage IV
Any T Any N M1
Treatment of Localized
Disease
Surgical resection in functionally fit patients
(lobectomy/pneumonectomy plus systematic
mediastinal lymph node sampling or
lymphadenectomy).
Cisplatin-based adjuvant combination chemotherapy
is recommended in stage II and IIIA and can be
considered in selected stage IB patients (T > 4 cm).
Preoperative cisplatin-based combination
chemotherapy can be considered in patients with
stage IIIA–N2 disease
Treatment of Localized
Disease Cont.
Postoperative radiotherapy may be considered in patients
not radically resected, and can be considered for patients
with resected stage IIIA disease.
Curative conformal radiotherapy as a single modality is to
be considered in patients unfit for standard surgery.
Platinum-based chemotherapy, preferably concurrent with
thoracic radiotherapy, is the standard treatment for
selected patients with locally advanced, unresectable
stage III NSCLC and adequate pulmonary function.
Stage I
Lobectomy or segmental, wedge, or sleeve
resection as appropriate.
Radiation therapy with curative intent (for
potentially resectable tumors in patients with
medical contraindications to surgery).
Cisplatin-based adjuvant combination
chemotherapy can be considered in selected
stage IB patients (T > 4 cm).
Stage I Cont.
Clinical trials of adjuvant chemoprevention
(beta carotene, retinol, 13-cis-retinoic acid,
[alpha]-tocopherol, N-acetylcysteine, or
acetylsalicylic acid).
Endoscopic photodynamic therapy and other
endobronchial therapies (under clinical
evaluation)
Stage II (T1/T2 N1 or T3N0)
Lobectomy; pneumonectomy; or segmental,
wedge, or sleeve resection as appropriate.
Radiation therapy with curative intent (for
potentially operable tumors in patients with
medical contraindications to surgery).
Adjuvant chemotherapy after curative
surgery.
Adjuvant Chemotherapy
The first adjuvant chemotherapy for NSCLC was performed
in the 1960s using a key drug known as cyclophosphamide.
In the 1980s and early 1990s, a new anti-cancer drug,
cisplatin, was developed. The first meta-analysis of this
drug was conducted by the Non-small Cell Lung Cancer
Collaborative Group in 1995. This analysis comparing
surgery with surgery plus chemotherapy containing
cisplatin produced a hazard ratio of 0.87 and suggested an
absolute benefit of chemotherapy of 5% at 5 years; this
difference was not statistically significant (p0.08).
Several clinical trials of adjuvant chemotherapy were planned after the
meta-analysis conducted in 1995, but the efficacy of adjuvant
chemotherapy remained a matter of controversy. However, useful
evidence was reported after 2003. The International Adjuvant Lung
Cancer Collaborative Group Trial (IALT) demonstrated a 4.1%
improvement in survival for patients with stage I to III NSCLC.
The JBR trial demonstrated a 15% improvement in 5-year survival for
the adjuvant chemotherapy arm in stage IB or II (excluding T3N0)
patients. The Adjuvant Navelbine International Trialist Association
(ANITA) trial reported that the overall survival at 5 years improved by
8.6% in the chemotherapy arm and that this survival rate was
maintained at 7 years (8.4%) in stage II and IIIA patients.
A meta-analysis based on collected and pooled individual patient data
from the 5 largest randomized trials was conducted by the Lung
Adjuvant Cisplatin Evaluation (LACE). A 5-year absolute benefit of 5.4%
from Adj chemotherapy. The benefit varied with stage (test for trend,
P = .04; HR for stage IA = 1.40; p>0.05; HR for stage IB = 0.93; p>0.05;
HR for stage II = 0.83; 95% p<0.05; and HR for stage III = 0.83 p<0.05).
The effect of chemotherapy did not vary significantly (test for
interaction, P = .11) with the associated drugs, including vinorelbine (
HR = 0.80; 95% CI, 0.70–0.91), etoposide or vinca alkaloid (HR = 0.92;
95% CI, 0.80–1.07), or other (HR = 0.97; 95% CI, 0.84–1.13). The greater
effect on survival observed with the doublet of cisplatin plus
vinorelbine. Chemotherapy effect was higher in patients with better
PS.
Alternatively, uracil-tegafur has been
developed and tested in Japan. The Japan
Lung Cancer Research Group (JLCRG) on
Postsurgical Adjuvant Chemotherapy reported
a 5-year overall survival advantage of 11% in
the uracil-tegafur group patients with stage
IB cancer. The efficacy of adjuvant
chemotherapy with uracil-tegafur was
confirmed in a meta-analysis.
Stage III A
Patients with stage IIIA NSCLC are a heterogenous
group. Patients may have metastases to ipsilateral
mediastinal nodes or potentially resectable T3
tumors invading chest wall or mediastinal
involvement with metastases to peribronchial or
hilar lymph nodes (N1). Presentations of disease
range from resectable tumors with microscopic
metastases to lymph nodes to unresectable, bulky
disease involving multiple nodal stations.
Stage III A
If complete resection of tumor and lymph
nodes was achieved, such patients benefit
from postoperative adjuvant chemotherapy.
Neoadj Chemotherapy followed by surgery
Combined chemoradiotherapy for inoperable
cases.