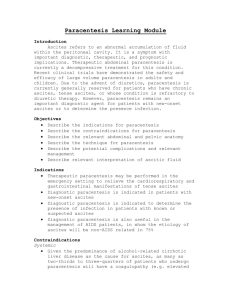
Paracentesis and Ascites Fluid Analysis
advertisement

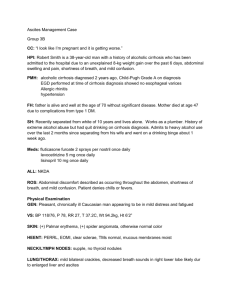
Paracentesis and Ascites Fluid Analysis Stephen Y. Chang, M.D. June 16, 2002 THE PROCEDURE: A relatively simple bedside procedure in which one inserts a needle into the abdomen, thereby evacuating either a small amount of ascites fluid for diagnostic purposes, or large amounts of fluid for therapeutic purposes. It is the most cost-effective means of determining the cause of ascites. INDICATIONS: 1. Above all, anyone (in- or outpatient) with new-onset ascites should have at least a diagnostic paracentesis. 2. Many authors advocate tapping anyone admitted to the hospital with ascites. 3. Anyone with ascites who is showing signs/symptoms of infection, especially fever, hypotension, peripheral leukocytosis, encephalopathy, acidosis. CONTRAINDICATIONS: Really, very few contraindications at all. 1. Coagulopathy stands as one relative contraindication, but keep in mind that most cirrhotics with ascites have a concomitant coagulopathy (reflected by an elevated INR). Very few of them will bleed unless the needle actually enters a blood vessel (which is a rare event). Incidentally, there are NO studies to support giving FFP or other blood products prior to paracentesis to reduce bleeding complications. 2. DIC or evidence of fibrinolysis is considered by some authors to be an absolute contraindication to paracentesis. RISKS: When you talk with the patient or proxy to get consent for the procedure, remember to discuss with them the following risks of the procedure: 1. Abdominal wall hematoma (rare, only about 2% of cases in some studies) 2. Infection (also extremely rare to get it from paracentesis; some studies report ZERO infections related to the procedure) 3. Bleeding There have been studies of paracentesis complications, and none of them report any deaths associated with the procedure itself. TOOLS: You’ll need the following… 1. A large bore Angiocath needle (around 16-18 gauge usually suffices for large volume taps; 20-22 is fine for a diagnostic). Avoid the short Angiocaths (less than 3.5 inches), as these often won’t be long enough to get good access into the peritoneal space 2. A thoracentesis kit. Out of this, you will use the long tubing provided to drain fluid into collection bottles in large volume paracentesis. And, in the occasional situations where an Angiocath is not effective, you may need to use the ‘harpoon’ long needle used in thoracentesis for access instead. Always make sure you familiarize yourself with the instruments in the kit and how the stopcocks work before you start your procedure! 3. 4. 5. 6. Betadine and sterile gauze 1 or 2% Lidocaine and a 25 gauge needle and 5cc syringe for infiltration Chux to keep the bed clean A gown and mask for yourself (the fluid is often under pressure, and it can spurt out the needle a good distance!). Always remember that with any procedure, you should be wearing eye/splash protection. 7. Sterile gloves 8. Collection bottles – if doing a large volume paracentesis, you may need up to 6-7 bottles (1 liter each) TECHNIQUE 1. Get consent from either the patient or the patient’s health care proxy. 2. Position the patient, either supine or, more commonly, in the lateral decubitus position favoring the side where you intend to insert the needle. The usual sites to tap are RLQ or caudal to the umbilicus (if the patient is thin). 3. Elevate the head of the bed slightly 4. Percuss the abdomen to determine where the fluid level exists 5. Clean the skin thoroughly with Betadine solution 6. Infiltrate the skin and subcutaneous tissues with lidocaine via the 25 gauge needle and wait about 3-5 minutes for the lido to take effect. 7. Insert the Angiocath or thoracentesis needle with a syringe attached at your chosen site perpendicular to the skin. As you advance your needle slowly, aspirate intermittently until you get fluid return. Continuous aspiration has the theoretical risk of vacuum suctioning bowel and omentum towards the needle. 8. Once flow is obtained, remove the needle leaving the catheter in place. Collect at least 20-30cc for your lab tests and cultures (into blood culture bottles – 5-10cc’s each bottle). 9. If performing a therapeutic paracentesis, then disconnect your syringe and attach the tubing to the catheter, with another needle at the other end of the tubing. This needle is used to insert into the vacutainer collection bottles (1 liter each). TECHNIQUE (con’t) : Remember to send at least the following routine ascites labs: 1. Cell count and differential 2. LDH 3. Albumin 4. Culture in blood culture bottles inoculated at the bedside ALSO remember to send a serum LDH and albumin at the same time (or at least from the same day)!!! INTERPRETING ASCITES FLUID Cell Count: There is no ‘standardized’ ascites fluid cell count Generally accepted ‘cut-off’ for upper-limits of normal for infection is less than 250 PMNs/mm3 PMNs usually constitue 70% of the cell count. In spontaneous bacterial peritonitis, for example, PMNs are the predominant line. In tuberculous ascites, you’ll see a lymphocytic predominance. Bloody ascites fluid is usually the result of the procedure itself, ie traumatic tap The Serum-Ascites Albumin Gradient: The concept surrounds oncotic-hydrostatic balance Simple calculation: Serum albumin – Ascites albumin= SAAG SAAG > 1.1 mg/dl SAAG < 1.1 mg/d Cirrhosis Alcoholic Hepatitis Cardiac Ascites “Mixed Ascites” Massive Liver Metastasis Fulminant Hepatic Failure Budd-Chiari Syndrome Portal Vein Thrombosis Veno-Occlusive Disease Myxedema Fatty Liver of Pregnancy Peritoneal Carcinomatosis Tuberculous Peritonitis Pancreatic Ascites Bowel Obstruction Biliary Ascites Nephrotic Syndrome Posteroperative Lymphatic Leak Serositis in Connective Tissue Disease Reproduced from Feldman et al, ed: Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 6th edition Exudates, Transudates and Ratios: We are always taught in medical school that the serum:ascites LDH and protein ratios help differentiate exudates and transudates The literature shows that these calculations are actually not all that helpful, surprisingly. The SAAG has become more favored in helping to characterize ascites fluid. Amylase: “Normally” in ascites, you see an ascites amylase that’s about half the serum amylase If the ascites is secondary to pancreatitis or perforated viscus, the amylase levels can be as great as five-fold higher than the serum levels Glucose: In uncomplicated ascites, usually similar to serum levels. In later SBP (but often not in early), ascites glucose levels can drop to as low as zero mg/dl secondary to bacterial consumption Cultures and Gram Stains: Cultures should be obtained by inoculating blood culture bottles at the bedside. This has been shown to improve sensitivity to at least 80%, compared with 50% for ‘conventional’ culture methods. Gram stains are relatively useless on ascites fluid – about as useful as asking for a Gram stain on blood cultures to look for bacteremia. The concentration of organisms just won’t be high enough to see something on Gram stain. Cytology Truly only helpful in diagnosing peritoneal carcinomatosis. Reported sensitivities up to 100%. Does not detect most other intra-abdominal cancers, mainly because most of the other cancers do not frequently metastasize to the peritoneum. Think of cytology as helping you only if you’re suspicious of a cancer that has spread to the peritoneum. And remember that a negative cytology does not rule out cancers such as hepatocellular carcinoma or liver metastases, which commonly cause ‘malignant ascites.’