Con - cnsgroup11
advertisement
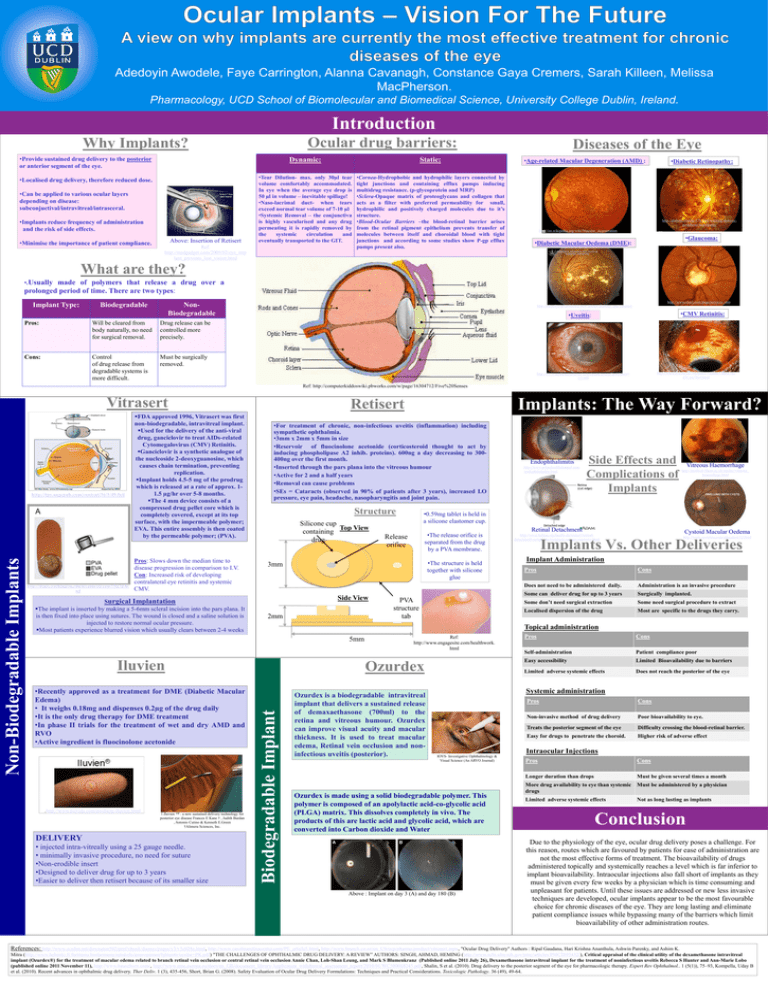
EFFECT OF ENVIRONMENT AND CLOZAPINE ON BASAL AND STIMULATED MEDIAL PREFRONTAL GABA RELEASE IN TWO Adedoyin Awodele,RAT Faye Carrington, Alanna Cavanagh, Constance Gaya Cremers, Sarah Killeen, Melissa MODELS OF SCHIZOPHRENIA MacPherson. Pharmacology, UCD School of Biomolecular and Biomedical Science, University College Dublin, Ireland. Introduction Ocular drug barriers: Why Implants? •Provide sustained drug delivery to the posterior or anterior segment of the eye. Dynamic: Static: •Localised drug delivery, therefore reduced dose. •Tear Dilution- max. only 30µl tear volume comfortably accommodated. In eye when the average eye drop is 50 µl in volume – inevitable spillage! •Naso-lacrimal duct- when tears exceed normal tear volume of 7-10 µl •Systemic Removal – the conjunctiva is highly vascularised and any drug permeating it is rapidly removed by the systemic circulation and eventually transported to the GIT. •Cornea-Hydrophobic and hydrophilic layers connected by tight junctions and containing efflux pumps inducing multidrug resistance. (p-glycoprotein and MRP) •Sclera-Opaque matrix of proteoglycans and collagen that acts as a filter with preferred permeability for small, hydrophilic and positively charged molecules due to it’s structure. •Blood-Ocular Barriers –the blood-retinal barrier arises from the retinal pigment epithelium prevents transfer of molecules between itself and choroidal blood with tight junctions and according to some studies show P-gp efflux pumps present also. •Can be applied to various ocular layers depending on disease: subconjuctival/intravitreal/intrasceral. •Implants reduce frequency of administration and the risk of side effects. •Minimise the importance of patient compliance. Above: Insertion of Retisert Ref: http://medgadget.com/2009/02/eye_imp lant_prevents_lost_vision.html Diseases of the Eye •Age-related Macular Degeneration (AMD) : •Diabetic Retinopathy: http://diabetestesting-578.com/warning-diabeticperipheral-neuropathy http://en.wikipedia.org/wiki/Macular_degeneration •Glaucoma: •Diabetic Macular Oedema (DME): What are they? •.Usually made of polymers that release a drug over a prolonged period of time. There are two types: Implant Type: Biodegradable http://www.otm1.com/page/services_otm NonBiodegradable Pros: Will be cleared from body naturally, no need for surgical removal. Drug release can be controlled more precisely. Cons: Control of drug release from degradable systems is more difficult. Must be surgically removed. http://od.pcli.com/articles/a-new-doctor/diabetes-and-cataractsurgery •CMV Retinitis: •Uveitis: http://www.eyesite.ca/7modules/Module7/html/Mo d7Case7Ref.html http://www.medicinenet.com/script/main/art.asp?articlekey= 121809 Ref: http://computerkiddoswiki.pbworks.com/w/page/16304712/Five%20Senses Vitrasert http://depts.washington.edu/hivaids/oit/case7/fig7d.ht ml Pros: Slows down the median time to disease progression in comparison to I.V. Con: Increased risk of developing contralateral eye retinitis and systemic CMV. Surgical Implantation The implant is inserted by making a 5-6mm scleral incision into the pars plana. It is then fixed into place using sutures. The wound is closed and a saline solution is injected to restore normal ocular pressure. Most patients experience blurred vision which usually clears between 2-4 weeks •For treatment of chronic, non-infectious uveitis (inflammation) including sympathetic ophthalmia. •3mm x 2mm x 5mm in size •Reservoir of fluocinolone acetonide (corticosteroid thought to act by inducing phospholipase A2 inhib. proteins). 600ng a day decreasing to 300400ng over the first month. •Inserted through the pars plana into the vitreous humour •Active for 2 and a half years •Removal can cause problems •SEs = Cataracts (observed in 90% of patients after 3 years), increased I.O pressure, eye pain, headache, nasopharyngitis and joint pain. Structure Silicone cup Top View containing drug 2mm Iluvien .http://www.psivida.com/products-iluvien.html 1.Iluvien ™ : a new sustained delivery technology for posterior eye disease Frances E Kane † , Judith Burdan , Antonio Cutino & Kenneth E.Green †Alimera Sciences, Inc. DELIVERY • injected intra-vitreally using a 25 gauge needle. • minimally invasive procedure, no need for suture •Non-erodible insert •Designed to deliver drug for up to 3 years •Easier to deliver then retisert because of its smaller size http://www.primehealthchannel.com /endophthalmitis.html Side Effects and Complications of Implants Vitreous Haemorrhage http://medweb.bham.ac.uk/easdec/vitreous_ hemorrhage.html Release orifice PVA structure tab Retinal Detachment Cystoid Macular Oedema http://www.beltina.org/health-dictionary/retinaldetachment-symptoms-treatment-surgery-recovery.html http://www.mvretina.com/education/12.html Implants Vs. Other Deliveries Implant Administration Pros Cons Does not need to be administered daily. Administration is an invasive procedure Some can deliver drug for up to 3 years Surgically implanted. Some don’t need surgical extraction Some need surgical procedure to extract Localised dispersion of the drug Most are specific to the drugs they carry. Topical administration 5mm •Recently approved as a treatment for DME (Diabetic Macular Edema) • It weighs 0.18mg and dispenses 0.2µg of the drug daily •It is the only drug therapy for DME treatment •In phase II trials for the treatment of wet and dry AMD and RVO •Active ingredient is fluocinolone acetonide •The release orifice is separated from the drug by a PVA membrane. •The structure is held together with silicone glue Side View Endophthalimitis •0.59mg tablet is held in a silicone elastomer cup. 3mm Ref: http://www.engagesite.com/healthwork. html Ozurdex Biodegradable Implant Non-Biodegradable Implants http://tpx.sagepub.com/content/36/1/49.full FDA approved 1996, Vitrasert was first non-biodegradable, intravitreal implant. Used for the delivery of the anti-viral drug, ganciclovir to treat AIDs-related Cytomegalovirus (CMV) Retinitis. Ganciclovir is a synthetic analogue of the nucleoside 2-deoxyguanosine, which causes chain termination, preventing replication. Implant holds 4.5-5 mg of the prodrug which is released at a rate of approx. 11.5 µg/hr over 5-8 months. The 4 mm device consists of a compressed drug pellet core which is completely covered, except at its top surface, with the impermeable polymer; EVA. This entire assembly is then coated by the permeable polymer; (PVA). Implants: The Way Forward? Retisert Ozurdex is a biodegradable intravitreal implant that delivers a sustained release of demaxaethasone (700ml) to the retina and vitreous humour. Ozurdex can improve visual acuity and macular thickness. It is used to treat macular edema, Retinal vein occlusion and noninfectious uveitis (posterior). Pros Cons Self-administration Patient compliance poor Easy accessibility Limited Bioavailability due to barriers Limited adverse systemic effects Does not reach the posterior of the eye Systemic administration Pros Cons Non-invasive method of drug delivery Poor bioavailability to eye. Treats the posterior segment of the eye Difficulty crossing the blood-retinal barrier. Easy for drugs to penetrate the choroid. Higher risk of adverse effect Intraocular Injections IOVS- Investigative Ophthalmology & Visual Science (An ARVO Journal) Ozurdex is made using a solid biodegradable polymer. This polymer is composed of an apolylactic acid-co-glycolic acid (PLGA) matrix. This dissolves completely in vivo. The products of this are lactic acid and glycolic acid, which are converted into Carbon dioxide and Water Above : Implant on day 3 (A) and day 180 (B) Pros Cons Longer duration than drops Must be given several times a month More drug availability to eye than systemic drugs Must be administered by a physician Limited adverse systemic effects Not as long lasting as implants Conclusion Due to the physiology of the eye, ocular drug delivery poses a challenge. For this reason, routes which are favoured by patients for ease of administration are not the most effective forms of treatment. The bioavailability of drugs administered topically and systemically reaches a level which is far inferior to implant bioavailability. Intraocular injections also fall short of implants as they must be given every few weeks by a physician which is time consuming and unpleasant for patients. Until these issues are addressed or new less invasive techniques are developed, ocular implants appear to be the most favourable choice for chronic diseases of the eye. They are long lasting and eliminate patient compliance issues while bypassing many of the barriers which limit bioavailability of other administration routes. References: http://www.oculist.net/downaton502/prof/ebook/duanes/pages/v3/v3c028a.html, http://www.carolinaretinacenter.com/PE_article5.html, http://www.bausch.co.nz/en_US/ecp/pharma/product/vitrasert.aspx, "Ocular Drug Delivery" Authors : Ripal Gaudana, Hari Krishna Ananthula, Ashwin Parenky, and Ashim K. Mitra (http://www.helsinki.fi/farmasia/biofarmasia/opiskelu/provopinnot/bjktentti/ocular+PK.pdf) "THE CHALLENGES OF OPHTHALMIC DRUG DELIVERY: A REVIEW” AUTHORS: SINGH, AHMAD, HEMING (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2895432/), Critical appraisal of the clinical utility of the dexamethasone intravitreal implant (Ozurdex®) for the treatment of macular edema related to branch retinal vein occlusion or central retinal vein occlusion Annie Chan, Loh-Shan Leung, and Mark S Blumenkranz (Published online 2011 July 26), Dexamethasone intravitreal implant for the treatment of noninfectious uveitis Rebecca S Hunter and Ann-Marie Lobo (published online 2011 November 11), http://www.bauschvrx.com/, http://www.ema.europa.eu/docs/en_GB/document_library/Application_withdrawal_assessment_report/2010/01/WC500068245.pdf, Shalin, S et al. (2010). Drug delivery to the posterior segment of the eye for pharmacologic therapy. Expert Rev Ophthalmol.. 1 (5(1)), 75–93, Kompella, Uday B et al. (2010). Recent advances in ophthalmic drug delivery. Ther Deliv. 1 (3), 435-456, Short, Brian G. (2008). Safety Evaluation of Ocular Drug Delivery Formulations: Techniques and Practical Considerations. Toxicologic Pathology. 36 (49), 49-64.