491
advertisement
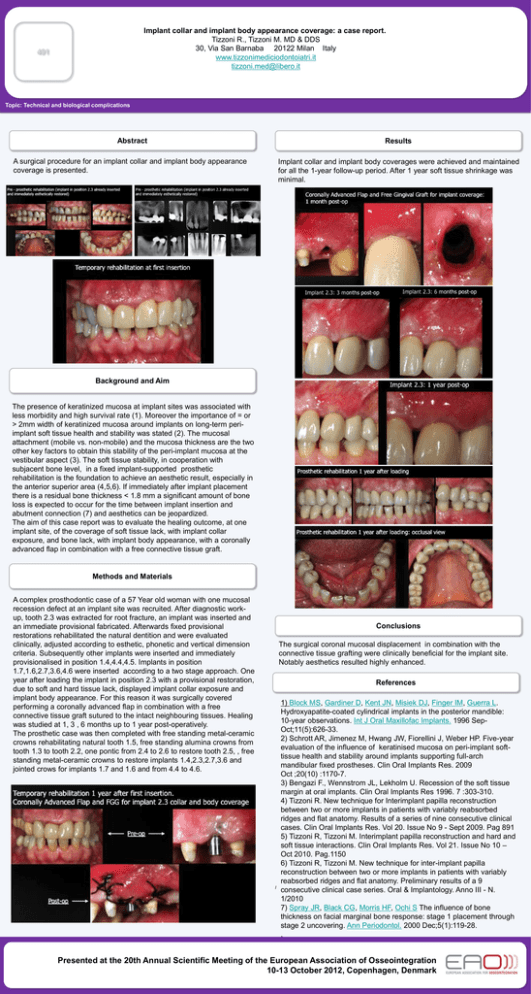
Implant collar and implant body appearance coverage: a case report. Tizzoni R., Tizzoni M. MD & DDS 30, Via San Barnaba 20122 Milan Italy www.tizzonimediciodontoiatri.it tizzoni.med@libero.it 491 Topic: Technical and biological complications Abstract Results A surgical procedure for an implant collar and implant body appearance coverage is presented. Implant collar and implant body coverages were achieved and maintained for all the 1-year follow-up period. After 1 year soft tissue shrinkage was minimal. Background and Aim The presence of keratinized mucosa at implant sites was associated with less morbidity and high survival rate (1). Moreover the importance of = or > 2mm width of keratinized mucosa around implants on long-term periimplant soft tissue health and stability was stated (2). The mucosal attachment (mobile vs. non-mobile) and the mucosa thickness are the two other key factors to obtain this stability of the peri-implant mucosa at the vestibular aspect (3). The soft tissue stability, in cooperation with subjacent bone level, in a fixed implant-supported prosthetic rehabilitation is the foundation to achieve an aesthetic result, especially in the anterior superior area (4,5,6). If immediately after implant placement there is a residual bone thickness < 1.8 mm a significant amount of bone loss is expected to occur for the time between implant insertion and abutment connection (7) and aesthetics can be jeopardized. The aim of this case report was to evaluate the healing outcome, at one implant site, of the coverage of soft tissue lack, with implant collar exposure, and bone lack, with implant body appearance, with a coronally advanced flap in combination with a free connective tissue graft. Methods and Materials A complex prosthodontic case of a 57 Year old woman with one mucosal recession defect at an implant site was recruited. After diagnostic workup, tooth 2.3 was extracted for root fracture, an implant was inserted and an immediate provisional fabricated. Afterwards fixed provisional restorations rehabilitated the natural dentition and were evaluated clinically, adjusted according to esthetic, phonetic and vertical dimension criteria. Subsequently other implants were inserted and immediately provisionalised in position 1.4,4.4,4.5. Implants in position 1.7,1.6,2.7,3.6,4.6 were inserted according to a two stage approach. One year after loading the implant in position 2.3 with a provisional restoration, due to soft and hard tissue lack, displayed implant collar exposure and implant body appearance. For this reason it was surgically covered performing a coronally advanced flap in combination with a free connective tissue graft sutured to the intact neighbouring tissues. Healing was studied at 1, 3 , 6 months up to 1 year post-operatively. The prosthetic case was then completed with free standing metal-ceramic crowns rehabilitating natural tooth 1.5, free standing alumina crowns from tooth 1.3 to tooth 2.2, one pontic from 2.4 to 2.6 to restore tooth 2.5, , free standing metal-ceramic crowns to restore implants 1.4,2.3,2.7,3.6 and jointed crows for implants 1.7 and 1.6 and from 4.4 to 4.6. Conclusions The surgical coronal mucosal displacement in combination with the connective tissue grafting were clinically beneficial for the implant site. Notably aesthetics resulted highly enhanced. References l 1) Block MS, Gardiner D, Kent JN, Misiek DJ, Finger IM, Guerra L. Hydroxyapatite-coated cylindrical implants in the posterior mandible: 10-year observations. Int J Oral Maxillofac Implants. 1996 SepOct;11(5):626-33. 2) Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinised mucosa on peri-implant softtissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009 Oct ;20(10) :1170-7. 3) Bengazi F., Wennstrom JL, Lekholm U. Recession of the soft tissue margin at oral implants. Clin Oral Implants Res 1996. 7 :303-310. 4) Tizzoni R. New technique for Interimplant papilla reconstruction between two or more implants in patients with variably reabsorbed ridges and flat anatomy. Results of a series of nine consecutive clinical cases. Clin Oral Implants Res. Vol 20. Issue No 9 - Sept 2009. Pag 891 5) Tizzoni R, Tizzoni M. Interimplant papilla reconstruction and hard and soft tissue interactions. Clin Oral Implants Res. Vol 21. Issue No 10 – Oct 2010. Pag.1150 6) Tizzoni R, Tizzoni M. New technique for inter-implant papilla reconstruction between two or more implants in patients with variably reabsorbed ridges and flat anatomy. Preliminary results of a 9 consecutive clinical case series. Oral & Implantology. Anno III - N. 1/2010 7) Spray JR, Black CG, Morris HF, Ochi S The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000 Dec;5(1):119-28. . Presented at the 20th Annual Scientific Meeting of the European Association of Osseointegration 10-13 October 2012, Copenhagen, Denmark