APIC Skin Prepping
advertisement
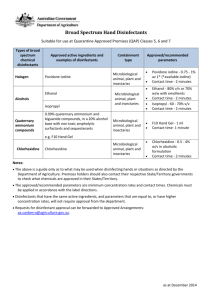
Skin Preparation: The Why, The Where, and The How Deb Danna RN BSN Clinical Consultant, CareFusion Overview • • • • • • Current Regulations and Guidelines Skin is the Source Skin Antiseptic Review Skin preparation Directions for Use Conclusion Return Demonstration and Competency Current Regulations and Guidelines • • • • • • FDA CDC AORN NQF Joint Commission CMS Joint Commission Best Practices Recommendations • • Hospitals Should Focus on Infection Management • Policies and Procedures must address regulatory requirements and evidence based standards • Involves education of health care workers • At hire and annually thereafter • At the time of change in job responsibility within the surgical environment Additional Hospital Responsibilities • Periodic Risk Assessments • Development of Metrics using Best Practices or Evidence-Based Guidelines • Compliance Monitoring and Evaluation 4 HAIs: A Costly Toll to U.S. Healthcare 1 1 1 1 1. Patient Protection and Affordable Care Act (PPACA) of 2010, S 301, 3008 and 3011;CMS IPPS FY11 Proposed Rule, April 19, 2010 5 HAIs: A Costly Toll to U.S. Healthcare 2 2. Scott RD. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. March 2009, Centers for Disease Control and Prevention. Accessed August 30, 2010 at: http://www.cdc.gov/ncidod/dhqp/pdf/Scott_CostPaper.pdf 6 Clinical and Economic Impact of HAIs • Attributable costs due to HAIs are substantial & carry significant morbidity and mortality Approximately 12% (159 patients) developed an HAI Avg. Length of Stay (LOS) was 5.9 to 9.6 days Excess LOS totaled 844 to 1,373 hospital days Attributable Costs $9,310 - $21,013 per patient $1.48 to $3.34 million in medical costs $5.27 million for premature death Costs attributable to healthcare-acquired infection in hospitalized adults and a comparison of economic methods. Med Care. 2010 Nov;48(11):1026-35. Roberts RR, et al. The National Spotlight-CMS Reimbursement CMS Reimbursement Final Rule •ALL hospitals participating in the US Medicare program must report data on specific HAIs through the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN). •Hospitals that do not submit data per the final rule are eligible to continue to participate in the Medicare program, but will be subject to a reduction in their Medicare Annual Payment Update. •As with other quality measures, any HAIs that may be added in the future will be publicly reported on the CMS Hospital Compare website Antiseptic Categories • Patient Preoperative Skin Preparation • Pre-injection vs. Pre-operative • Surgical Hand Scrub • Healthcare Personnel Hand wash How are you prepping the skin? • One Major risk factor for infections: • • • Heavy skin colonization of bacteria at incision site 80% of resident and transient skin flora resides in the first 5 layers of the stratum corneum. Does your application methodology assure that the solution reaches into the cracks and fissures of the stratum corneum layer? Disinfecting the Skin • The recommended antimicrobial agent should have the following properties: • Broad spectrum • Rapid bactericidal activity • Persistence or residual properties on the skin • Effective in the presence of blood • Non-irritating or have low allergic and/or toxic responses • No or minimal systemic absorption Antiseptic agent Mechanism of action Gram + bacteria Gram – bacteria Viruses Rapidity of action Persistent/ residual activity Use on eye or ear Use on mucous membranes Contraindications Cautions Alcohol Denatures proteins. Excellent Excellent Good Excellent None No. Can cause corneal damage or nerve damage. No Chlorhexidine gluconate Disrupts cell membrane. Excellent Good Good Moderate Excellent No. Can cause corneal damage. Can cause deafness if in contact with inner ear. Use with caution. Use with caution. Known hypersensitivity to drug or any ingredient. Lumbar puncture and use on meninges. Povidone-Iodine Oxidation/ substitution with free iodine. Excellent Good Good Moderate Minimal Yes. Moderate ocular irritant. Yes. Sensitivity to povidone-iodine (shellfish allergies are not a contraindication). Chlorhexidine gluconate with alcohol Disrupts cell membrane and denatures proteins. Excellent Excellent Good Excellent Excellent No. Can cause corneal damage. Can cause deafness if in contact with inner ear. No Known hypersensitivity to drug or any ingredient. Lumbar puncture and use on meninges. Flammable. Iodine-based with alcohol Oxidation/ substitution by free iodine denatures proteins. Excellent Excellent Good Excellent Moderate No. Can cause corneal damage or nerve damage. No. Sensitivity to povidone-iodine (shellfish allergies are not a contraindication). Flammable. Parachoroxylenol (PCMX) Disrupts cell membrane. Good Fair Fair Moderate Moderate Yes Yes Known hypersensitivity to PCMX or any ingredient. Minimally effective in the presence of organic matter. The FDA has classified PCMX as a Category III (data are insufficient to classify it as safe and effective). The FDA continues to evaluate PCMX. Flammable. Does not penetrate organic material. Optimum concentration is 60% to 90% Prolonged skin contact may cause irritation in sensitive individuals. Rare severe hypersensitivity reactions have been reported. Use with caution on mucous membranes. Prolonged skin contact may cause irritation. May cause iodism in susceptible individuals; avoid use in neonates. Inactivated by blood. Common Skin Preparations and Application Techniques Scrub and Paint 7.5% PVP Scrub and 10% PVP Paint Solution Preoperative Skin Prep: Application Techniques 7.5% Povidone Iodine Scrub and 10% Povidone Iodine Paint Solution • Scrub of the operative site should begin at the incision site, working out to the outer parameter in a concentric circular motion for 5 minutes. • Paint solution should be applied starting at the site of incision and working in a circular motion out to the perimeter of the area prepped. It should be allowed to dry for 2 to 3 minutes or until completely dry. Dry time of the paint application is a must for full efficacy of the product, due to the release of free available iodine necessary to kill bacteria on the skin. DuraPrep/Prevail-FX/Prevail • DuraPrep: 0.7%Povidone Iodine /74% Isopropyl alcohol, povacrylex (6 ml & 26 ml) PREVAIL-FX: 0.83%Povidone Iodine /72.5% Isopropyl alcohol, polymer (40 ml) PREVAIL: 0.5% Povidone Iodine/ 62% ethanol alcohol (59 ml & 40 ml) Preoperative Skin Prep: Application Techniques • To activate the applicator: twist the applicator head and push down. Lightly squeeze the bottle to initiate the flow of the prep solution. Application: Apply for thin even coat starting at the incision site and working outward in a circular motion. The flow of the solution is controlled by squeezing the applicator body. The solution should not be blotted, but simply allowed to dry. Dry time for larger volume alcohol based skin antiseptics is a minimum 3 minutes in non-hairy areas and up to 1 hour in hairy areas Chlorhexidine Gluconate 2%-4% formulations Hibiclens/BetaSept/ Exidine Preoperative Skin Prep: Application Techniques 2% - 4% Chlorhexidine Gluconate • Chlorhexidine Gluconate skin prep agents should be applied liberally to the surgical site and swabbed for at least 2 minutes, starting from the incision site out to the periphery. The prepped area should be blotted dry with a sterile towel; this procedure is then repeated for an additional 2 minutes and dried with a sterile towel. • Total prep time is 4 minutes. ChloraPrep 2% Chlorhexidine gluconate 70% Isopropyl Alcohol Preoperative Skin Prep: Application Techniques 2% CHG / 70% Isopropyl Alcohol • For dry surgical sites (e.g., the abdomen or arm): Repeated back-and-forth strokes of the sponge should be used for approximately 30 seconds on the incision site and outward to the periphery. • For moist surgical sites (e.g., inguinal fold or axilla): Repeated back-and-forth strokes of the sponge should be used for approximately 2 minutes on the incision site and outward to the periphery. As noted above, using a back and forth scrub applies the antiseptics with sufficient friction to encourage exfoliation and/or deeper penetration of the superficial layers, as well as the cracks and fissures of the skin. Total prep time is 30 seconds / 2 minutes followed by a 3 minute dry time in non-hairy areas and up to 1 hour for hairy areas Preoperative Skin Prep: Application Techniques 2% CHG/70% Isopropyl Alcohol • Latex free • External use only • No contact to patient’s eyes, ears, or mouth, lumbar puncture, intravaginal, etc. • Do not use on children under 2 months • Avoid freezing and excessive heat • Allow to dry No pooling of solution 26 ml Not recommended for head and neck surgery Remove wet materials before starting procedure Preoperative Skin Prep: Application Techniques 2% CHG / 70% Isopropyl Alcohol • Allow to dry completely • Do not let solution pool • Do not use 26ml applicator for head and neck • Do not use on small areas • Remove any wet materials prior to using ignition source Fire Safety • Flammable prep agent = ALCOHOL • Do not allow prep agent to pool on or under body parts • Allow prep agent to dry • Allow vapors to dissipate before applying drape Fire Safety • Alert all personnel about the use of a flammable preparation agent through active communication and during the “time out” period • Do not heat flammable skin preparation agents Issues Related to Shaving • Shaving attributed to microscopic cuts in the skin • Cuts are foci for bacterial multiplication1 • If shaving performed >24 hours prior to operation, infection rate exceeds 20%2 1. Martorell C, Engelman R, Corl A, Brown RB. Surgical site infections in cardiac surgery: an 11-year perspective. AM J Infect Control. 2004;32(2):63-68. 2. Institute of Healthcare Improvement. Surgical Site Infections. Available at: http://www.ihi.org/IHI/Topics/PatientSafety/SurgicalSiteInfections. Accessed December, 2007. 1. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999; 20: 250-278; quiz 279-280. 2. Seropian R, Reynolds BM. Wound infections after preoperative depilatory versus razor preparation. Am J Surg 1971;121:251-4. Micro Abrasions Before Clipping Before Shaving After Clipping After Shaving Recommended Practices for Clipping Leading healthcare industry organizations recommend that, when preoperative hair removal is necessary, it should be done with clippers instead of razors. • Centers for Disease Control and Prevention (CDC) • Association of Perioperative Registered Nurses (AORN) • The Institute for Healthcare Improvement (IHI) • The Surgical Care Improvement Project (SCIP) • The 2008 ISDA Compendium • Greater Healthcare now-Canadian SSI guidelines Recommendations: AORN • If hair interferes with the surgical procedure, ideally remove it: • the day of surgery • outside the operating or procedure room • From only those areas where it interferes with the surgical procedure • using a single-use electric or battery-operated clipper, or a clipper with reusable head that can be disinfected between patients • Always follow Manufacturers’ Directions for Use (DFUs) In Conclusion • KEY to effective preoperative patient skin antisepsis Antiseptic agents supported by clinical evidence Proper application technique Questions?