Bound by Silicone - roeloffze dental laboratory
advertisement

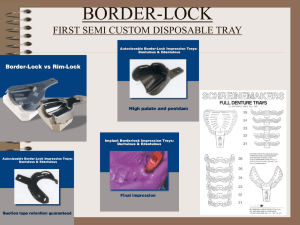
The sticky relationship between Dentists and Dental Laboratories Mark Jackson, RDT Precision Ceramics Dental Laboratory, DAMAS Montclair, CA The Dentist and the Dental Lab According to the FDA, the Dental Laboratory is a Medical Device Manufacturer and subject to FDA Good manufacturing Practices….. But things haven’t always been like this! During the middle ages and throughout the 19th century, dentistry was not a profession in itself, and often dental procedures were performed by barbers or general physicians. Barbers usually limited their practice to extracting teeth which alleviated pain and associated chronic tooth infection. At the turn of the century, most dentists were expected to make their own dentures crowns and bridges, but by the 1900’s the dentists realized the economic benefits of finding specialized help. Professional relations were best summarized in two simple words: “Yes Doctor.” The “Plaster Monkey” was actually a term of endearment, and the “dental mechanic” became an important member of the dental team, though dentists still kept them closely supervised….and undereducated. Dental Technicians were forbidden to attend lectures and meetings, and in 1963, the NADL and ADA broke off relations. It was a contentious time. Today’s credentialed technicians have strong backgrounds in material science, dental anatomy and CAD/CAM technology, and in some cases can earn more than a general dentist. Despite some professional growing pains, and some sibling rivalry, we share a relationship that is mutually beneficial, financially rewarding and based on a shared respect. HOWEVER…. Our Relationship is held together by a third party The dental impression is the key ingredient in our relationship, and can often make or break it. We depend on the quality, consistency and the technical support provided by our impression material manufacturers. Impressions are the foundation of everything we do. It all starts with a great impression.... But usually not….. More than 50% of the impressions we receive are substandard, yet only 1-2% will be returned Proper tray selection Proper use of tray adhesive Material properly mixed Adequate volume of material Adequate adhesion between materials No pressure points or tray pinching No teeth contacting the tray Good detail of margin (finish line) Good detail of prepared teeth No voids or pulls in the material that will cause interference While this impression displays a number of problems, it was clearly the improper tray for this application. Improper tray selection can cause tray flex and rebound. This tray had no adhesive at all, and also shows signs of possible tray distortion. Tray adhesives are specifically formulated and not interchangeable. With modern impression delivery systems, mixing problems have been all but eliminated, however glove contamination and chemicals can inhibit polymerization and setting resulting in tacky washed out appearance. Improperly filled impression trays can result in missed anatomical features or movement of the material within the tray borders Inadequate adhesion between different impression materials can be caused by contamination, exceeding the working time or improper storage of material. This tray was either not positioned properly, or was the wrong size. When this happens, the tray can flex and spring back, distorting the impression, or in the best case hold the bite open. Like the previous example of a pressure point, this tray was either the wrong size, or improperly positioned, but instead of a soft tissue compression, we have tooth-on-tray contact. Poor gingival retraction and syringing technique. Not bleeding the mixing tip or poor syringing technique has resulted in air folding or entrapment Insufficient retraction or tearing Improper retraction, possible fluid or chemical contamination Improper retraction allowing blood or saliva to pool around the prepared tooth. Exceeding working time. This impression has voids and pulls caused by exceeding working time, moving the tray after seating, or not enough material. These defects can interfere with occlusion and mounting models Evaluating remakes Every impression would be a perfect one, that had been inspected by the dentist, and was free of the defects we just discussed, but that is rarely the case…. Most dental laboratories have a profit margin of 10% or less. That means they may have to do as many as 19 units at no profit to pay for a single remake. Every remake is evaluated to determine the nature of the failure. In some cases it is laboratory error or product failure, and sometimes it is doctor error. The easiest way to see if the impression was the problem is to simply insert the new die into the old impression and look for the discrepancy. A common problem is misreading the margin, usually caused by a bad impression, though technician error does happen too. Frankly, the lab takes some blame due to errors in mixing stone, applying surfactant or surface disinfectants, though we try to automate these processes when possible. But in an overwhelming number of cases the problem can be traced back to a bad impression. In some cases we accepted them when we really should have sent them back. And it’s even less likely there will be time to do it over! This is where many of us revert back to our primordial roots, avoid confrontation and “do our best” at the doctors instruction We take the “passive aggressive” approach… The “habitual offender” card Carefully inspect your impression before releasing your patient. Any pull, voids, bubbles, unset or sticky material indicates contamination or a mixing problem. This will lead to a remake. If you use a desensitizing substance on prepared teeth, apply it AFTER taking your impression. These substances effect impression materials and if used improperly will guarantee a remake. Retraction cord containing epinephrine, or other material containing epinephrine will cause deterioration, sticky or unset margins in some impression materials. AGGRESSIVELY rinse and clean the prepared teeth before injecting your wash material. Materials containing Ferrite sulfate will cause some impression materials to not set properly, especially in thin areas such as margins. Save yourself a remake; clean and rinse your preps well before taking the impression If you are using “sideless” triple trays, PLEASE check to see that the patient did not bite into, or onto the tray. If they did, when we mount the models, the bite will be off, and you will lose precious time adjusting the occlusion and possibly ruining the crown, or sending it back for repairs. A preliminary check could save hundreds of dollars later. PLEASE take some time to make sure your temporaries are in occlusion, and that contacts are tight. For long span bridges, or cosmetic make-overs, consider our lab processed temporaries. Believe it or not, we have seen three and four unit bridge cases with single crown temporaries on the abutments. That’s a great way to guarantee your bridge will NOT fit! We recommend a two cord technique. A combination of #00 and #2 cords will provide adequate retraction for nice clear exposure of your margins. For anterior cases, please send an impression of the temporaries, or a diagnostic wax up, so that we can try and match patient expectations. Photos, shade maps and other tools will ensure a happy patient and a happy doctor. When injecting wash impression around the margins, use a stirring motion and “jiggle” the material constantly to avoid air bubbles or voids. Never stop and restart an impression. If you don’t think the cartridge has enough material left to completely encircle the prep, use a new cartridge. If the case has loose tissue, of if the prep is very subgingival, use the cartridge tip to push the tissue away as you inject the material to prevent it from laying over onto the margin. DO NOT use the “touch” technique to determine if your impression is set; use an inexpensive egg timer or other timing device. The manufacturer has done extensive tests to determine the best setting time and conditions. The material you are touching has been exposed to air, and may set before the was material has, and it is important to have this part intact and accurate. Don’t touch; thime it or you may end up remaking it. All crown preps should have adequate prep reductions of at least 1.5 mm for both PFM and All Ceramic Crowns. Note: 7 out of 10 tips are impression related! Kerr Rep We call in reinforcements!