Effective and Supportive Transitions of Care
advertisement
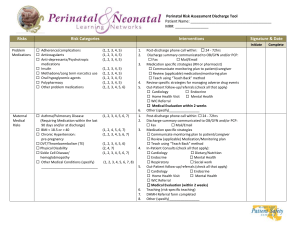
Effective and Supportive Transitions of Care: The Care Teams Role in Reducing Admissions Jim Kinsey, Planetree Presented to Texas Center for Quality and Safety January 2013 Setting the Stage The term "transitions of care" refers to a patient leaving one care setting and moving to another as their condition or healthcare needs change. The care transition often involves multiple persons including the patient, family or other caregivers... An optimal transition should be well planned with the involvement of the patient and family, and adequately timed. More often, however, the communication between settings and the coordination among caregivers, patients and healthcare professionals fail to provide all the information needed for optimum quality of care Just the Facts Just the Facts Cost $25 billion dollars annually Most patients are on 6+ medications at time of discharge Limited access to post-hospitalization follow-up care Preventable transition errors (mostly medication related) Penalties: $280,000,000 in 2012 Including over 2, 000 hospitals 1,910 of those hospitals receiving less than 1% penalty Penalties increase to 2% in 2013 and 3% 2014 NQF 2010-2012 It is not just about reimbursement… So where do we begin… Communication Collaboration Communicate: Patient and Family Activation • Care Partner Programs • Clear concise advance directives • Diagnosing patient preferences Preference Diagnosis: First Step to Effective Transitions TEAM TALK • Inform the patient that choice exists. • Differentiate between the doctor’s medical expertise and the patient’s expertise on what matters most to him/her. • Invite the patient to form a team to explore options. OPTION TALK • List options and risks, benefits and side effects. • Engage patient in deliberations. • Observe patient’s reactions. • Follow patient’s lead as guide for continuing option talk or moving to decision talk. DECISION TALK • Ask: Do you feel ready to make a decision or receive a recommendation? • Assess whether patient’s decision is consistent with stated priorities. If yes, offer support; if no, propose additional option talk • If asked to make a recommendation, doctor should confirm understanding of patient’s priorities Drawn from Mulley, A.G., Trimble, C. and Elwyn, G. “Stop the silent misdiagnosis: patients’ preferences matter.” BMJ, 2012, 345. Collaborating for Positive Patient Outcomes Medication Reconciliation Discharge Instructions Consistent Care Philosophy Coordinated Discharge Plan Patient Care Narrative or Personal EMR Physician Follow-Up Scheduled for 24 hours or less Social Support Evaluation Verbal Report Shared Electronic Record Care Team Activities Acute Care Preference Diagnosis/Social Support Care Partner Program Discharge Planning Comprehensive Medication Review Personal MR Narrative Verbal report to next provider Skilled Care Standing orders collaboration Doctor Visit within 24 hours Evaluate Social Support Medication Availability Consistent treatment plan Prepare for discharge Home Care Receive verbal report, preferably in person with patient Equipment delivered in advance Medication reconciliation Creating a Collaborative Patients Voice • Tell me about your recent transition of care? • Tell me how we may have done that better? Provider Voice: Who are the players in your community? • • • • What is working? What isn't working? How to we create standard work and processes between our service lines? How can we standardize treatment philosophies while maintain focus on patient preferences? Most importantly put down the history and focus on providing exceptional patient experiences “…the thought is that we are here to provide service to patients and their families, understanding that patients are not isolated individual units, but they function as part of a social system, so involving family also in access to information, education and care is very important.” Susan Frampton, President Planetree Jim Kinsey, Planetree 610.733.5140 jkinsey@planetree.org www.planetree.org