Part I
Investigator Insights
Emerging Multikinase Inhibitors
in Thyroid Carcinoma
Dr. Marcia Brose
Abramson Cancer Center
University of Pennsylvania
MSB
09/21/09
Thyroid Cancer: Clinical
Pathology
Papillary
Follicular cells
Differentiated
Follicular
Hurtle Cell
Anaplastic
Parafollicular cells
Medullary
Sporadic
Familial
American Cancer Society. www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_is_thyroid_cancer_43.asp. Carling T and
Uldesman R. Cancer of the Endocrine System.: Section 2: Thyroid Cancer. Principles of Clinical Oncology. 7th edition. Lippincott
Williams and Wilkins. 2005.
MSB
05/30/09
Global Incidence of Thyroid Cancer
was > 212,000 in 20081
Estimated Thyroid Cancer Incidence in 2008
Annual Incidence
40000
35000
~37,000
~33,000
30000
• DTC represents
> 90% of all thyroid
carcinomas2
25000
20000
~18,000
15000
10000
~6,000
5000
0
US
EU
• Thyroid cancer is
the most common
form of endocrine
malignancy1
LA/C
Japan
• The prognosis of
patients with DTC
is generally good
due to tumor
biology and efficacy
of the initial surgery
and 131I therapy3
LA/C = Latin America and Caribbean.
1. GLOBOCAN 2008, International Agency for Research on Cancer. http://globocan.iarc.fr/.
2. Sherman. Lancet. 2003;361:501-511.
3. Eustatia-Rutten et al. J Clin Endocrinol Metab. 2006;91:313-319.
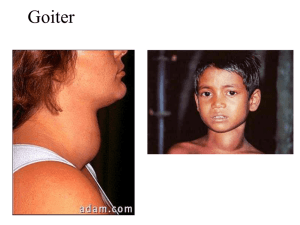
Dimensions of the problem
• Increasing in incidence
– 95% sporadic or RT-induced, 5% familial
• 3.5 to 4:1 female to male gender distribution
• > 95% of carcinomas arise from thyroid follicular
cells and are well-differentiated
• Surgery +/- I-131 remains the standard of care
– Vast majority treated in this manner are cured
• Emergence of Multiple TKIs in Iodine-Refractory
TC and MTC that can affect response and likely
prolong PFS and OS
Thyroid Cancer in the United States
New Diagnosis
Pfister, D. Treatment of Radioactive Thyroid Cancer. Presentation. ASCO, 2007.
Cancer Deaths
Thyroid cancer in the United States
0-1.0cm
1.1-2.0cm
2.1-5.0cm
Davies, JAMA 2006
295:2164
>5.0cm
DTC: Initial Disease Stage Predicts
OVERALL SURVIVAL
Stage I
100%
75%
Stage II
of all
tumors
80%
Survival
60%
Stage III
25%
40%
of all
tumors
20%
Stage IV
0%
p<0.001
0
2
4
Jonklaas J et al. Thyroid. 2006, 16(12): 1229-1242.
6
Years
8
10
12
14
MSB
05/30/09
Thyroid Cancer: Treatment Strategy
• High Risk: (Age >45, male, metastasis,
extrathyroidal extension, >4cm)
– Total Thyroidectomy
– RAI (131I) Ablation
– TSH Suppression Therapy with Thyroid
Hormone
– Follow Serial Thyroglobulin Levels (Tg)
– XRT for recurrent local disease/positive margins
– Surveillance: NeckUS, Tg, Neck MRI, Chest CT,
RAI Whole body scan, FDG-PET
MSB
05/30/09
TSH Suppression Improves Survival for
DTC Patients With Metastases
100
Survival, %
80
60
n = 450
40
Median
TSH suppressed
TSH unsuppressed
20
All
> 45 yr
15 yr
11 yr
10 yr
6 yr
p < 0.01
p < 0.005
0
0
2
4
Jonklaas et al. Thyroid. 2006;16:1299-1242.
6
8
10
Years
12
14
16
18
Survival and Response to
Treatment
1.0
1
0.9
0.8
127 patients
4 cancer related
deaths
Survival (%)
0.7
0.6
0.5
168 patients
0.4
0.3
2
• Group 1: initial 131I uptake
and CR
– Age < 40 years
– Well-differentiated cancer
– Small size of metastases
• Group 2: initial 131I uptake
and persistent disease
• Group 3: no initial 131I uptake
0.2
0.1
3
149 patients
0.0
0
5 10 15 20 25 30 35 40
Years after the discovery of metastases
Durante et al. J Clin Endocrinol Metab. 2006;91:2892-2899.
RAI-refractory disease
• 25–50% of metastatic thyroid cancers lose
ability to take up iodine
• RAI refractory means that there are
progressing lesions that do not take up
RAI (Note: there may still be some that do)
• Loss of iodine uptake inversely correlates
with survival
Cooper DS, et al. Thyroid. 2009;9:1176-214.
Hodak SP, Carty SE. Oncology. 2009;23:775-6.
Mehra R, Cohen RB. Hematol Oncol Clin North Am. 2008;22:1279-95,xi.
RAI-Refractory Thyroid Cancer
• L-T4 treatment: serum
TSH < 0.1 mU/L
• Local treatments when
needed: surgery, radiation,
radiofrequency or cryoablation
• Imaging follow-up every
6 months
• Stable disease: follow-up
Cooper et al. Thyroid. 2009;9:1167-1214.
• Progression:
– > 20% (RECIST) in
6-15 months
– Inclusion in a trial
• Chemotherapy: low
efficacy, significant
toxicity (eg, doxorubicin:
5% PR, 47% SD,
median PFS 7 months)
• Targeted therapy as
first line (ATA, 2009)
NCCN and ATA guidelines for the treatment of
differentiated thyroid cancer (DTC)
Initial treatment
• Total thyroidectomy, except in patients with unifocal microcarcinoma
(individualized to patient and extent of disease)1,2
Postoperative treatment
• Radioactive iodine (131I) (RAI) therapy1,2
Follow-up treatment
• Levothyroxine to suppress TSH levels to < 0.1mU/L1,2
Recurrent or metastatic disease treatment
• Local therapy (re-operation, external radiation)
• Systemic therapy
– RAI therapy
– patients with refractory advanced disease
• chemotherapy (limited efficacy and considerable toxicity)1,2
• participation in clinical trials with small molecule tyrosine kinase
inhibitors is recommended1,2
NCCN = National Comprehensive Cancer Network.
ATA = American Thyroid Association .
1. NCCN Clinical Practice Guidelines in Oncology. Thyroid Carcinoma V.1.2010.
2. Cooper DS, et al. Thyroid .2009;9:1167-214.
Thyroid Cancer is associated with
aberrant cell signaling
MAP Kinase
Genetic Alteration
PTC
FTC
BRAF V600E
44%
0%
BRAF copy gain
3%
35%
RET/PTC (1 and 3)
20%
0%
8-10%
17-45%
PI3KCA mutations
3%
6%
PI3KCA copy gain
12%
28%
PTEN
2%
7%
Pax8/PPARγ
0%
35%
>70%
>65%
PI3K/AKT
RAS
Total
Nikiforov, Mod Path, 2008, Xing Endocrine Rel Ca(2005), Wang et al, 2007
RAS/BRAF Mutations are More Prevalent
in RAI Refractory Thyroid Cancer
Ricarte-Filho JC, Cancer Research 2009 Jun 1;69(11):4885-93
MSB
09/21/09
Cell signalling in differentiated
thyroid cancer
Tumor Cell
RET/PTC
Endothelial Cell
EGFR
VEGFR-2
Ras
B-Raf
MEK
ERK
Ras
PI3K
Raf
PI3K
MEK
AKT
ERK
mTOR
AKT
mTOR
S6K
• Growth
• HIF1a
• Survival
• Inhibition of apoptosis
• Proliferation • Migration
S6K
• Growth
• Survival
• Proliferation
• Migration
• Angiogenesis
Graphic adapted from
Keefe SM, et al. Clin Cancer Res. 2010;16:778-83.
Who is appropriate for kinase inhibitor
therapy?
1. Patients whose tumors no longer take up
radioactive iodine or who have exceeded
their lifetime dose
2. Patients with disease measurable by
exam or CT scan
3. Patients with >1 lesion which is >1 cm in
size and who are symptomatic
4. Patients with progressive disease
MSB
09/21/09
Part II
Investigator Insights
Emerging Multikinase Inhibitors
in Thyroid Carcinoma
Dr. Marcia Brose
Abramson Cancer Center
University of Pennsylvania
MSB
09/21/09
Kinase Inhibitors
ATP
KI
ATP
Y
P
KI
Y
Activated pathway
Activated Pathway
Cancer
Cancer
RET, BRAF…..
inhibition
VEGFR inhibition
Tumor
Tumor
growth
angiogenesis
Targeting cell signalling in thyroid cancer
Tumor Cell
RET/PTC
Motesanib
Sorafenib
Sunitinib
Vandetanib
XL-184
Endothelial Cell
EGFR
VEGFR-2
Vandetanib
Ras
B-Raf
Sorafenib
MEK
ERK
Ras
PI3K
AKT
mTOR
S6K
Sorafenib
Everolimus
Sirolimus
• Growth
• HIF1a
• Survival
• Inhibition of apoptosis
• Proliferation • Migration
Raf
PI3K
MEK
AKT
ERK
mTOR
Axitinib
Motesanib
Sorafenib
Sunitinib
Vandetanib
Everolimus
Sirolimus
S6K
• Growth
• Survival
• Proliferation
• Migration
• Angiogenesis
Graphic adapted from
Keefe SM, et al. Clin Cancer Res. 2010;16:778-83.
Thyroid Cancer is associated with
aberrant cell signaling
MAP Kinase
Genetic Alteration
PTC
FTC
BRAF V600E
44%
0%
BRAF copy gain
3%
35%
RET/PTC (1 and 3)
20%
0%
8-10%
17-45%
PI3KCA mutations
3%
6%
PI3KCA copy gain
12%
28%
PTEN
2%
7%
Pax8/PPARγ
0%
35%
>70%
>65%
PI3K/AKT
RAS
Total
Nikiforov, Mod Path, 2008, Xing Endocrine Rel Ca(2005), Wang et al, 2007
UPCC 03305: Sorafenib in
Advanced Thyroid Cancer
Eligibility criteria
• Metastatic, iodine
refractory thyroid cancer
• Life expectancy >3
months
Primary endpoints
n=55
• Evidence of PD within 6
months of study entry
Sorafenib
400mg b.i.d.
• RECIST
• PFS
• Response rate
• ECOG 0–2
• Good organ and bone
marrow function
b.i.d. = twice daily; RECIST = Response Evaluation Criteria In
Solid Tumors; ULN = upper limit of normal
Gupta-Abramson V, et al. J Clin Oncol 2008;26:4714–9
Update UPCC O3305: May 2009
Results:
• Response for all 50 evaluable patients
– PR 36% (18 patients)
– SD 46% (23 patients)
– clinical benefit 82% (41 patients)
• Exact binomial confidence interval excludes the null
hypothesis (p<0.0001)
• PFS is 63 weeks for all patients, and 84 weeks in patients
with DTC
Brose M, et al. J Clin Oncol 2009;27(May 20 Suppl.):301s (Abstract 6002)
UPCC 03305: Best Response in
46 Evaluable Patients
Change in sum of target lesion by RECIST
compared to baseline (%)
Best response of advanced thyroid cancer patients to sorafenib
PD
30
20
10
0
–10
–20
–30
–40
–50
–60
–70
–80
–90
–10
SD
PR
Papillary
Follicular/Hürthle Cell
Medullary
Poorly Differentiated/Anaplastic
Brose M, et al. J Clin Oncol 2009;27(May 20 Suppl.):301s (Abstract 6002)
Cutaneous Adverse Events with Sorafenib in
Thyroid Carcinoma Patients
1. Cutaneous toxicity peaks in the second
cycle
2. Brief dose holidays and dose reductions
are reasonable. Rash usually improves
with continued sorafenib treatment
3. Rash is more common in patients with
extensive sun exposure in the past
4. Skin creams may be used as well as
NSAIDs for control of the pain from the
MSB
rash
09/21/09
Phase III Study of Sorafenib in Locally Advanced or
Metastatic Patients with Radioactive Iodine Refractory Thyroid
Cancer (DECISION) trial – Primary Endpoint POSITIVE
Eligibility criteria
• Locally advanced
or metastatic DTC
• Progression
within 14 months
• RAI refractory
• No prior targeted
therapy,
chemotherapy or
thalidomide
Primary Endpoint:
PFS (RECIST)
Independent review
Randomisation (1:1)
(n=380)
• An International, multicentre, randomised, double-blind, phase III study
of sorafenib versus placebo in locally advanced/metastatic RAIrefractory DTC
Sorafenib
400mg orally
b.i.d.
n=190
Placebo
n=190
Secondary Endpoints:
OS, TTP, RR, DCR, PRO, PK
Safety
Exploratory Biomarkers
Progression
Investigator’s decision
Crossover or
continue
sorafenib 400mg
orally b.i.d.
Off
study
Disease
progression
www.clinicaltrials.gov. NCT00984282
Phase III DECISION Trial
• Over 400 patients enrolled in the trial
world wide
• January 3, 2013 press release revealed
that the primary endpoint of Progression
Free Survival significantly favored the
Sorafenib arm
• The final results of the study to be
presented at a major meeting in 2013
MSB
09/21/09
Therapeutic Options beyond frontline TKI
therapy
1. Single progressive lesions can be resected or
irradiated and the frontline TKI continued
2. Minimally progressive lesions can often be
observed on the original TKI as this disease
frequently progresses very slowly
3. For patients progressing on a frontline TKI, an
m-TOR inhibitor can be added to block the
PI3K escape pathway
4. For disease progressing in multiple areas one
might switch to another available TKI or a
clinical trial with an investigational agent
MSB
09/21/09
Part III
MSB
09/21/09
Investigator Insights
Emerging Multikinase Inhibitors
in Thyroid Carcinoma
Dr. Marcia Brose
Abramson Cancer Center
University of Pennsylvania
MSB
09/21/09
Advanced Thyroid Cancer’s New Unmet Need:
Progression on Sorafenib/VEGFR2 inhibitor
• What to do with patients who progress but
maintain good performance status
• Most patients respond to frontline TKI
therapy but then progress in a new lesion
or a subset of lesions
Targets of Kinase Inhibitors
Compound Name
VEGFR
BRAF
PDGFR
KIT
RET
Other
Sorafenib
(Nexavar)
+
+
+
+
+
FLT-3
Sunitinib (Sutent)
+
+
+
Axitinib
(AG-013736)
+
+
+
Motesanib (AMG706)
+
+
+
Pazopanib
(GW786034)
+
+
+
Vandetanib
(Zactima)
+
+
EGFR
Cabozotanib
(XL184)
+
+
C-MET
Lenvatinib
(E7080)
+
+
FGFR
+
+
FLT-3
+
Targeted Agents: Phase II Clinical Data
Drug
Key Baseline
Characteristics
n
Sorafenib
(Brose)
•DTC+ PDTC(90%),
47
Sunitinib
(Cohen)
• DTC (74%); MTC
(26%)
Axitinib
(Cohen)
PFS
PR
SD
PD
20
38%
47%
2%
51
-
17%
DTC
74%
DTC
9% DTC
•Papillary (50%);
Medullary (18%);
Follicular/Hurthle
(25%/18%); Anaplastic
(3%)
60
18.1
30%
48%
7%
Motesanib
(Sherman)
•Papillary (61%);
Follicular/Hurthle (34%)
93
10
14%
67%
8%
Pazopanib
(Bible)
PD and DTC
(Progression <6months)
37
12
49%
-
-
Lenvatinib
(E7080,
Sherman)
•DTC 100%
58
13.3
45%
46%
5%
Months
MSB
05/30/09
Targeting cell signalling in thyroid cancer
Tumor Cell
RET/PTC
Motesanib
Sorafenib
Sunitinib
Vandetanib
XL-184
Endothelial Cell
EGFR
VEGFR-2
Vandetanib
Ras
B-Raf
Sorafenib
MEK
ERK
Ras
PI3K
AKT
mTOR
S6K
Sorafenib
Everolimus
Sirolimus
• Growth
• HIF1a
• Survival
• Inhibition of apoptosis
• Proliferation • Migration
Raf
PI3K
MEK
AKT
ERK
mTOR
Axitinib
Motesanib
Sorafenib
Sunitinib
Vandetanib
Everolimus
Sirolimus
S6K
• Growth
• Survival
• Proliferation
• Migration
• Angiogenesis
Graphic adapted from
Keefe SM, et al. Clin Cancer Res. 2010;16:778-83.
UPCC 19309: Everolimus + Sorafenib
for DTC patients who progress on
Sorafenib alone
Eligibility criteria
• Metastatic, iodine
refractory thyroid cancer
• Life expectancy >3
months
n=35
• PD on sorafenib
Sorafenib
+ Everolimus
Intra-patient
Dose escalation.
Primary endpoints
• RECIST
• PFS
• Response rate
• ECOG 0–2
• Good organ and bone
marrow function
b.i.d. = twice daily; RECIST = Response Evaluation Criteria In
Solid Tumors; ULN = upper limit of normal
22 patients accrued so far
Primary Endpoint:
Best Overall response Rate (BORR)
(RECIST 1.1) (Partial and complete
RR) in sorafenib naïve pts
Independent review
BRAF V600E testing
Eligibility criteria:
• Locally advanced
or metastatic DTC
• Progression
within 14 months
• RAI refractory
Informed Consent
UPCC 18310: NO25530: An Open-Label, Multi-Center
Phase II Study of the BRAF Inhibitor Vemurafenib in
Patients with Metastatic or Unresectable Papillary Thyroid
Cancer (PTC) positive for the BRAF V600 Mutation and
Resistant to Radioactive Iodine
+
+
First Line
Sorafenib Naïve
(n=25)
Second Line
Prior Sorafenib
(n=25)
Secondary Endpoints:
•PFS, TTP, OS, TTP, in
sorafenib naïve pts
•BORR, CB, TTP, PFS and
OS, in soraefnib exposed
patients
Vemurafenib
960mg BID
Clinical Trials Ongoing for Metastatic Differentiated
Thyroid Cancer
Compound Name
DTC/MTC
Status
Sorafenib (Nexavar)
DTC
First Line – International Phase III –
Positive Study, Awaiting Data Presentation
Lenvatinib (E7080)
DTC
First and Second Line – Phase III
Vemurafenib
(BRAF V600E inhibitor)
DTC (PTC)
First and Second Line Phase II – (Phase III?)
Everolimus+Sorafenib
DTC
Second Line – Phase II
Cabozantinib
DTC
First Line – Phase I complete
First Line and Second Line Phase II– Pending
Pioglitazone (PPARγ)
DTC (FTC*)
First and Second Line - Phase II
Pazopanib (GW786034)
DTC
First and Second line – Phase II Done
Sunitinib (Sutent)
DTC
First line Phase II – Done.
MSB
10/16/10
Take Home Messages-I
• Multiple VEGFR agents in DTC have activity that affect the vast
majority of patients with advanced RAI-refractory thyroid cancer
needing therapy
• Results of phase III trial with sorafenib (DECISION) showing that
patients treated with sorafenib have a longer progression free
survival than those on placebo. We look forward to a future major
oncology meeting for these results. Results from the Phase III trial of
lenvatinib (SELECT ) are likely to follow in another year.
• Molecular markers (eg. BRAF V600E mutation) are newer targets
being tested in Phase II clinical trials. If positive, patients will need
routine molecular testing for these mutations
• Many studies for second line treatment of DTC are underway and
now a primary focus of our research program at the Abramson
Cancer Center and at other sites. These trials target new molecular
mechanisms and hope to add to the success of the VEGFR inhibitors
in this disease.
Take Home Messages-II
1. Patients with progressive RAI-refractory TC should be
referred to an oncologist with access to all the available
and investigational kinase inhibitors.
2. Treatment with a kinase inhibitor should be initiated in
patients with progressive, measurable disease.
3. The physician managing these patients should be
comfortable with and skilled in managing the adverse
events related to kinase inhibitors.
4. Many clinical trials are now available for patients
progressing on frontline kinase inhibitor therapy.
MSB
09/21/09
References
1. Giuffrida D, Prestifilippo A, et al; Journal of Oncology Volume 2012,
Article ID-391629, “New Treatment in Advanced Thyroid Cancer”
2. Brose M, Nutting C, et al; BMC Cancer 2011, 11:349 “Rationale
and design of DECISION: a double blind, randomized, placebo
controlled phase III trial evaluating the efficacy and safety of
sorafenib in patients with locally advanced or metastatic, RAIrefractory, differentiated thyroid cancer”
3. Harris P, Bible K; Expert Opinion Investigational Drugs; October
2011 20(10): 1357-1375; “Emerging Therapeutics for Advanced
Thyroid Malignancies: Rationale and Targeted Approaches”
4. Gupta-Abramson V, Troxel A, et al; JCO 2008 Vol. 26: 4714
“Phase II Trial of Sorafenib in Advanced Thyroid Cancer”
5. Kojic K, Kojic S & Wiseman S; Expert Reviews in Anticancer
Therapy 2012 Vol.12(3):345; “Differentiated thyroid cancers: a
comprehensive review of novel targeted therapies
MSB
09/21/09