Randomized Phase III Trial of Regorafenib in Patients (pts)
advertisement

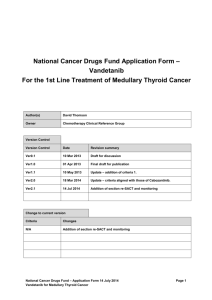
Management Advances for Differentiated and Medullary Thyroid Carcinoma Marcia S. Brose MD PhD Abramson Cancer Center of the University of Pennsylvania Philadelphia, PA On behalf of: Christopher Nutting, Barbara Jarzab, Rossella Elisei, Salvatore Siena, Lars Bastholt, Christelle de la Fouchardiere, Furio Pacini, Ralf Paschke, Young Kee Shong, Steven I. Sherman, Johannes WA Smit, John Woojune Chung, Harald Siedentop, Istvan Molnar and Martin Schlumberger Disclosures • Companies: AstraZeneca, Bayer/Onyx, Eisai, Exelixis, Novartis, Oxigene, Plexxikon, Roche • Relationships: Advisory board consultant, honoraria, research grants, and primary investigator • As there are currently no FDA approved agents for progressive DTC, all agents I will discuss will be off label use or in the context of a clinical trial 2 Thyroid cancer: clinical pathology Papillary (87%) Follicular cells Differentiated Follicular (6%) Anaplastic (1%) Parafollicular cells Hürthle cell (3%) Medullary (2%) Treatment of Differentiated Thyroid Cancer includes: • Surgery – thyroidectomy • Radioactive iodine • Thyroid stimulating hormone (TSH) suppression • Recurrent progressive RAI refractory disease treated with sorafenib Carling T and Uldesman R. Cancer of the Endocrine System: Section 2: Thyroid Cancer. Principles of Clinical Oncology. 7th edition. Lippincott Williams and Wilkins. 2005. Howlader N et al. SEER Cancer Statistics Review; http://seer.cancer.gov/statfacts/html/thyro.html. Radioactive Iodine (RAI)-Refractory Differentiated Thyroid Cancer (DTC) • It is estimated1 that in the USA in 2013 there will be: – >60 000 new cases of thyroid cancer, and – 1850 deaths due to thyroid cancer • In approximately 5–15% of patients with thyroid cancer, the disease becomes refractory to RAI2,3 • Median survival for patients with RAI-refractory DTC and distant metastases is estimated to be 2.5–3.5 years4,5 • Patients often suffer multiple complications associated with disease progression 1. Howlader N et al. SEER Cancer Statistics Review; http://seer.cancer.gov/statfacts/html/thyro.html; 2. Xing M et al. Lancet 2013; 381:1058–69; 3. Pacini F et al. Expert Rev Endocrinol Metab 2012;7:541–54; 4. Durante C et al. J Clin Endocrinol Metab 2006;91:2892–99. 5. Robbins RJ et al. J Clin Endocrinol Metab 2006;91:498–505. FDG-PET Predicts Survival in Patients With Metastatic Thyroid Cancer Survival Distribution Function 1.00 FDG-negative 176/179 alive 0.75 FDG-positive 156/223 alive 0.50 0.25 Median survival = 53 months 0 0 10 20 30 Robbins et al. J Clin Endocrinol Metab. 2006;91:498-505. 40 50 Months 60 70 80 90 Genetics of Differentiated Thyroid Cancer: aberrant intracellular signaling Poorly differentiated • • RAS (25–30%) TP53 (20–30%) CTNNB1 (10–20%) BRAF (10–15%) Anaplastic Medullary Oncocytic Conventional Follicular Mutations in 70–75% • RAS (40–50%; lower in oncocytic) • PAX8/PPARg (30–35%; lower in oncocytic) • TP53 (21%) • PTEN (8%) • PIK3CA (7%) BRAF (2%) aBRAF Papillary Mutations identified in ~70% BRAFa (40–50%) RASb (7–20%) • RET/PTC (clonal; 10–20%) • EGFR (5%) • TRK (<5%) • PIK3CA (2%) Papillary DTC mutations are mostly V600E; 1–2% are K601E and others includes N-, H-, and K-RAS (predominantly NRAS and HRAS codon 61) Nikiforov YE et al. Arch Pathol Lab Med 2011;135:569–77; COSMIC database – Catalog of Somatic Mutations in Cancer bRAS Targeting Cell Signaling in Thyroid Cancer Tumor Cell RET/PTC Motesanib Sorafenib Sunitinib Vandetanib Cabozantinib Lenvatinib Endothelial Cell EGFR VEGFR-2 Vandetanib Ras B-Raf Sorafenib MEK ERK Ras PI3K Raf AKT mTOR S6K Sorafenib Everolimus Sirolimus • Growth • HIF1a • Survival • Inhibition of • Proliferation apoptosis • Migration MEK ERK PI3K Axitinib Motesanib Sorafenib Sunitinib Vandetanib Lenvatinib Cabozantinib AKT mTOR S6K • Growth • Migration • Survival •Angiogenesis • Proliferation EGFR, epidermal growth factor receptor; VEGFR, vascular endothelial growth factor receptor. Graphic adapted from Keefe SM, et al. Clin Cancer Res. 2010;16:778-783. Everolimus Sirolimus Targets of Kinase Inhibitors Compound Name VEGFR BRAF PDGFR KIT RET Other Sorafenib + + + + + FLT-3 Sunitinib + + + Axitinib + + + Motesanib + + + Pazopanib + + + Vandetanib + + EGFR Cabozantinib + + C-MET Lenvatinib + + FGFR Vemurafenib + + FLT-3 + BRAF V600E DTC, differentiated thyroid cancer; EGFR, endothelial growth factor receptor; FGFR, fibroblast growth factor receptor; PDGFR, platelet-derived growth factor receptor; TKI, tyrosine kinase inhibitor; VEGF, vascular endothelial growth factor; VEGFR, VEGF receptor. 1. Perez CA , et al. Biologics. 2012;6:257-265. 2. Pacini F. Expert Rev Endocrinol Metab. 2012;7:541-554. Targeted Agents: Phase 2 Clinical Data n PFS (months) PR SD PD Drug Key Baseline Characteristics Sorafenib (Brose) DTC + PDTC (90%) 47 20 38% 47% 2% Sunitinib (Cohen) DTC (74%); MTC (26%) 51 — 17% DTC 74% DTC 9% DTC Axitinib (Cohen) Papillary (50%); medullary (18%); follicular/Hürthle (25%/18%); anaplastic (3%) 60 18.1 30% 48% 7% Motesanib (Sherman) Papillary (61%); follicular/Hürthle (34%) 93 10 14% 67% 8% Pazopanib (Bible) PD and DTC (progression < 6 months) 37 12 49% — — Lenvatinib (Sherman) DTC (100%) 58 13.3 45% 46% 5% DTC, differentiated thyroid cancer; MTC, medullary thyroid cancer; PD, progressive disease; PDTC, poorlydifferentiated thyroid cancer; PFS, progression-free survival; PR, partial response; SD, stable disease. DECISION study design1 417 patients randomized from Oct 2009 to July 2011 • Locally advanced or metastatic, RAI-refractory DTC • Progression (RECIST) within the previous 14 months • No prior chemotherapy, targeted therapy, or thalidomide • • 400 mg orally twice daily Randomization 1:1 Placebo orally twice daily Stratified by: – – • Sorafenib geographical region (North America or Europe or Asia) age (<60 or ≥60 years) Progression assessed by independent central review every 8 weeks At progression: – – Primary endpoint • Progression-free survival Secondary endpoints Overall survival Response rate Safety Time to progression Disease control rate Duration of response Sorafenib exposure (AUC0–12) patients on placebo allowed to cross over at the investigator’s discretion patients on sorafenib allowed to continue on open-label sorafenib at the investigator’s discretion 1. Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 Key inclusion and exclusion criteria (1) Inclusion • Locally advanced or metastatic DTC (papillary, follicular including Hürthle cell or poorly differentiated) • RAI-refractory DTC – At least one target lesion without iodine uptake, or – Progression following treatment dose of RAI, or – Cumulative RAI treatment ≥600 mCi • Progressive disease within the last 14 months (RECIST) • Adequate TSH suppression (<0.5 mU/l) 1. Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 Key inclusion and exclusion criteria (2) Inclusion (cont.) • Not a candidate for surgery or radiotherapy with curative intent • Adequate bone marrow, liver and renal function • Eastern Cooperative Oncology Group (ECOG) performance status (PS) 0–2 Exclusion • Prior anti-cancer treatment with targeted therapy or chemotherapy 1. Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 Baseline disease characteristics Sorafenib (n=207) Placebo (n=210) Histology, investigator assessed, % Papillary Follicular Hürthle cell Missing 66.2 21.3 11.6 1.0 67.1 26.2 6.7 0 Metastases Locally advanced Distant 3.4 96.6 3.8 96.2 Most common target/non-target lesion sites, % Lung Lymph nodes (any) Bone Pleura Head and neck Liver 86.0 54.6 27.5 19.3 15.9 13.5 86.2 48.1 26.7 11.4 16.2 14.3 Prior thyroidectomy, % 100 99.0 Locoregional therapy or EBRT, % 40.1 43.3 400 mCi 376 mCi Median cumulative RAI activity EBRT, external beam radiation therapy 1. Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 Progression-free survival (by independent central review) n Median PFS, days (months) Sorafenib 207 329 (10.8) Placebo 210 175 (5.8) 100 PFS probability (%) 90 80 70 HR: 0.587; 95% CI: 0.454–0.758; p<0.0001 60 50 40 30 20 10 0 0 100 200 300 400 500 600 700 800 Days from randomization Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 CI, confidence interval; HR, hazard ratio; PFS, progression-free survival Overall survival 100 Survival probability (%) 90 80 70 60 Median OS 50 Sorafenib Not reached Placebo Not reached 40 30 HR: 0.802; 95% CI: 0.539–1.194 p=0.138, one-sided 20 10 0 0 100 200 300 400 500 600 700 800 900 1000 Days from randomization At progression: • 150 patients on placebo (71%) received open-label sorafenib • 55 patients on sorafenib (27%) received open-label sorafenib Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 CI, confidence interval; HR, hazard ratio; PFS, progression-free survival Other secondary efficacy endpoints Sorafenib n (%) Placebo n (%) 196 201 24 (12.2) 1 (0.5) <0.0001 0 0 – 24 (12.2) 1 (0.5) – Stable disease for ≥6 months 82 (41.8) 67 (33.2) – Disease control rate (CR + PR + SD ≥6 months) 106 (54.1) 68 (33.8) <0.0001 10.2 (7.4–16.6) NA – Total evaluable patients Response rate Complete response Partial response Median duration of response (PRs) months (range) CR, complete response; PR, partial response; SD, stable disease; NA, not assessed p value Maximum reduction in target lesion size (by independent central review) Maximum reduction in target lesion size (%) 60 50 40 30 20 73% of patients 27% of patients 10 0 –10 –20 –30 –40 –50 –60 –70 Sorafenib Placebo Maximum reduction is defined as the difference in the sum of the longest diameter of target lesions from baseline. Negative values refer to maximal reduction and positive values to the minimal increase. Treatment and dose modifications (double-blind period) Sorafenib (n=207) Placebo (n=209) 651 mg 793 mg 46.1 weeks (0.3−135.3) 28.3 weeks (1.7−132.1) Dose modification due to AEs, % Dose reduction Dose interruption 77.8 64.3 66.2 30.1 9.1 25.8 Permanent discontinuation due to AEs, % 18.8 3.8 Mean dose Median (range) treatment duration AE, adverse event Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 Most common treatment-emergent AEs (double-blind period) AE*, % Sorafenib (n=207) Any grade Grade 3/4 Placebo (n=209) Any grade Grade 3/4 Hand–foot skin reaction 76.3 20.3 9.6 0 Diarrhea 68.6 5.8 15.3 1.0 Alopecia 67.1 0 7.7 0 Rash/desquamation 50.2 4.8 11.5 0 Fatigue 49.8 5.8 25.4 1.4 Weight loss 46.9 5.8 13.9 1.0 Hypertension 40.6 9.7 12.4 2.4 Metabolic – lab (other) 35.7 0 16.7 0 Anorexia 31.9 2.4 4.8 0 Oral mucositis Pruritus Nausea Hypocalcemia 23.2 21.3 20.8 18.8 1.0 1.0 0 9.2 3.3 10.5 11.5 4.8 0 0 0 1.4 *National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) version 3.0 Brose M et al. Oral presentation at the American Society of Clinical Oncology Annual Congress 2013; abstract 4 CI, confidence interval; HR, hazard ratio; PFS, progression-free survival Serious adverse events and deaths (double-blind period) Sorafenib n=207 Placebo n=209 77 (37.2) 55 (26.3) Most frequent serious AEs*, n (%) Secondary malignancy • Squamous cell carcinoma of the skin Dyspnea Pleural effusion 9 (4.3) 7 (3.4) 7 (3.4) 6 (2.9) 4 (1.9) 0 6 (2.9) 4 (1.9) Grade 5 events (deaths), n (%) Drug-related** 14 (6.8) 1 (0.5) 6 (2.9) 1 (0.5) Serious AEs, n (%) * Occurring in ≥2.0% of sorafenib-treated patients ** Myocardial infarction (sorafenib); subdural hematoma (placebo) Sorafenib benefit by BRAF status (PFS) – Papillary histology only BRAF wild-type PFS probability (%) 100 80 Median PFS, days (months) Sorafenib (n=42) 278 (9.1) Placebo (n=42) 170 (5.6) HR: 0.58, 95% CI: 0.34–1.00, p=0.049 BRAF mutation 100 80 60 60 40 40 20 20 Median PFS, days (months) Sorafenib (n=32) 623 (20.5) Placebo (n=40) 286 (9.4) HR: 0.40, 95% CI: 0.20–0.80, p=0.008 0 0 0 200 400 600 800 Days from randomization 0 200 400 600 800 Days from randomization BRAF mutation did not predict PFS benefit from sorafenib (biomarker-treatment interaction p=0.393) Brose M et al. Oral presentation at the European Society of Medical Oncology (ECCO-ESMO) Annual Congress 2013 Sorafenib benefit by RAS status (PFS) RAS wild-type PFS probability (%) 100 80 Median PFS, days (months) Sorafenib (n=102) 329 (10.8) Placebo (n=104) 175 (5.7) HR: 0.60, 95% CI: 0.42–0.85, p=0.004 RAS mutation 100 80 60 60 40 40 20 20 0 0 0 200 400 600 800 Days from randomization Median PFS, days (months) Sorafenib (n=24) 167 (5.5) Placebo (n=26) 105 (3.4) HR: 0.49, 95% CI: 0.24–1.00, p=0.045 0 200 400 600 800 Days from randomization RAS mutation was not an independent prognostic factor for PFS Univariate (placebo arm only): mutant vs wild type RAS, HR=1.80; p=0.022 Multivariate (placebo arm only): mutant vs wild type RAS, HR=1.56; p=0.154 RAS mutation did not predict PFS benefit from sorafenib (biomarker-treatment interaction p=0.422) Brose M et al. Oral presentation at the European Society of Medical Oncology (ECCO-ESMO) Annual Congress 2013 UPCC 18310: Vemurafenib in patients with Progressive PTC with BRAF V600E Key Eligibility Criteria • Recurrent, unresectable or metastatic PTC • BRAFV600 mutation positive by cobas • RAI refractory • Evidence of progression within 14 months Cohort 1: VEGFR2i-naive (n = 26) Cohort 2: VEGFR2i-pretreated (n = 25) Vemurafenib 960 mg bid until disease progression or unacceptable toxicity • Prior chemotherapy allowed Primary end point: response rate per investigator in VEGFR2i-naive patients. Secondary end points: safety, duration of response, PFS, OS, PK, response rate in VEGFR2 inhibitor–pretreated patients bid, 2 times a day; OS, overall survival; PFS, progression-free survival; PK, pharmacokinetics; VEGFR, vascular endothelial growth factor receptor; VEGFR2i, vascular endothelial growth factor receptor 2 inhibitor. Brose et al. ECCO-ESMO 2013 Cohort 1: VEGFR2i-Naive Best Objective Response Max change in sum of diameters RECIST (%) 25.0 Cohort 1, N = 26 No confirmed objective response Confirmed objective response 0.0 –25.0 –30.0 –50.0 –75.0 Objective response n (%) [95% CI] CR, n (%) PR, n (%) SD ≥6 mo Clinical benefit (CR, PR, or SD ≥6 mo), n (%) [95% CI] 0 (0) 9 (35%) 6 (23%) 15 (58%) [0.37-0.77] –100.0 Each bar represents one cohort 1 patient AE, adverse event; CR, complete response; PR, partial response; SD, stable disease. 24 aPatients with at least 2 postbaseline tumor scans or progressive disease/withdrawal because of death or AE within first 2 cycles. Cohort 1: VEGFR2i-Naive Survival Kaplan-Meier Curves Censored OS PFS 1.0 Censore d Survival Probability Survival Probability 1. 0 0.8 0. 6 0. 4 Median PFS 15.6 mo (95% CI: 11.2–NR)a 0. 2 0.8 0.6 0.4 Median OS: Not reachedb 0.2 0.0 0. 0 0 5 10 15 20 0 patients continue therapy. 10 15 Months Months a13 5 bMedian follow-up time: 11.4 mo. Brose et al. ECCO-ESMO 2013 25 20 Summary: RAI-Refractory DTC • DTC is a vascular tumor that has been associated with increased activity of the MAPK pathways, and iodine-refractory patients have an average survival of 3 years • Results of phase 3 trials with sorafenib (DECISION) were positive, This agent was the FDA approved November 2013, and is first agent to be approved since doxorubicin in 1974. • Two additional phase 3 trials of lenvatinib (SELECT) and vandetanib (VERIFY) are ongoing • Additional MKIs have also shown activity in the Phase II setting, many of which target VEGFR-2, but also mTOR, MEK, MET and BRAF and BRAF V600E and will be needed in the second- and third-line setting DTC, differentiated thyroid cancer; MKI, multikinase inhibitor; mTOR, mammalian target of rapamycin; RAI, radioactive iodine; VEGFR, vascular endothelial growth factor. Thyroid cancer: clinical pathology Papillary (87%) Follicular cells Differentiated Follicular (6%) Anaplastic (1%) Parafollicular cells Hürthle cell (3%) Medullary (2%) Treatment of Medullary Thyroid Cancer includes: • Surgery – thyroidectomy • Thyroid stimulating hormone (TSH) replacement • Recurrent non surgical and metastatic disease treated with Cabozantinib and Vandetanib Carling T and Uldesman R. Cancer of the Endocrine System: Section 2: Thyroid Cancer. Principles of Clinical Oncology. 7th edition. Lippincott Williams and Wilkins. 2005. Howlader N et al. SEER Cancer Statistics Review; http://seer.cancer.gov/statfacts/html/thyro.html. Medullary Thyroid Cancer • From calcitonin-producing parafollicular C cells • Accounts for 2%-5% of thyroid cancers – ~1400 cases per year in US – Disproportionate number of thyroid cancer deaths – 350,000 Americans living with thyroid cancer • Heritable in 25% of cases • Mutations in the RET gene cause familial MTC– multiple endocrine neoplasia 2 (MEN2) • 30%-40% of sporadic MTC bear somatic RET mutations Plasma Markers in MTC • Calcitonin – Synthesized and excreted by C cells of the thyroid and by some medullary thyroid tumors – Diarrhea and flushing at high levels – Calcitonin levels can be affected by RET inhibition • Carcinoembryonic antigen (CEA) – Synthesized and excreted by some medullary thyroid tumors – Synthesized by other types of tumors as well Patients With Distant Metastasis at Diagnosis Have a Poor Prognosis • 10-year overall survival: 40% • Median overall survival: 3.2 years Roman et al. 2005. MTC: Initial Treatment • Complete surgical resection is the only curative treatment for MTC • Metastasis (lymph node or systemic) is present at diagnosis in 40%-50% of sporadic cases of MTC • Surgery : – Total thyroidectomy – Extent of surgery depends on stage of disease • Curable vs noncurable • Central neck dissection +/- Ipsilateral neck dissection or Contralateral neck dissection – Goal • Early disease: removal of all neoplastic disease • Advanced disease: airway protection MTC: Treatment • Radiation therapy – Adjunctive and palliative treatment for extensive neck or mediastinal disease – Palliative treatment for bony metastasis – May be effective in controlling complications associated with MTC activity in the neck and mediastinum – No evidence that radiation therapy improves survival – Radioactive Iodine is ineffective in the treatment of MTC!!! MTC: Treatment • Follow-up postsurgery – High level of calcitonin 2-3 months postsurgery indicates persistent disease – Most important prognostically is total calcitonin and the doubling time (DT) – Reoperation may allow removal of at least some neoplastic tissue, but less likely to prevent recurrence • Calcitonin levels normalize in 5%-35% of cases after re-operation – Radiation to the neck and mediastinum in cases of persistent elevated calcitonin levels can decrease the risk of recurrence (unlikely to affect survival) Risk Stratification Using Serum Calcitonin DT • Calcitonin DT highly predictive of mortality • Independent predictor in multivariate analysis, controlled for TNM stage • Rapid DT could identify stage II and III patients at higher risk for death Barbet. JCEM. 2005. MTC: Sites of Recurrent or Persistent Disease Optimal Imaging Strategies • • • • Cervical nodes and thyroid bed Lungs and mediastinum Liver and abdominal lymph nodes Bone CT, computed tomography; MRI, magnetic resonance imaging. Giraudet. JCEM. 2007. Neck ultrasound Chest CT Liver protocol MRI MRI spine and pelvis MTC: Treatment of Metastatic Disease • • No standard of care Rate or progression is variable – Some patients survive for years with metastatic disease • Traditional chemotherapy – Prior to 4/6/2011, doxorubicin was the only FDA-approved agent; relative risk (RR) <40%; poorly tolerated, short duration response – Dacarbazine-based regimens RR< 40% and generally short-lived – NCCN practice guidelines (2008) • Disseminated symptomatic disease – – – – – – Clinical trial (preferred) Radiation therapy for focal symptoms Sorafenib Dacarbazine-based chemotherapy Consider bisphosphonate therapy for bone metastases Best supportive care Rationale for RET as a Therapeutic Target • Activated by mutations in ~50% of cases (>60% of progressive cases presenting for clinical trials) • Somatic mutation of RET associated with poor prognosis • Limited expression outside the thyroid, potentially high therapeutic index ZETA Study: Vandetanib Significantly Prolonged PFSa vs Placebo PFS: 65% Relative Reduction in Risk of Progression1 ▬▬ CAPRELSA 300 mg Events/Patients 59/231 Progression-free Survival 1.0 ▬▬ Placebo 41/100 Median PFS not reached 0.75 (95% CI: 22.6 months, nonestimable) 0.50 16.4 months median PFS 0.25 (95% CI: 8.3-19.7) HR=0.35 (95% CI: 0.24-0.53) P<0.0001 0.0 0 6 12 18 24 30 36 33 6 1 0 0 0 Months Number at Risk CAPRELSA 300 mg Placebo • 231 100 173 47 145 30 118 24 CI=confidence interval; HR=hazard ratio. 1. CAPRELSA® (vandetanib) Tablets [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals LP. 2. Wells SA Jr et al. J Clin Oncol. 2012;30(2):134-141. 38 FDA Approves vandetanib in MTC 4/6/2011 • Approved for progressive or symptomatic disease only • MDs required to undergo Risk Evaluation and Mitigation Strategy (REMS) training for QTc prolongation detection – REMS program lays out a plan for EKG monitoring throughout therapy for all patients treated with vandetanib – Training itself takes approximately 2 hours • Starting dose 300 mg/d Cabozantinib Phase III in MTC Progression Free Survival by IRC 1.0 0.9 0.8 Probability 0.7 0.6 0.5 0.4 0.3 P< 0.0001 p<0.0001 0.2 0.1 0.0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Months Cabozantinib Placebo 121 78 55in tumor 31 response 12 •219 Significant difference rate 2 111 35 11 6 3 2 0 – 27% in cabozantinib vs 0% placebo; P<0.0001 • Median duration of response: 14.7 months COMETRIQTM (cabozantinib) Capsules [package insert]. Exelixis, Inc: San Francisco, CA. 1 0 FDA Approves cabozantinib in MTC 11/29/2011 • Approved for progressive or symptomatic disease only • Warnings about gastrointestinal perforations and fistula formations • Starting dose 140 mg/d Key Points: MTC for Oncologists • MTC has a distinct clinical presentation, genetics, and molecular targets compared with differentiated thyroid cancer • Importance of distinguishing progressive vs indolent disease (imaging and CEA DT) • Success of treatment will be strongly dependent on attention to kinase-related symptom management • REMS is required for vandetanib; oncologists are required to follow EKGs closely • Cabozantinib has black box warning about risk of fistula formation in regions of prior invasive disease and radiation • Either can be used in first or second line setting University of Pennsylvania Thyroid Cancer Therapeutics Program • Brose Translational Research Lab – – – – • Susan Mandel, MD Ara Chalian, MD Douglas Fraker, MD Robert Lustig, MD Virginia LiVolsi, MD Zubair Baloch, MD Steve Keefe, MD Daniel Pryma MD • Marcia Simpson Brose is a Damon Runyon-Siemens Clinical Investigator • Many community endocrinologists who have referred their patients, and the patients who have agreed to participate in our trials Experimental Therapeutics Program – – • Yvette Cruz, RN Carolyn Grande, RN, CRNP Thelma McCloskey Parna Prajapati Ramkrishna Makani Jillian Stanley Thyroid Cancer Interest Group – – – – – – – – Raya Terry, MD Tatyana Kuznetsova, PhD Waixing Tang, MD Zakkiyya Posey Thyroid Cancer Clinical Trials Unit – – – – – – • • Andrea Troxel, PhD Peter O’Dwyer, MD Pathology/Imaging – – Michael Feldman, MD, PhD Laurie Loevner, MD