Carotid Artery Disease
advertisement

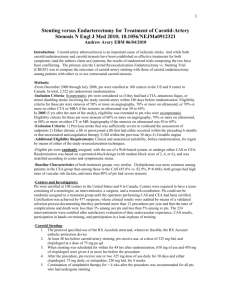
SVS Clinical Research Priorities: Carotid Disease John J Ricotta MD FACS Background: Public Health Impact (AHA Heart Disease and Stroke Statistics 2011 Update, Circ 2011;123: e18-e209) 7M strokes, 13M silent infarctions 795k strokes/yr – 610k new, 185k recurrent - 87% (690k) ischemic (140-200k CAD) - 2/3 unheralded - 150k fatal (16.7% of all CVD) - 15-30% survivors permanent serious disabled, only 1/3 completely recover 250-500 K TIA/yr – 17% stroke w/in 90 days Early RX of TIA/Stroke reduces death and disability from recurrence Background: Imaging CDUS preferred for initial imaging No agreement on best imaging protocols CDUS, CTA, MRA, DSA Neck imaging not routinely incorporated into acute stroke protocols No agreement on role of imaging in asymptomatic patients No agreement on follow up protocols Background: Therapy CEA beneficial for Sx and Asx CS CAS beneficial for Sx pts CEA decreasing CAS increasing 86% /14% CREST: CEA reduced stroke/death CAS reduced MI Composite endpoints equivalent 90% of Interventions on Asymptomatic pts. NNT 16-19 Role of BMT? CEA vs CAS Met Analysis (Murad et al JVS 2011;53:792-7) Background: Economic Impact (AHA Heart Disease and Stroke Statistics 2011 Update, Circ 2011;123: e18-e209) Annual stroke Cost 40.8 Billion -direct costs 25.2 Billion Lifetime Cost / stroke $140,048 CEA cost effective even Asx pts - low stroke rate, longevity and high cost of stroke CEA more cost effective than CAS d/t procedural costs ($4,000/ case) Background Economic Impact Carotid and Neuroimaging costs are a significant portion of health care costs - CMS reimbursed 3m CDUS/yr - CT/ MRI cost likely much more Defining appropriate algorithms for case finding and follow up is important Identifying imaging protocols that identify stroke prone lesions is important -avoid unnecessary Interventions in Asx pts. Current Evidence Review recent Guidelines from ASA/ACC/AHA and SVS to Identify clinical issues that require further study Review SVS Membership recommendations Issues divided based on several criterion - Resource Utilization - Patient Selection for Intervention - Comparison of Alternative Therapies - Conditions with little data to guide treatment Guidelines: Imaging No Benefit to population based Screening - bruit alone not an indication High Risk screening may be indicated - smokers, PVD, CAD (L main), age >65, multiple factors increase yield F/U with disease or after intervention indicated but no agreement on intervals or what to do with pts who are “normal” after intervention Guidelines: Imaging Plaque character, surface ulceration, “hits” on TCD, asymptomatic lesions on brain imaging all associated with increased stroke risk Impression but no evidence that severity (60-79 vs. 80-99) of Asymptomatic Stenosis is related to stroke risk Duplex, CT and MR all utilized to describe plaque character but with inconsistent results Silent on imaging protocols in acute stroke Imaging in Acute Stroke Patients “Brain attack” protocols focus on MRI with intracranial MRA -neck MRA or carotid duplex is not standard “Just in time” duplex not mentioned in patients with ANS, EXPRESS data shows expedited evaluation reduces recurrent Sxs This is inconsistent with recommendation for early CEA in acute stroke patients Selection of therapy depends on distribution of intracranial and extracranial disease Imaging Questions When is screening Asymptomatic Pts for CS indicated? How do we define “stroke prone” lesions? Impact of early duplex in TIA pts What imaging is needed in the acute stroke patient IC vs EC ? What follow up is appropriate for CS or after carotid intervention? Potential Studies Identify “high risk” subgroups to screen with CDUS Identify/ Compare reproducible, available techniques to identify plaque and surface characteristics to identify “high risk” lesions Determine natural history of 60-79% vs 80-99% stenosis Evaluate “just in time” imaging in TIA pts Evaluate yield of routine neck imaging in acute stroke patients (race, age) Utility of post intervention imaging Guidelines: Patient Selection Intervention for Sx > 50%, Asx >60%, >70% provided AHA procedural guidelines met CEA preferred to CAS in good risk pts. CAS preferred in High risk SX pts CAS an alternative in Sx and Asx pts within AHA guidelines In Sx pts intervention preferred within 2 weeks of Symptoms Guidelines: Patient Selection Acknowledge the dysjunction of the “composite” endpoints of stroke, death, MI Definition of “Medical High Risk” Acknowledge need for Medical arm in Asymptomatic patients Intervention for High Grade recurrent stenosis despite poor data Guidelines Unanswered Questions Definition of “High Risk” CAS / CEA pts Ideal stent , EPD Long term sequelae of “silent hits” on MRI, chemical MI Recommendations on combined carotid and coronary disease Patient Selection Questions Medical Treatment vs intervention in Asx pts. (2 ongoing trials underway) Long term cognitive impact of MRI lesions How to reduce MI in CEA and Stroke in CAS What is contemporary CEA/CAS High Risk When to intervene in restenosis Carotid interventions in CABG pts Potential Studies CAS/CEA/Med Rx in asymptomatic pts - can combine with lesion characterization Long Term Cognitive Function CAS/CEA/BMT Intervention vs observation in Asx restenosis Role of Carotid Screening in CAD pts -identify “high yield” group Revascularization Strategies in CABG pts -unilateral Asx >80%, b/l Asx >70%, Sx >50% ( evaluate aortic arch) Potential Studies How to improve results of Interventions - Role of CAD screening in Asx CEA pts - Role of anatomic selection in CAS -“Learning curve” in CAS - Influence of stent design, EPD type in CAS Guidelines: Insufficient Data to Guide Treatment Intervention in acute stroke Crescendo TIA Stroke in Evolution FMD - symptomatic and asymptomatic Carotid Dissection Questions Define acute stroke pts who will benefit from urgent/emergent intervention -size infarct IC vs EC disease Treatment of SIE, Crescendo TIA Treatment for FMD – sx and asx -observation, AP, AC, CAS Carotid dissection – if/when to intervene, AC vs. AP Potential Studies Urgent (<48hrs) vs. Early (<2wks) intervention in acute stroke –role of brain imaging and arterial anatomy in selection FMD – Asx: Antiplt vs. observation Sx: Antiplt vs. CAS Dissection – AC vs. AP vs. CAS in symptomatic pts Early intervention vs. Medical Rx for Crescendo TIA and SIE, selection factors Priorities CAS/CEA/BMT in Asymptomatic pts Optimal imaging protocols Improving results of Interventions Management of Pts with combined disease, recurrent stenosis Management of Acute Neurological Syndromes Unusual Conditions