PowerPoint - Interactive Metronome
advertisement

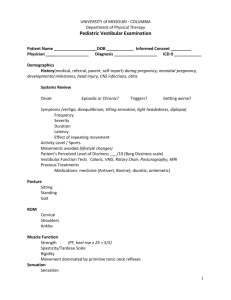
Fall Risk Reduction Program Designing an Exercise Program Module #3 Shelley Thomas, MPT, MBA Dara Coburn, M.S., CCC-SLP Fall Risk Reduction Program: Review of Modules 1 & 2 In the first module we reviewed the premise of the Fall Risk Reduction Program, including the inclusion criteria for patient selection The second module reviewed patient assessment Identifying patients at risk of falling Evaluating patients in a dual task condition to simulate “real life” situations Fall Risk Reduction Program: Module 3 In this module, we will delve further into patient assessment. You have identified patients at risk for falling and evaluated performance under dual task conditions. Now you must further do further assessment to identify the system(s) of balance most responsible for the falls, and develop an plan of care to address the system(s). Agenda Screening & Assessing Balance Impairments: Information to gather in order to design an exercise program Exercise selection Designing a program Agenda Screening & Assessing Balance Impairments: Information to gather in order to design an exercise program Exercise selection Designing a program Multifactorial Risk Assessment Focused History Physical Examination Functional Assessment Environmental Assessment American Geriatric Society Clinical Practice Guidelines: Prevention of Falls in Older Adults Multifactorial Risk Assessment: Focused History History of falls – need detailed description of the fall circumstances, frequency, symptoms Medication review History of risk factors – acute & chronic medical issues Multifactorial Risk Assessment – Physical Exam Physical function - Gait, balance (including postural reflexes), mobility, and lower extremity joint function Neurological function – Cognitive evaluation, peripheral nerve function, proprioception, reflexes, and tests of cortical, cerebellar, & extrapyramidal function Muscle strength Cardiovascular status – Heart rate, postural pulse, blood pressure Visual acuity Vestibular function (oculomotor tests, positional testing) Examine feet and footwear Multifactorial Risk Assessment – Functional Assessment Assess activity of daily living (ADL) skills Perceived functional ability and fear of falling Multifactorial Risk Assessment – Environmental Assessment Home safety Other environment factors as needed Turning the multifactorial risk assessment into an exercise program – What to do with all this information? Stratify the Patient Problems into Systems of Balance Musculoskeletal System Proprioceptive System Oculomotor System Vestibular System Cognition/Communication Musculoskeletal System Muscle, tendons, ligaments, bones, joints, and associated tissues that move the body and maintain form Key muscle groups associated with walking and upright balance reactions: Hip flexors Hip extensors (especially gluteous maximus) Hip Abductors (especially gluteous medius) Knee extensors (quadricepts Knee flexors (hamstrings) Plantarflexors (gastrocnemius, soleus) Dorsiflexors Upper and lower abdominal muscles Proprioceptive System Proprioception is the unconscious awareness of body position. It tells us about the position of our body parts in relationship to each other and the environment. It allows us to have a knowledge of how much force and speed the muscle is required to generate in order to accomplish a specific movement which results in appropriately graded muscle control. Oculomotor System Is the control system that coordinates the 12 muscles which accurately direct our eye movements. Three main types of Oculomotor Skills: Saccades – The ability to quickly and accurately make eye movements or jumps from one target to another. Fixation – The ability to maintain steady visual attention on a target. Pursuits – The ability to smoothly follow a moving target. Vestibular System System of the body that is responsible for spatial orientation and balance. The vestibular system sends information to the brain about the location of one's head in space. Vestibular, Oculomotor, Proprioception Systems: Need at least two In order to maintain balance, at least two of these systems must be sending balance information to the brain at any time. Examples: If in the dark, brain can use proprioceptive and vestibular inforamation to remain upright against gravity. If have lower extremity amputation, can use vestibular and oculomotor systems. If have labrynthiasis impacting vestibular system, can use oculomotor and proprioceptive information. Cognition & Communication Systems (involved in dual tasking) Cognition is the ability to think and process information Attention, memory, processing, problem solving, judgment, impulse control, and executive skills. Communication is the ability to exchange and comprehend language. Naming, word finding, following directions, answering questions, speaking, and writing. How much of the “cognitive pie” does mobility take? If maintain balance “hogs” resources, decreases cognitive and communication skills. Places person in an either/or situation – can maintain balance or focus on cognitive task. Sample Patient Problem List Musculoskeletal Peripheral Neuropathy Proprioception Oculomotor Vestibular X Lower extremity strength rated 3/5 X Flexed posture X Inadequate footwear X X X Decreased visual acuity due to diabetic retinopathy X Decreased problem solving skills Impaired balance reactions Cognition X X X X Now that you have stratified the problems into the systems of balance, you can design a plan of care that incorporates Interactive Metronome Why include Interactive Metronome in the plan of care? Movement Requires Directed attention Pathologies that disrupt motor timing and sequencing lead to inaccurate movements IM & Dual Tasking IM requires a patient to focus on auditory stimuli and make a motor response to hit the trigger on the beat. Must decide if need to slow down, speed up, or remain consistent. Computer can measure performance in milliseconds, so act at same speed as muscular contractions. Helps patients identify their own timing tendency and learn how to counteract own tendencies. Fall Risk Reduction Program Exercises This library of exercises are suggestions. Concept is to design exercises, using the Interactive Metronome that target specific problem areas Center treatment interventions around long and short term goals that are important to the patient. Goal selection was discussed in the second module Download can be found on course materials page Musculoskeletal System Exercises *Photos and exercise descriptions available on course materials page Leg Squats Alternate Stepping Lunges Stepper with Weights Heel Raises Bridging Long Arc Quads Abdominal Crunch Taps Ups Postural Alignment Lateral Tap Ups Postural Alignment with Marching Proprioceptive System Exercises *Photos and exercise descriptions available on course materials page Clock Clapping with Eyes Closed, Seated Uneven Surface with Eyes Open Clapping with Eyes Closed, Standing Uneven Surface with Eyes Closed Oculomotor System Exercises *Photos and exercise descriptions available on course materials page UNO Poster Board Visual Sequencing Visual Memory Recall/recognition Vestibular System Exercises *Photos and exercise descriptions available on course materials page Head Movement in Supine Sidelying to Sit with Head Rotation Head Movement in Sitting Visual tracking focal item Head Turns with Reaching Across Midline In Sitting, Head stationary, Saccades Head Turns with Walking Using the in-Motion Triggers Rolling Seated, Reaching Across and Behind to hit target Cognition/Communication System Exercises *Photos and exercise descriptions available on course materials page STROOP Activities Yes/No Questions Selected and Divided Attention Aphabetizing Naming Visual Attention Sorting Word Finding Memory Sequencing Melodic Intonation Picture Identification Impulse Control Intelligibility Drills Following Directions Safety Awareness Oral Motor Exercises Setting Table Fall Risk Reduction Poster Overview Fall Risk Reduction Best Practices Kit Contains: 1 – STOOP Board (12” x 18”) 5 – Fill-in-the-Blank Cards (4” x 11”) 5 – Melodic Intonation Cards (4” x 11”) 15 –Object Cards (7½” x 6”) 1 set – 1 – 12 Numbered Cards (8½” x 4”) 1 set – Yes/No Cards (4” x 8½”) 1 set – 1 – 25 Numbered Cards (4” x 3”) 15 – Word Cards (2½” x 3) 1 set – Various Sized Squares Integrating Kit Items for Fall Risk Reduction Tasks 1 – 12 Numbered Cards Toe Tapping Clock Various Sized Squares Object Cards Visual Memory Memory Naming Picture Identification 1 – 25 Numbered Cards STOOP Board Word Cards STROOP Activities Alphabetizing Yes/No Cards Fill-in-theBlank Cards Melodic Intonation Cards Sorting Sequencing Yes/No Questions Word Finding Melodic Intonation "Homework" Complete following worksheet to develop a plan of care for your patient. Use the same patient as in Module #2. Post-test Complete post-test to receive link for Module # 4 of 6 Materials Page This video PowerPoint Module 3 Homework Exercise Guide Poster Best Practices Kit www.interactivemetronome.com/index.php/ fall-risk-coaching QUESTIONS? You can call or email us. We’re here to help! Call 877-994-6776: Opt. 3 – Education imcourses@interactivemetronome.com Opt. 5 – Technical Support support@interactivemetronome.com Opt. 6 – Clinical Support clinicaled@interactivemetronome.com Opt. 7 – Marketing newsletter@interactivemetronome.com