Traumatic Brain Injury (TBI) Rehabilitation Programs
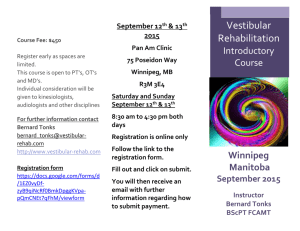
advertisement
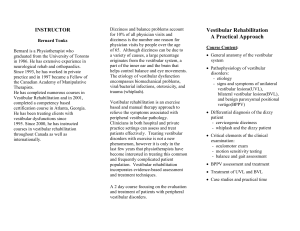
Traumatic Brain Injury (TBI) Rehabilitation Programs for Younger Children and Adolescents Vanderbilt Bill Wilkerson Center: Pi Beta Phi Rehabilitation Institute Populations Served • Since 1988, the mission of the Pi Beta Phi Rehabilitation Institute at Vanderbilt Bill Wilkerson Center has been service to children and adults with acquired brain injuries. Services Provided • Our services focus on the most primary and persistent concerns after post acute recovery from TBI: memory, executive functions, academic learning skills, speechlanguage abilities, & social communication. • Additionally, we provide therapies to improve functional selfcare, safety, mobility, strength, range of motion, balance and coordination, and feeding and swallowing. • Depending upon the age of the client, our therapy programs are aimed at readiness for school, school reentry, classroom placement, and selection of appropriate supports for academic success. Age 3 to 10 Therapy Services • Speech-Language Pathology: Evaluation and tx of cognitivecommunicative & academic skills, and social communication. • Occupational Therapy: Evaluations and tx to address physical, visual, perceptual, and cognitive abilities limiting functional independence, safety, and school academic success. Pre-school/School-Age/Academic • Develop language-literacy and handwriting skills, • Improve executive functions and attention and class room performance • Assistance with IEP and classroom/school placement. Age 11 – 21 Therapy Services • Speech-Language Pathology: Evaluation and treatment targeting cognitive-communicative deficits, academic skill development, and social communication. • Occupational Therapy: Assessment and treatment targeting physical, visual, perceptual, and cognitive deficits that influence independence in activities of daily living, safety, and academic success. Driver Evaluation/Training • Physical Therapy: Assessment and treatment targeting physical problems, such as decreased mobility, balance, coordination, dizziness, weakness, that influence independence and safety in daily activities. Middle School, High School, & College Academic Entry/Re-entry • Conduct a comprehensive evaluation of the student’s cognitive deficits to identify barriers to academic success. • Comprehensive treatment plan is developed with goals targeting reading comprehension, listening skills, speech, writing, attention, and memory Physical Therapy • Evaluation of balance and vestibular function, including a neurological screen – – – – – Oculomotor function Vestibular screening BPPV assessment (video goggles) Dynamic visual acuity/Gaze stability ( inVision computerized testing) Dynamic gait assessment • Examine use of sensory cues for balance (vestibular, visual, somatosensory) – Computerized dynamic platform posturography (Neurocom Smart Equitest) Physical Therapy • Balance/vestibular rehabilitation – Oculomotor training – Vestibulo-ocular-reflex (VOR) training – Functional balance retraining – Dynamic gait training • Dual-task activities to incorporate cognitive skills • Incorporate relevant functional tasks, including sports specific activities Balance Disorders Laboratory (BDL) • The BDL is a diagnostic clinic where specially-trained audiologists conduct tests to help physicians determine the cause of dizziness, disequilibrium and vertigo. • The BDL specializes in unique treatment options, and assess conditions using the most current testing techniques and technologies (e.g. head impulse, rotational, and videonystagmography testing). Driver Evaluation and Training • Evaluate patients to determine if they are able to safely drive a vehicle in a variety of environments. • If patient is able to benefit from intervention – train patients to drive without risk. – train the use of adaptive driving equipment. How to refer… Multidisciplinary TBI Clinic • Collaboration between PBPRI, Acute Care SLP Service, and Trauma Surgery • Director – Oscar Guillamondegui, MD