pptx format - North Central Region of the WOCN
advertisement
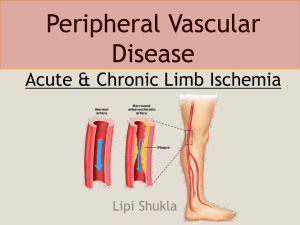
The Voyage to Peripheral Arterial Disease Management…Are We Missing the Boat? Carol Bohanon DNP, FNP-BC, CWS, CFCN September, 2014 Disclosure Relevant Financial Relationships NONE Off-Label Investigational Uses NONE Objectives • Identify signs & symptoms of lower extremity peripheral arterial disease (PAD) • Significance of early recognition and treatment options for PAD • Discuss tests and interventions specific to arterial disease • Describe pharmacologic therapies for treatment of arterial disease • Review arterial wound care Resources Guideline Statements for PAD: Management of Patients With Peripheral Artery Disease (Compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations). J Am Coll Cardiol. 2013;60:1555-70. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45 Suppl S:5A–67A. Performance measures for adults with peripheral artery disease. J Am Coll Cardiol. 2010;56:2147-81. Arterial Disease of the Lower Extremity Arterial Occlusive Disease • Plaque in arterial blood vessel wall narrows over time Arterial Occlusive Disease Asymptomatic: Claudication: reproducible pain or tightness in calf or thigh after walking a certain predictable distance Rest Pain: pain that occurs with advanced atherosclerosis when limbs are in a supine position Tissue Damage: not enough oxygen to support tissue growth, ulcer occurs Clinical Presentation of PAD Acute Lim b Ischem ia Chronic Lim b Ischem ia Stable Claudication Asym ptom atic PAD Adapted from Hirsch AT. Fam Pract Recertification. 2000;15(suppl):6-12. Survival for PAD patients Overall Mortality Rate: Claudicant patient 2.5 x ↑ SURVIVAL FOR PAD PATIENTS IC: intermittent claudication CLI: critical limb ischemia J Vasc Surg 2007;45,Suppl S Risk Factors Race: Non-Hispanic blacks (2 fold) Gender: Male 2:1 Age: > 65 (2 fold) Smoking (3 fold) Diabetes mellitus (4 fold) Hypertension J Vasc Surg 2007; 45, Suppl S Risk Factors Dyslipidemia (2 fold) Inflammatory markers Hyperviscosity & hypercoagulable state Hyperhomocysteinemia Chronic renal insufficiency Good History & Examination Must specifically ask about leg pain, claudication, and rest pain symptoms Many patients/family think it is a normal part of aging. Arterial Disease Presentation Atrophic, shiny skin Lack of pedal hair Yellow, thickened nails Decreased pulses Ulcers Edema of extremity – dependency INTERMITTENT CLAUDICATION “Exertional pain involving the calf that impedes walking, resolves within 10 minutes of rest, and neither begins at rest nor resolves on walking” “Rose Criteria” Bull World Health Organ 1962;27:645-58 Intermittent Claudication Exertional pain: “Fatigue” “Cramping” “Tightness” Calf > Thigh > Buttock Relief with standing Symptoms consistent from day to day Differentiating True from Pseudoclaudication Variable Character Exertional Symptoms with standing Relief Distance to symptoms Intermittent Claudication Pseudoclaudication Cramp, tight, fatigue Tingling, weak, clumsy yes yes or no no yes Stop, stand Must sit Consistent Inconsistent Arterial Pulse Exam 0 = absent pulse 1 = faint, but detectable 2 = reduced – can count pulse 3 = normal pulse 4 = bounding Lower Extremity Arterial Pulse Exam A: Femoral B: Popliteal (medial) C: Dorsalis pedis D: Post-tibial • Indicate presence of bruit • Symmetrical • Asymmetrical Ankle Brachial Index (ABI) Categorize Severity Using ABI Criteria (Ankle Brachial Index) Severity Resting ABI ’s Normal 1.00- 1.4 Borderline 0.91-0.99 Mild 0.80-0.90 Moderate 0.50-0.80 Severe <0.50 Values > 1.4 “non-compressible” JACC 2013;61:14 Ankle Brachial Index (ABI) ABI= Lower extremity systolic pressure Highest brachial artery systolic pressure Right Arm Pressure 136 mm Hg Highest Right Pedal Pressure 154 mm Hg Right ABI 154/140= 1.1 Left Arm Pressure 140 mm Hg Highest Left Pedal Pressure 54 mm Hg Left ABI 54/140 = 0.4 Scenarios where ABI lack accuracy: • Non compressible vessels • Elderly • Diabetes • Renal failure • Iliac artery disease (isolated internal iliac) • If claudication symptoms and normal ABI, exercise ABI should be done. Circulation 2006;113;e463 Arterial Vascular Study Doppler Waveform Normal Doppler Arterial Signal Triphasic Biphasic Abnormal Doppler Arterial Signal Reduced Bi. Monophasic Absent Transcutaneous Oximetry (TcP02) Supine (15 minutes) Elevation (3 minutes) Dependent (10 minutes) Healing range Grey zone Unlikely to heal >40 20 to 40 <20 Survival is directly related with ABI severity J Vasc Surg 2007;45 Suppl S:5A Coexisting Vascular Disease • Coronary artery disease (44.6 %) 25% symptomatic • Cerebral artery disease (16.6 %) • Renal artery disease (23-42%) > 50 % stenosis J Vasc Surg 2007;45,Suppl S 60 year-old man is evaluated for a 1 year history of progressive right leg pain. Vascular examination reveals diminished pedal pulses. Which of the following features will be most useful to distinguish between intermittent claudication and pseudoclaudication? 1. History of nicotine addiction 2. Symptoms brought on by exertion 3. Soft bruit over the right common femoral artery. 4. ABI of 0.8 on the right and 0.85 on the left. 5. Symptom relief with sitting only 60 year-old man is evaluated for a 1 year history of progressive right leg pain. Vascular examination reveals diminished pedal pulses. Which of the following features will be most useful to distinguish between intermittent claudication and pseudoclaudication? 1. History of nicotine addiction 2. Symptoms brought on by exertion 3. Soft bruit over the right common femoral artery. 4. ABI of 0.8 on the right and 0.85 on the left. 5. Symptom relief with sitting only Arterial Disease Initial Treatment Risk Factor Modification: Reduce high cholesterol Tobacco cessation Tight glucose control Reduce hypertension Avoid sedentary lifestyle Claudication Treatment TASC II Guidelines: • Cilostazol (Pletal) 100 mg PO daily • First-line pharmacotherapy (3 – 6 months) for the relief of claudication symptoms (Inter-Society Consensus for the Management of. Peripheral Arterial Disease (TASC II) • Drug class: Antiplatelet agent • Contraindicated in patients with heart failure TASC II J Vasc Surg 2007;45 Suppl S:5A J Am Coll Cardiol 2011;58 (19) Claudication Treatment TASC II Guidelines: • Pentoxifylline (Trental) 400 mg ORALLY three times a day with meals • Considered second-line alternative • Class: Hemorheologic • Reduces blood viscosity and improves erythrocyte flexibility, microcirculatory flow, and tissue oxygen concentrations TASC II J Vasc Surg 2007;45 Suppl S:5A J Am Coll Cardiol 2011;58 (19) Morbidity Reduction GOAL: reduce risk of MI, stroke, & vascular death in individuals with symptomatic (IC, CLI, IR or surgical revasc, amputation related to ischemia) & NONSYMPTOMATIC lower extremity PAD with ABI ≤ 0.90 Aspirin 325 mg daily and/or Clopidogrel 75 mg daily Assess bleeding risk NO benefit of anticoagulation therapy (warfarin) TASC II / JACC 2011;58(19) Non-diabetic 76 year-old male with remote tobacco use presents with claudication at 3 block, reduced biphasic Doppler signals, and ABI of .89. No hx of CHF or ulcers. Initial treatment should include: 1. Encourage activity 2. Cilostazol 100 mg BID 3. Monitor & treat risk factors for PAD 4. Appropriate antiplatelet therapy 5. All of the above Non-diabetic 76 year-old male with remote tobacco use presents with claudication at 3 block, reduced biphasic Doppler signals, and ABI of .89. No hx of CHF or ulcers. Initial treatment should include: 1. Encourage activity 2. Cilostazol 100 mg BID 3. Monitor & treat risk factors for PAD 4. Appropriate antiplatelet therapy 5. All of the above CLEVER Study Supervised Exercise vs Stenting for Intermittent Claudication Patients: Intermittent claudication due to aorto-iliac PAD Supervised exercise 111 patients Primary Stenting Optimal medical management (cilostazol) Primary efficacy outcome assessed @ 6 months Circulation. 2012;125:130-9. Conventional Angiography Advantages • Most sensitive (calcified vessels) • Angioplasty/stenting Disadvantages • Invasive • Iodinated contrast • Bad outcome 1:1000 CLEVER STUDY SUPERVISED EXERCISE VS STENTING FOR INTERMITTENT CLAUDICATION Patients: Intermittent claudication due to aorto-iliac PAD Change in peak walking time @ 6 months P-value Supervised exercise: 5.8 ± 4.6 minutes 0.04 Stenting: 3.7 ± 4.9 minutes 0.001 0.02 Opt med therapy (cilostazol): 1.2 ± 2.6 minutes Circulation. 2012;125:130-9. Treatment Guidelines: Canadian Walking Program • Supervised exercise should be part of the initial treatment for all PAD patients • Treadmill or track walking to reproduce symptoms 30 – 60 minutes/session, 3 sessions per week for 3 months TASC II J Vasc Surg 2007;45 Suppl S:5A J Am Coll Cardiol 2010;56;2147 Indications for Revascularization Absolute: Rest Pain Non-healing ulceration Relative: Life-style limiting symptoms Diagnose PAD Risk Factor Modification No limitation Life-style limiting claudication Exercise program Critical limb ischemia* Define anatomy: Angiogram, CTA, MRA Revascularize: Endovascular, Surgical *rest pain, non-healing ulcers, gangrene CT Angiography Advantages • Non-Invasive • Accuracy • Multi-assessment Disadvantages • No angioplasty/stenting • Iodinated contrast MR Angiography Advantages • Non-invasive • No iodinated contrast Disadvantages • Less Specific (overcalls stenoses) • No angioplasty/stenting • Nephrogenic systemic fibrosis Creatinine clearance cutoff: 30 ml/min 5 Year Primary Patency Rates Angioplasty±Stenting Bypass Grafting 80% 80% Iliac 70% Vein 60% 50% 20% Synthetic Femoral Popliteal Tibial 70% 60% 65% 40% 50% 10% BYPASS VERSUS ANGIOPLASTY IN SEVERE ISCHAEMIA OF THE LEG (BASIL) TRIAL: Severe lower limb ischemia (rest pain, ulceration, gangrene) Bypass surgery 452 patients Balloon angioplasty J Vasc Surg 2010;51:5S-17S BYPASS VERSUS ANGIOPLASTY IN SEVERE ISCHAEMIA OF THE LEG (BASIL) TRIAL: Amputation-free survival Overall survival J Vasc Surg 2010;51:5S-17S Treatment Guidelines: Critical limb ischemia • Estimated life expectancy ≤ 2 years or autogenous vein is not available, balloon angioplasty is reasonable (II B) • Estimated life expectancy > 2 years and autogenous vein is available, bypass surgery is reasonable (II B) JACC 2011;58:2020 Consultation with Vascular Surgeon or Interventional Radiologist Angioplasty Revascularize when possible Endovascular angioplasty and/or stenting (proximal/smokers) Surgical arterial bypass (distal/diabetes) Bypass surgery Poor Invasive or Surgical Candidate Medical comorbidity Lack of suitable outflow vessel Patient preference Therapies to augment arterial blood flow Cardiac gaited pump Circulator Boot ® Non-cardiac Gaited Pumps ArtAssist™ Plexi- Pulse ® Aircast Arterial Flow ® Arterial Ulcers Therapy Hyperbaric Oxygen Therapy (HBOT) Indicated and insurance payment for: Osteomyelitis Diabetic ulcers not moving toward closure after 30 days Acute traumatic ischemia Enhancement of healing in selected problem wounds, infection 78 year-old nondiabetic man with thigh/calf claudication, smoker, renal cancer, Cr 0.9 who presents with a traumatic plantar surface foot ulcer. Doppler signals are abnormal at the superficial femoral level with TCPO2s of 30/10/40, pulse exam: fem 3, pop 1. Most expedient treatment to improve arterial blood flow: 1. Medical management with supervised Canadian walking program 2. Arterial pumping of the lower extremity 3. Angiogram +/- angioplasty/stenting 4. Vascular surgical consult for distal pedal arterial bypass 78 year-old nondiabetic man with thigh/calf claudication, smoker, renal cancer, Cr 0.9 who presents with a traumatic plantar surface foot ulcer. Doppler signals are abnormal at the superficial femoral level with TCPO2s of 30/10/40, pulse exam: fem 3, pop 1. Most expedient treatment to improve arterial blood flow: 1. Medical management with supervised Canadian walking program 2. Arterial pumping of the lower extremity 3. Angiogram +/- angioplasty/stenting 4. Vascular surgical consult for distal pedal arterial bypass Treatment of Arterial Ulcers Arterial Ulcers •Discrete edge •Pale base / eschar • Atrophic skin • Lack of pedal hair • Severe pain – rest pain • Located on heel, toe, foot, trauma Arterial ulcers • Optimize blood flow • • • • • Proactive care Natural warmth Control edema Consider debridement Pain Management Indications for Amputation Absolute: Severe rest pain with no revascularization option Limb gangrene Life threatening infection Relative: Life-style limiting symptoms Amputation for Critical Limb Ischemia Below knee: • 10% perioperative mortality mortality rate @ 1 year = 25% • 60% primary healing rate • 15% will need future AKA TASC II J Vasc Surg 2007;45 Suppl S:5A Wound Dressing Decision Tree Dry Wound Hydrogel: Curasol Wound’ Dres, Silvasorb, Biafine Minimal Wound Drainage Hydrogels: Curasol, Woun’Dres, Silvasorb, Biafine Gauze: Xeroform, Excilon, Nu Gauze, Adaptic Alginates: Sorbsan, Restore, Kaltostat , Algicell Hydrofibers Aquacel, Aquacel AG, Maxorb AG Iodosorb: Mixed with Curasol Collagen: Fibracol, Promogran, Prisma, Medifil Moderate Wound Drainage Hydrogels: Curasol, Woun’Dres, Silvasorb, Biafine Gauze: Xeroform, Excilon, Nu Gauze, Adaptic, Curasalt, Gauze Alginates: Sorbsan, Restore, Kaltostat , Algicell Hydrofibers Aquacel, Aquacel AG, Maxorb AG Iodosorb: Mixed with Curasol Collagen: Fibracol, Promogran Prisma, Medifil Heavy Wound Drainage Infected Wound Iodosorb Alginates: Sorbsan, Restore, Kaltostat , Algicell Hydrofibers Aquacel, Aquacel AG, Maxorb AG Foam: Allevyn, Mepilex, Mepilex Lite Collagen: Fibracol, Promogran Prisma, Medifil Iodosorb Gauze with: NS, DABS, Acetic Acid, Dakin’s Change 3-4x/ day Silver Dressings: Aquacel AG, Prisma, Silverlon, Acticoat 7, Maxorb AG WOUND FILLERS Absorbent Moist healing environment Facilitates debridement Eliminates dead space Softens eschar and liquefies slough Easy to apply WOUND FILLERS Difficult to remove Not for dry eschar or light exudate (unless goal is to desiccate the ulcer bed) Can dehydrate wound bed Requires secondary dressing Not for deep or sinus tracting wounds Take home points Early identification of peripheral arterial disease Early intervention of peripheral arterial disease Proactively protect from injury Do not hydrate/macerate eschar (dead tissue) Do not debride if moderate to severe ischemia Treatment Options Identify etiology of wound and treat appropriately Create proper wound environment for healing Current therapies available Goals of the patient Insurance rules Atypical Arterial Disease Thromboangiitis Obliterans/Buerger’s disease Nonatherosclerotic, segmental, inflammatory (vasculitis), occlusive disease that affects the small & medium arteries and veins and is strongly associated with tobacco exposure (cigarettes, cannabis, tobacco chewing) Demographics: Young smokers 15 - 45 years old Male (9:1) Presentation: Foot claudication Rest pain / Digital ulcers Superficial phlebitis Upper extremity involvement Variable Buerger’s Disease Premature Atherosclerosis Upper Extremity Yes No Foot Claudication Yes No Phlebitis Yes No Tobacco Yes Yes Age < 40 > 40 Treatment Smoking cessation Digit protection Arterial pumping Non-surgical candidate Wound care Auto amputation