Peripheral Arterial Disease
Education and ABI Training
for Vascular Nurses
Presented by
The Society for Vascular Nursing
Comprehensive In-Service Lecture Kit
Supported by an educational grant from
Bristol-Myers Squibb/Sanofi Partnership
PERIPHERAL ARTERIAL DISEASE
Education and ABI Training for
Vascular Nurses
A Train the Trainer Program
The Ankle Brachial Index:
The Key to Early Detection
and Management of
Peripheral Arterial Disease
Acknowledgements
Course Development
– ABI Registry Task Force
Diane Treat-Jacobson, Ph.D., R.N.
Carolyn Robinson MSN, RN, CNP,CVN
Marge Lovell RN, CCRC, CVN, BEd
Patricia Lewis, MS, FNP, CVN
M. Kate Schmidt, BSN, RN, CVN
Contact Information
Society for Vascular Nursing
203 Washington St., PMB 311
Salem, MA 01970
888-536-4786; 978-744-5005; Fax: 978-744-5029
Peripheral Arterial Disease
and Claudication
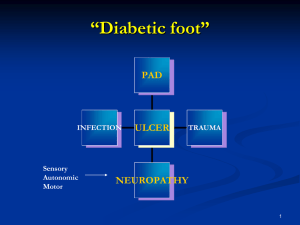
Peripheral Arterial Disease (PAD)
A disorder caused by atherosclerosis that
limits blood flow to the limbs
Claudication
A symptom of PAD characterized by pain,
aching, or fatigue in working skeletal
muscles. Claudication arises when there is
insufficient blood flow to meet the metabolic
demands in leg muscles of ambulating
patients
New PAD Guidelines
Enhanced quality of patient care
Increased recognition of the importance of
atherosclerotic lower extremity PAD:
– Prevalence
– Cardiovascular risk
– Quality of life
Improved ability to detect and treat renal artery
disease
Improved ability to detect and treat AAA
The evidence base has become increasingly robust,
so that a data-driven care guideline is now possible
Defining a Population “At Risk” for
Lower Extremity PAD
Age less than 50 years with diabetes, and one
additional risk factor (e.g., smoking, dyslipidemia,
hypertension, or hyperhomocysteinemia)
Age 50 to 69 years and history of smoking or diabetes
Age 70 years and older
Leg symptoms with exertion (suggestive of
claudication) or ischemic rest pain
Abnormal lower extremity pulse examination
Known atherosclerotic coronary, carotid, or renal
artery disease
Relative Prevalence of Peripheral
Arterial Disease
Age
(years)
Population
(millions)
PAD
(millions)
Claudication
(millions)
40-59
68.9
2.1
0.9
60-69
19.8
1.6
0.8
70
24.8
4.7
113.5
8.4
2.5
4.2
Criqui MH et al. N Engl J Med. 1992;326:381-6.
Hiatt W et al. Circulation. 1995;91:1472-9.
Porter J. Mod Med. 1987;55:66-75.
US Census Data, 1998 estimates.
Web address www.census.gov/population/estimates/nation/infile2-1.txt
Systemic Manifestations of
Atherosclerosis
• TIA
• Ischemic stroke
• Myocardial Infarction
• Unstable angina pectoris
• Renovascular hypertension
• Erectile dysfunction
• Claudication
• Critical limb ischemia, rest pain,
gangrene, amputation
Prevalence of PAD
NHANES1
Aged >40 years
San
4.3%
Diego2
11.7%
Mean age 66 years
NHANES1
14.5%
Aged 70 years
Rotterdam3
19.1%
Aged >55 years
Diehm4
In a primary care
population defined by age
and common risk factors,
the prevalence of PAD was
approximately one in three
patients
19.8%
Aged 65 years
PARTNERS5
29%
Aged >70 years, or 50–69 years with a history diabetes or smoking
0%
5%
10%
15%
20%
25%
30%
NHANES=National Health and Nutrition Examination Study;
PARTNERS=PAD Awareness, Risk, and Treatment: New Resources for Survival [program].
1. Selvin E, Erlinger TP. Circulation. 2004;110:738-743.
2. Criqui MH et al. Circulation. 1985;71:510-515.
3. Diehm C et al. Atherosclerosis. 2004;172:95-105.
4. Meijer WT et al. Arterioscler Thromb Vasc Biol. 1998;18:185-192.
5. Hirsch AT et al. JAMA. 2001;286:1317-1324.
35%
Prevalence of PAD Increases with Age
Rotterdam Study (ABI <0.9)1
San Diego Study (PAD by noninvasive tests)2
Patients With P.A.D. (%)
60
50
40
30
20
10
0
55-59
60-64
65-69
70-74
75-79
80-84
85-89
Age Group,
years
ABI=ankle-brachial index
1. Meijer WT, et al. Arterioscler Thromb Vasc Biol. 1998;18:185-192.
2. Criqui MH, et al. Circulation. 1985;71:510-515.
Gender Differences in the
Prevalence of PAD
18
Prevalence (%)
16
14
12
6880 Consecutive Patients (61% Female)
in 344 Primary Care Offices
Women
Men
10
8
6
4
2
0
<70
70–74
75–79
Age (years)
Diehm C. Atherosclerosis. 2004;172:95-105.
80–74
>85
Diabetes Increases Risk of PAD
Prevalence of PAD (%)
25
22.4*
19.9*
20
15
12.5
10
5
0
Normal glucose
tolerance
Impaired glucose
tolerance
Diabetes
Impaired Glucose Tolerance was defined as oral glucose tolerance test value ≥140 mg/dL but <200 mg/dL.
*P.05 vs normal glucose tolerance.
Reprinted with permission from Lee AJ et al. Br J Haematol. 1999;105:648-654. www.blackwell-synergy.com
Ethnicity and PAD:
The San Diego Population Study
% PAD
10
9
8
7
6
5
4
3
2
1
0
NHW
Black Hispanic Asian
NHW = Non-hispanic white
Criqui et al. Circulation. 2005: 112: 2703-2707.
Risk Factors for PAD
Reduced Increased
Smoking
Diabetes
Hypertension
Hypercholesterolemia
Hyperhomocysteinemia
C-Reactive Protein
Relative Risk
0
1
2
3
4
5
6
Hirsch AT, et al. J Am Coll Cardiol. 2006;47:e1-e192.
Pathogenesis of
Progressive Atherosclerosis
Risk of Ischemic Events
Previous MI
– 5-7 times more likely to have another MI
– 3-4 times more likely to have a stroke
Previous stroke
– 9 times more likely to have another stroke
– 2-3 times more likely to have an MI
PAD
– 4 times more likely to have an MI
– 2-3 times more likely to have stroke
Long-term Survival in Patients With PAD
100
Survival (%)
Normal subjects
75
Asymptomatic PAD
50
Symptomatic PAD
Severe symptomatic PAD
25
0
2
4
6
8
10
12
Year
Criqui MH et al. N Engl J Med. 1992;326:381-386. Copyright © 1992 Massachusetts Medical Society. All rights reserved.
Contemporary PAD
Rates of Myocardial Infarction and Death
3649 subjects (average age 64 yrs) followed up for 7.2 years
50
40
%
30
20
10
0
MI
No PAD
Asymptomatic PAD
Death
Symptomatic PAD
Hooi JD, et al. J Clin Epid. 2004;57:294–300.
Association Between ABI and
All-Cause Mortality*
Risk increases at
ABI values below
1.0 and above 1.3
Total mortality (%)
80
70
N=5748
60
50
40
30
20
10
0
<0.61
(n=156)
0.61-0.70 0.71-0.80 0.81-0.90 0.91-1.00 1.01-1.10 1.11-1.20 1.21-1.30 1.31-1.40
(n=141)
(n=186)
(n=310)
(n=709)
(n=1750) (n=1578)
Baseline ABI
Age range=mid- to late-50s; *Median duration of follow-up was 11.1 (0.1–12) years.
Adapted from O’Hare AM et al. Circulation. 2006;113:388-393.
(n= 696)
(n=156)
>1.40
(n=66)
A Risk Factor “Report Card” for all
Individuals with Atherosclerosis
Tobacco smoking
Complete, immediate
cessation
Hypertension
BP less than 130/85
mmHg
Diabetes
Hb A1C <7.0
Dyslipidemia
LDL Cholesterol less than
100 mg/dl
Raise HDL-c
Lower Triglycerides
Inactivity
Follow activity guidelines
Antiplatelet therapy (like aspirin or Plavix) is:
Mandatory
Pathway of Disability in
Intermittent Claudication
PAD
Reduced
muscle
strength
Poor
walking
ability
and IC
Disability
Denervation, muscle-fiber
atrophy, decreased type
II fibers, decreased
oxidative metabolism
Cycle of deconditioning: decreased
HDL, poorer glycemic control,
poorer BP control
Adapted from McDermott M. Am J Med. 1999;CE (I):18-24.
Impact of PAD on Quality of Life
PAD Diagnosis and Management
Symptom Experience
Limitation in Physical Functioning
Limitation in Social Functioning
Compromise of Self
Uncertainty
Adaptation
SF-36 Scores in Health and Disease
Intermittent
claudication
CHF
No. of people
30
Chronic
lung
disease
34 36 38
40
Average
adult
50
Physical Component Summary Score
Average
well adult
55
Location of Obstruction
Influences Symptoms
Obstruction in:
Aorta or
iliac artery
Claudication in:
Buttock, hip,
thigh
Femoral artery
or branches
Thigh,
calf
Popliteal
artery
Calf, ankle,
foot
Claudication: A Symptom of
Peripheral Arterial Disease
Exertional aching pain, cramping, tightness,
fatigue
Occurs in muscle groups, not joints (buttocks,
hips, legs, calves)
Reproducible from one day to the next on
similar terrain
Resolves completely with rest
Occurs again at the same distance once
activity has been resumed
Symptoms in PAD
Patients with
PAD
Symptomatic
PAD
~39%1
Typical Symptoms
(Intermittent
Claudication)
~9%
1.
2.
Asymptomatic
PAD
~61%1
Atypical
Symptoms
~91%
American Heart Association. Heart Disease and Stroke Statistics—2005 Update. 2005.
Hirsch AT, et al. JAMA. 2001;286:1317-1324.
Clinical Assessment of
Peripheral Arterial Disease
Components of Clinical
Assessment
Complete history
– Risk factor assessment
– Activity assessment
Review of medications
Physical examination
– Inspection of lower extremities
– Pulse exam
Questions for Patients
Do you develop discomfort in your legs
when you walk?
– Cramping, aching, fatigue
Do you get this pain when you are sitting
standing, or lying?
Do symptoms only start when you walk?
Does the discomfort always occur at about
the same distance?
Do symptoms resolve once you stop
walking?
PAD Pulse Evaluation
Right
Left
Femoral
Popliteal
Dorsalis pedis
Posterior tibial
Ankle–brachial
index
Note: 0-4 scale, where 0 = absent, 2 = Diminished, 4 = Normal Limits
The Ankle-Brachial Index (ABI)
The first diagnostic assessment that
should be done to evaluate a patient for
PAD after a pulse exam in the presence of
risk factors or if claudication is suspected.
Inexpensive, accurate and can be done in
the primary care setting
The ABI is 95% sensitive and 99% specific
for PAD
Predicts limb survival, potential for wound
healing, and mortality
The Ankle-Brachial Index (ABI)
Indicated
– In the absence of palpable pulses,
or if pulses are diminished
– In the presence or suspicion of
claudication, foot pain at rest, or a
non-healing foot ulcer
– Age greater than 70 years of age,
>50 years with risk factors
(diabetes, smoking)
Concept of ABI
The systolic blood pressure in the leg should be
approximately the same as the systolic blood pressure
in the arm.
Therefore, the
ratio of systolic
blood pressure in
the leg vs the arm
should be
approximately 1
or slightly higher.
Leg pressure
÷
Arm pressure
ABI has been found to be 95% sensitive and 99%
specific for angiographically diagnosed PAD.
Adapted from Weitz JI, et al. Circulation. 1996;94:3026-3049.
≈1
Understanding the ABI
Performed with patient resting in
supine position
All pressures are measured with a
arterial Doppler and appropriately
sized blood pressure cuff
Both brachial pressures are measured
Ankle pressures are measured using
the posterior tibial and/or dorsalis
pedis arteries
Measuring the Ankle-Brachial Index (ABI)
Step 1: Gather Equipment Needed
Equipment needed:
1. Blood Pressure
Cuff
2. Hand-held 5-10
MHz Doppler
probe
3. Ultrasound Gel
American Diabetes Association. Diabetes Care 2003: 26; 3333–3341.
Measuring the Ankle-Brachial Index
(ABI)
Step 2: Position the Patient
Place patient
in supine
position for
5 – 10 minutes
minutes
American Diabetes Association. Diabetes Care 2003: 26; 3333–3341.
Measuring the Ankle-Brachial Index (ABI)
Step 3: Measure the Brachial Blood
Pressure
1. Place the blood pressure cuff
on the arm above the elbow.
2. Apply gel to the skin surface.
3. Place the Doppler probe over
the brachial pulse
4. Inflate the cuff to approx. 20
mm/hg above the point where
systolic sounds are no longer
heard.
5. Deflate the cuff slowly until
the arterial signal returns
(systolic pressure)
6. Repeat in the other arm
American Diabetes Association. Diabetes Care 2003: 26; 3333–3341.
Measuring the Ankle-Brachial Index
(ABI)
Step 4: Position the Cuff Above the Ankle
Place blood
pressure cuff
just above the
ankle of one leg,
apply gel over
the area of the
dorsalis pedis
artery
Dormandy JA et al. J Vasc Surg. 2000;31:S1-S296.
Measuring the Ankle-Brachial Index (ABI)
Step 5: Measure the Pressure in the Dorsalis
Pedis Artery
1. Place Doppler probe
over the dorsalis
pedis artery; inflate
the cuff
2. Deflate the cuff; when
the return of blood
flow is detected,
record this as the
systolic pressure of
the DP artery of that
leg
Dormandy JA et al. J Vasc Surg. 2000;31:S1-S296.
Measuring the Ankle-Brachial Index (ABI)
Step 6: Measure the Pressure in the
Posterior Tibial Artery
1. Place gel and
Doppler probe over
the posterior tibial
artery (below the
cuff)
2. Measure the
pressure, record as
posterior tibial
pressure for that
leg
Dormandy JA et al. J Vasc Surg. 2000;31:S1-S296.
Measuring the Ankle-Brachial Index (ABI)
Step 7: Repeat the Process in the
Opposite Leg
Repeat the same
process in the
other leg and
record the
pressures of the
dorsalis pedis
and posterior
tibial arteries
Dormandy JA et al. J Vasc Surg. 2000;31:S1-S296.
Calculating the ABI
Right Leg ABI
Left Leg ABI
Higher right-ankle
pressure
(DP or PT pulse)
=
Higher arm pressure
(of either arm)
Higher left-ankle pressure
(DP or PT pulse)
=
Higher arm pressure
(of either arm)
ABI Interpretation
≤ 0.90 is diagnostic of peripheral arterial
disease
Hiatt WR. N Engl J Med. 2001;344:1608-1621.
Calculating the ABI
Example Calculation
Right Leg ABI
=
Left Leg ABI
60 mm Hg
120 mm Hg
Hiatt WR. N Engl J Med. 2001;344:1608-1621.
66 mm Hg
=
120 mm Hg
Calculating the ABI
Example Calculation
Right Leg ABI
60 mm Hg
Left Leg ABI
66 mm Hg
= 0.50
120 mm Hg
120 mm Hg
= 0.55
ABI Interpretation
≤ 0.90 is diagnostic of peripheral arterial
disease
Hiatt WR. N Engl J Med. 2001;344:1608-1621.
ABI Limitations
Possible false negatives in patients with
noncompressible arteries, such as some
diabetics and elderly individuals
Insensitive to very mild occlusive disease
and iliac occlusive disease
Not well correlated with functional ability
and should be considered in conjunction
with activity history or questionnaires
Interpreting the
Ankle–Brachial Index
ABI
0.90–1.30
Interpretation
Normal
0.70–0.89
Mild
0.40–0.69
Moderate
0.40
Severe
>1.30
Noncompressible
vessels
Adapted from Hirsch AT. Family Practice Recertification. 2000;22:6-12.
Referring to the Vascular Lab
Caveats for referral to vascular lab
• Assessment of the location and severity is
desired
• Patients with poorly compressible vessels
• Normal ABI where there is high suspicion of
PAD
Vascular Lab Evaluation
• Segmental pressures
• Pulse volume recordings
• Treadmill
PAD Diagnosis
Indications for Referral
for Vascular Specialty Care
Lifestyle-disabling
claudication (refractory to
exercise or pharmacotherapy)
Rest pain
Tissue loss
Severity
of
ischemia
Summary
PAD is a common atherosclerotic disease
associated with risk of cardiovascular ischemic
events and significant functional disability
PAD can be effectively assessed in the primary
care setting by primary care nurses
The ankle brachial index is an effective and
efficient measurement tool for diagnosis of PAD
Early detection of PAD allows for appropriate
disease management and decreased likelihood of
ischemic events and disease progression
The Graying of U.S. Society
Seniors 12.4 percent of the
population
Baby boomers will number 75 million
2030
– 20 percent will be over age 65
– 1/2 population > age 40
Nurse Competence in Aging
Imperatives
Moving to an aging society
85+ population > 8.9 million in 2030
Older adults
– Utilize 50% of hospital days
– 45% of the direct care
– primary patient population of most
specialty nurses.
Geriatric preparation significantly
improve health care to older adults.
Classifying the Elderly
ages 65 to 74 - the young old
ages 75 to 84 - the middle old
ages 85 and older - the old old
Impact of Aging
↑risk of health
↑co-morbidities
↑ disabilities
↑dementia
↑seniors with chronic illness requiring
care
↓quality of life
Age Related Changes
Cardiac
Pulmonary
Renal
Gastrointestinal
CNS
Integument
Cardiac Function
Coronary artery blood flow
– decreases 35% between ages 20 and 60.
Cardiac output decreases
Systolic and diastolic murmurs
There is a decrease in cardiac
responsiveness rate with exercise.
Cardiovascular Function and
Aging
Central and peripheral circulation decreases
Aerobic capacity decreases about 1% per
year
Maximum heart rate decreases about 1 beat
per year
Maximum stroke volume decreases
Maximum cardiac output decreases
Peripheral blood flow decreases
Physiological Changes to the
Body with Aging
Heart muscle
– Contractile strength and efficiency decreases
– Left ventricular wall thickens
Heart valves
– fibrotic and sclerotic
SA node and AV tracts
– Infiltrated by fibrous tissue.
Aortic and mitral valves
– Calcify
Changes in Blood Vessels
Veins and arteries
– dilate and stretch
– decreased strength and elasticity.
Peripheral arteries
– Tortuous
– Less resilient.
Aorta and large arteries
– stiffen
Aorta
– may lengthen and become tortuous.
Blood Pressure Changes
Systolic blood pressure
– May rise disproportionately higher than
diastolic.
Changes in the cardiovascular system
– Direct effects on other organs.
Hypertension
– Atherosclerotic changes in blood vessels
– May result in the loss of vision, renal
Strength Changes With Aging
Maximal strength decreases
Muscle mass decreases
Total number and size of muscle
fibers decreases
Nervous system response slows
Exercise and the Elderly
1996 report 30% of the elderly exercise
regularly.
Results in decreased risk for a number of
chronic and debilitating illnesses.
US Department of Health and Human Services
Assess
– Motivation.
– Level of activity that a person is capable of
doing,
– Help him/ her to understand how to change
Health Care for the Elderly
Include
– health promotion,
– disease prevention,
– health maintenance
Anatomical and physiological changes
– cardiovascular
– Genitourinary
– Neurological
– musculoskeletal
respiratory
endocrine
skin