Új, Nem-Invazív Módszer és Műszer Endothél Diszfunkció
advertisement
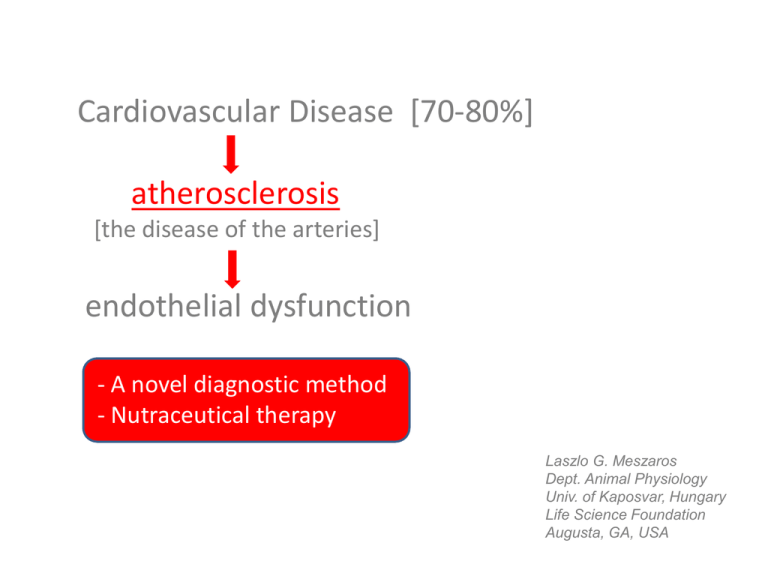
Cardiovascular Disease [70-80%] atherosclerosis [the disease of the arteries] endothelial dysfunction - A novel diagnostic method - Nutraceutical therapy Laszlo G. Meszaros Dept. Animal Physiology Univ. of Kaposvar, Hungary Life Science Foundation Augusta, GA, USA “You’re as old as your arteries…” Some Cardiovascular Disease (CVD) Statistics Atherosclerosis (AS) Some more AS statistics – WHO 2008 The most “deadliest” risk factors all relate to AS… “As old as your arteries…” Non-optimal circulation: in essence, every organ, tissue affected AS risk factors and markers AHA - 2012 LDL ↑ Diet & Physical Inactivity – 74% (ApoB/ApoA ↑ Lp-PLA2 ↑) Smoking Alcohol Genetics (Air) Pollution HDL ↓ CRP ↑ Metabolic disease BPsys ↑ Obesity ↑ Homo-Cystein ↑ Diabetes Frequency AS is a degenerative (chronic) disease Putative causes: error accumulation epigenetics Age Anatomy of arteries Function of arterial cells – Vasodilation 1 Endothelial cell layer (largest endocrine organ): • regulates smooth muscle constriction/dilation • thereby, sets vessel diameter (and?) • (permeability, blood cell – vessel wall interact.) Vasodilators: • synth.: EDHF (C-natriuretic peptide?), NO • mediates: shear stress, bradykinin, ANP*, VIP*, prostagladines, prostacyclin… Vasoconstrictors: • synthesize: endothelins • mediates: adrenerg-, muscarinic agonists, vasopressin, thromboxane, hypox. *Atrial Natriuretic Peptide, Vasoactive Intestinal Peptide Function of arterial cells – Vasodilation 2 AS ̶ initiation and progression of the disease AS Stages: 1. Endothelial dysfunction (ED) – NO (aging, free radicals, ADMA) (Flow-mediated dilation ) endothelial activation (early inflammation?) LDL-cholesterol oxidation (free radicals?) – fatty streaks NON-LOCALIZED Years 2. Recruitment of immune cells, collagen synthesis, calcification, endothelial permeability, apoptosis, SM proliferation – plaques LOCALIZED and/or NON-LOCALIZED 3. Thrombocyte activation, thrombus formation mosly LOCALIZED Techniques to assess arterial health must consider LOCALITY/NON-LOCALITY. Vasography: Flow-Mediated Dilation Another Way method to assess endothelial function in the arteries HU (P1000657) and US (US 61483768) patents Techniques to assess arterial health I. Sorting them out… - invasive vs. non-invasive - early vs. late - expensive vs. less expensive - usable for screening vs. … - locality vs. non-locality - simple to use vs. …(requirement of clinical setting) - grading, staging Costly, clinical setting required: Angiography – invasive, local Stress test (ECG) – indirect Calcium “scoring” (CT) – late stage Ultrasound – seems user-dependent, local? Intravascular ultrasound – invasive, local (advantage?) Techniques to assess arterial health II. Pulse Wave Velocity (much less costly) - narrower the artery faster the pulse travels (Bernoulli) - detection of pulse appearance at two locations with different distances from the heart Arterial Stiffness (m/s) Localized or not? No, it is not! Aorta-Femoral For instance, very good correlation between B-A PWV and coronary calcification: Liu, C-S.: Arterial Stiffness is Highly Correlated with Coronary Atherosclerosis, J. Athero. Thromb. 18:online (2011) Blacher, J.: Impact of Aortic Stiffness on Survival…, Circulation 99:2434 (1999) Techniques to assess arterial health III. FMD (Flow-Mediated Dilation with ultrasound) – the first sign, but… Localized or not? No, it is most likely not! Bots, ML.et al.: Assessment of flow-mediated vasodilatation (FMD) of the brachial artery, Eur. Heart J., 26:363 (2004) Techniques to assess arterial health IV. Pulse Contour Analysis (PCA) – less costly Millaseau, SC. et al.: Determination of age-related increases in large artery stiffness by digital pulse contour analysis, Clin. Sci., 103:371 (2002) Aix SphygmoCor Arteriograf ArcSolver CVprofiler… SI and RI: Pulse Tracer BioClip According to the theory behind them: evolution is STUPID. Wang, K-L. et al.: Wave Reflection and Arterial Stiffness…, Hypertension, 55:799 (2010) Some problems with PCA 1. The model: “wave reflection” 2. Math: Without curve fitting? Pulse contour types Vasography = FMD differently and better Reminder: shear stress ↑, then Ca ↑, which makes NO ↑ resulting in vasodilation. Vasography = FMD differently and better Methods: - Pressure pulse (PP) recorded by using piezoelectric sensor (UFI, USA) - Volume pulse recorded near-infrared plethysmographic sensor (Norelco, USA) SIMULTANEOUSLY Data fed into a 12 bit A/D converter Pulses averaged, then normalized in length and height Max. rate of rise (rsys) computed from normalized records by taking the time-derivative Significance by ANOVA Vasography = FMD differently and better Development of VP is delayed (relative to PP) The delay is larger, max. rate is slower in the elderly Vasography = FMD differently and better NG = nitroglycerin, an NO donor The rate difference between PP and VP decreases after NG in the elderly (Max. rate in PP is not altered by NG) Thus, max. rate in VP measures endothelial function (just like FMD with ultrasound, but without the snags) Vasography = FMD differently and better A: R = 0.783; P < 0.001 B: Difference is significant (P < 0.05) Vasography = FMD differently and better Tone + Pulsation (PWV) vs. Pulsation (rsys) The exponential curve is NOT a surprise Vasography = Pulsating FMD (PFMD) Thanks for listening…