Sinusitis
advertisement

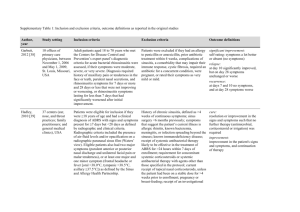
Objectives: i. ii. iii. iv. v. vi. List the possible etiologies of sinus infections Compare and contrast the symptoms found in bacterial vs viral sinusitis Describe the treatment of viral sinusitis Describe the treatment of bacterial sinusitis Describe the complications of sinus infections and indications for referral Describe the complications of sinus infections and indications for referral USC Case #4: Sinusitis Chief Complaint (CC): cold symptoms, nasal congestion, some sinus pain History of Present Illness (HPI) A 24 year old medical student, presents to the office in August complaining of ongoing upper respiratory cold symptoms for almost 2 weeks now. She has used over-the-counter medication without significant benefit. She has also taken a few antibiotic pills her roommate had laying around last week. This also provided little benefit. She lists her specific symptoms as runny nose, worsening nasal congestion, mildly productive cough, sore throat, headache, subjective fever and chills, decreased appetite, and overall malaise. You begin, as any good medical student would do, to form a differential diagnosis. What are a few of the diagnosis on your list so far? 1. Rhinitis, viral 2. 3. 4. 5. 6. Sinusitis, viral Sinusitis, bacterial Pneumonia Influenza Meningitis What other important historical points would you want to elicit? Questions regarding dental pain, purulent nasal discharge, hemoptysis, epistaxis, chest pain, and unilateral facial pain or pressure worse with bending over should not be forgotten. Specific presence of neck pain, visual disturbance, periorbital edema, and mental status changes should be addressed. One should consider immediate referral if these findings are present. This information can help eliminate more serious conditions from your differential. Specific antibiotic use should also be identified. Periorbital Cellulitis Review of Systems (ROS) HEENT: Respiratory: CV: GI: GU: Skin: General: Denies severe headache, diplopia or visual loss, mental status change, dental pain, neck pain, epistaxis Reports purulent nasal discharge and right-sided facial pain Denies hemoptysis, purulent sputum production, dyspnea Denies chest pain Denies abdominal pain, nausea, vomiting, and diarrhea Denies change in urinary pattern or hematuria Denies rash Denies weight loss or night sweats Reports mild loss of appetite since illness began What is the significance of questioning for chest pain? Viral myocarditis often begins with flu like illness. This can be a life threatening condition and should be treated with caution. Signs and symptoms include chest pain or discomfort, flu like symptoms, fever, dyspnea, fatigue, tachycardia, peripheral edema, friction rub, S3/S4 gallop, pulmonary crackles, and orthopnea. The complication from myocarditis is heart failure. If signs and symptoms are noted then appropriate supportive measures and diagnostic work up are warranted. What specific questions are important in regards to past medical history in this patient? Important historical data would include history of allergic rhinitis, swimming, drug and alcohol use, intranasal cocaine use, sick contacts, smoking history, recent hospitalization, and chronic medical diseases such as asthma, diabetes, HIV, liver or renal disease, recurrent dental infections, and cystic fibrosis. History of nasal polyps, facial trauma (e.g. septal deviation), and head injury should also be obtained. These conditions predispose a person to acquire infections more readily. Also note season of year for likelihood of influenza infection. Past Medical History (PMH) Denies diabetes mellitus, asthma, allergic rhinitis, HIV, liver or renal disease, or recurrent infections Surgical History (SxH) Denies any previous surgery Family History (FH) No diabetes, heart disease, asthma, immune deficiencies, or similar symptoms. Social History (SH) Denies cocaine use. Denies IV drug use. Occasional alcohol and marijuana. Smokes 1 PPD x 6 years. Lives with family. Medical student. Heterosexual. Physical Exam (PE) Temp: 99.5 Pulse: 88 BP: 125/78 Resp: 18 Weight: 175 Height: 6’ 0” GENERAL: mild distress. Alert and oriented. Cooperative with fluent speech. HEENT: normocephalic, atraumatic. External ocular muscles intact. Pupils equal round and reactive to light. TM’s intact c clear fluid. No erythema or exudates noted. Nasal mucosa swollen and erythematous with thick yellow discharge. No polyps noted. There is right maxillary and frontal sinus tenderness to palpation. Posterior oropharynx without exudates. Mild erythema noted. NECK: supple without lymphadenopathy, thyromegaly, bruits, or mass noted. Full range of motion. CHEST: clear to auscultation bilaterally without crackles, rhonchi, or wheeze. HEART: S1, S2 without murmur, gallop, rub, or click. Regular rate of 88. ABDOMEN: soft, nontender, nondistended. No organomegaly. EXTREMITIES: pulses full and equal. Full range of motion. SKIN: No rash or erythema noted. What is your diagnosis at this point? Acute rhinosinusitis. What is the most common cause of acute sinusitis/rhinosinusitis? Viral infection accounts for nearly 98% of all acute sinus infections. Only 2% of viral infections are complicated by bacterial superinfection. One of the most important issue surrounding sinusitis is determining the exact etiology of the infection. See table below for common viral, bacterial, and fungal agents causing sinusitis. What is the natural course of rhinosinusitis? Typical viral infections last 7 to 10 days whereas ¾ of all bacterial infections resolve at one month’s time. However the accompanying morbidity and possibility of extension of infection into the skull, orbital, and meninges warrants antibiotic intervention. What benefit is transillumination of the sinuses? Transillumination can only be performed for the frontal and maxillary sinuses. Additionally, it cannot differentiate between viral or bacterial sinusitis and is very operator dependant. It has little clinical value and poor predictive information. What role does radiological imaging play in the diagnosis of sinusitis? Imaging is not recommended for the usual community acquired sinusitis, unless intracranial or orbital extension is suspected. CT is normally reserved for those who have failed multiple antibiotic courses and surgery is a consideration. CT also provides better sensitivity and specificity than plain x-ray. Again, these diagnostic tests cannot differentiate between viral and bacterial causation. Additionally, CT occasionally will result in false positives. In one study, 27 of 31 patients with simple common colds had abnormal sinus CT films. (see image below) Arrows indicate inflamed mucosal lining of maxillary sinuses What is the criterion for diagnosing bacterial sinusitis? Studies have been done using clinical findings to differentiate viral vs. bacterial infection, however they used imperfect diagnostic controls. The definitive diagnostic test for sinusitis etiology is sinus aspirate culture, which have not been implemented in comparison studies. Up to Date has published three organizational guideline comparisons which comment on duration of symptoms, fever, sinus pain, and purulent nasal discharge as criteria for diagnosis. (See below) What is the accepted treatment for acute viral sinusitis? Treatment of rhinoviral infections should be aimed at controlling the inflammation and facilitating drainage. 1st generation antihistamines help decrease sneezing, rhinorrhea, and nasal mucous thickness. Expectorants can also aid in thinning secretions. Osteopathic manipulation such as facial effleurage and myofascial release of the thoracic outlet can facilitate improved drainage and produce little side effects. NSAID’s can also benefit by reducing malaise and headache. Decongestants and cough suppressants can be added but should not be used for prolonged periods. What about bacterial sinusitis? There are no good randomized placebo controlled studies for treatment of bacterial sinusitis using pre and post treatment sinus aspirate cultures as standards for cure. However, it is felt that antibiotic therapy reduces the degree of symptoms and duration of the illness based on clinical and radiographic evidence. Antibiotic resistance to S. pneumoniae, H. influenza, and M. catarrhalis is a growing concern mainly due to use of antibiotics for viral infections. Cephalexin, clindamycin, and macrolides generally do not provide adequate coverage or they are associated with resistance in the community. Therefore, first line therapy should include narrow spectrum antibiotics such as amoxicillin, trimethoprim-sulfamethoxazole, and doxycycline. One could also consider no antibiotic intervention based on the self limited nature and very low frequency of complications mentioned earlier. If the patient does not improve or worsens, other agents such as levofloxacin, amoxicillin-clavulanate, or a 3rd generation cephalosporin could be implemented. Typical course would be 7 to 10 days of treatment. The viral sinusitis treatment plan would also be prescribed in addition to antibiotics. There is some data supporting chronic infections responding favorably to intranasal steroids. When should a primary care physician refer their patient to a specialist (ENT)? If the patient were to fail multiple antibiotic courses or they presented with significant symptoms mentioned previously, then referral would be in order. One should begin thinking about referral if CT scan is being ordered. An otolaryngologist can perform sinus aspirate cultures for specific antibiotic resistance, nasal endoscopy, sinus washings, or surgery to correct any anatomical predisposing conditions. Facial Cellulitis Algorithm for the antibiotic management of acute bacterial rhinosinusitis Algorithm for the management of acute bacterial rhinosinusitis. CT: computed tomography; MRI: magnetic resonance imaging. * In patients with uncomplicated ABRS with good follow-up, observation without antibiotics is an option. Antibiotics should be started if there is no improvement in symptoms. Guidelines differ as to when to start antibiotics if there is no improvement in symptoms. REFERENCE Acute sinusitis and rhinosinusitis. 2015 UpToDate®. uptodate.com