Sniffing out the problem
advertisement
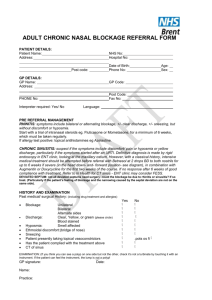
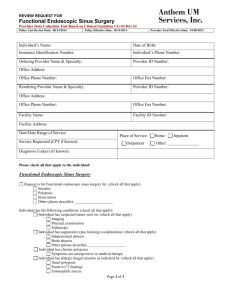
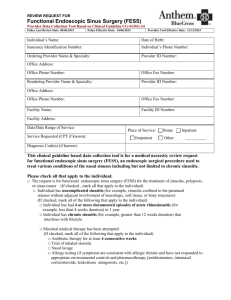
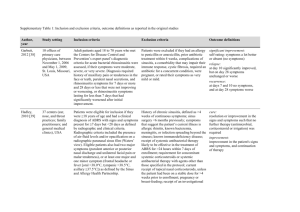
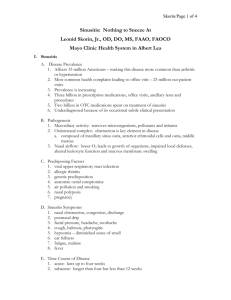
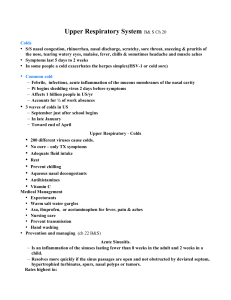
Sniffing out the problem Jonathan Hern Commissioning Guide for Chronic Rhinosinusitis • ENTUK and RCS • Based on European position paper on sinusitis • Guidance for primary and secondary care treatment of sinusitis Introduction • • • • • • Acute sinusitis Duration < 12 weeks Aetiology usually infective Chronic sinusitis Duration > 12 weeks Aetiology multifactorial including inflammatory, infective and obstructive (sinus ventilation and drainage) • 10% prevalence in UK Acute sinusitis • History • Presence of 2 or more symptoms for < 12 weeks • Either nasal obstruction and/or discharge • Facial pain/pressure • Reduced sense of smell Acute sinusitis Acute sinusitis Paediatric acute sinusitis Chronic Sinusitis in primary care • • • • • • History Presence of 2 or more symptoms for > 12 weeks Either nasal obstruction and/or discharge Facial pain/pressure Reduced sense of smell Subcategorised by presence or absence of nasal polyps • CRSwNP or CRSsNP • Unilateral symptoms raise suspicion of neoplasia Primary care • • • • • • • Examination Anterior rhinoscopy Otoscope or endoscope Discharge Inflammation Nasal polyps Turbinate hypertrophy Assessment of severity • 10cm Visual analogue scale • Mild (VAS 0 -3) • Moderate/severe (VAS>3) Allergic rhinitis • • • • • Nasal itching Sneezing Rhinorrhoea Epiphora Asthma (assess control) Red flags • • • • • • • • • Unilateral symptoms Cacosmia Epistaxis/crusting Diplopia Reduced visual acuity Globe displacement Periorbital oedema Severe frontal headache Neurological signs Primary care • Treatment • Nasal douching • Intranasal corticosteroids (mometasone or fluticasone) • Bilateral nasal polyps visible on AR Prednisolone EC 30mg OD 7 days with topical steroid drops (fluticasone or betamethasone) Options not advised in primary care in Chronic Sinusitis • Plain x-rays • Oral antibiotics Reassess symptom control after 3 months • Mild symptoms (VAS 0 -3) continue with medical treatment • Moderate/severe (VAS >3) assess treatment compliance and technique and refer to secondary care if not improving Treatment of chronic sinusitis in primary care Secondary care • History • Reassess history and consider diagnosis and treatment of co-morbidity • Allergy ASA triad • Systemic condition (vasculitides, ChurgStrauss, sarcoidosis) • Ciliary dyskinesia Secondary care • • • • • Examination Nasal endoscopy Purulent middle meatal discharge (swab) Polyps Middle meatal oedema SNOT 22 • Disease specific patient related outcome measure Secondary care • CT scanning • Uncertainty from nasal endoscopy (2 out of 3 rule) • Neoplasia suspected • Complications of CRS (orbital/neurological) • Allergy testing SPT or RAST and IgE Secondary care • Continue nasal saline irrigation • CRSwNP • Prednisolone, steroid drops/spray, consider Doxycycline 100mg OD 3 weeks • CRSsNP • Steroid spray, consider 4-6 weeks of macrolide antibiotic (most likely effective if IgE levels not elevated; avoid clarithromycin with statins in patients with IHD) Treatment of CRSsNP Treatment of CRSwNP Surgery • • • • Endoscopic sinus surgery Balloon sinuplasty Ethmoid or frontal stratus CT mandatory before surgery. CT score <4 alternative diagnosis should be considered • Many patients likely to require long term maintenance therapy with saline irrigation and topical steroids Variation in treatment Conclusion • • • • Primary and Secondary Care Pathways Consider earlier referral Early surgery Long term medical maintenance therapy