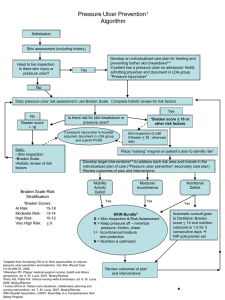
AAWC Pressure Ulcer Guideline Algorithm Presentation 8.13
advertisement

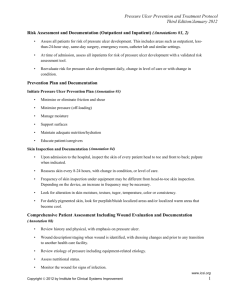
AAWC Pressure Ulcer Guideline Content Validated, Evidence Based “Guideline of Pressure Ulcer Guidelines” Using the AAWC Pressure Ulcer (PU) Guidelines to Manage Pressure Ulcers • 3 Steps to manage a PU patient: – Assess and document patient, skin & PU – Prevent PU with care plan focused on reducing risk – Treat patient and PU to heal and prevent recurrence • For guideline details, references, implementation tools, patient brochure and evidence please see: http://aawconline.org/professional-resources/resources/ Fonts Used in This PPT and in the AAWC PU Guideline Checklist • Recommendations in bold font are – Ready to Implement : • A-level evidence support • + Content validity index (CVI)>0.75 • Recommendations in bold italics – Need more Education • Content validity index (CVI) <0.75 (Raters say not relevant to PU) • A-level evidence support • Recommendations in normal font – Need more research to be considered evidence-based , but have a CVI of at least 0.75, – i.e. 75% of independent raters or more believed this recommendation was clinically relevant for PU practice. Using the AAWC Pressure Ulcer Guidelines to Prevent/Manage Pressure Ulcers • Assess and document patient’s skin • Prevent pressure ulcers (PU) as feasible. – Focusing on those at risk of developing a PU • Treat patient and PU to heal as feasible Pressure Ulcer Management • If feasible manage with a interdisciplinary wound care team or appropriate consults as needed by the individual receiving care. Assess the Patient’s Skin • Trained staff regularly assess skin sites at risk – By 72 hours after admission or per setting protocol – Usually weekly and on change in patient status Pay special attention to more darkly pigmented skin. • Document and plan care to address skin changes. • Assess skin areas where devices may cause pressure, e.g. splints, casts, tubes as feasible. Evaluate and document patient medical/surgical history • Physical Exam – Include whole-body visual and tactile skin inspection within 72 h or protocol-specified time and regularly after admission identifying PU present on admission • • • • Psychosocial condition Environment Goals, including quality of life PU risk using clinical judgment + reliable, valid scale: – Braden, Norton, Waterlow + • Assess other validated risk factors: – Body mass index (BMI) extremes – Diabetes – Extremes of age Document Progress • Document pressure ulcer progress weekly – using reliable, valid measures, e.g. • length x width to estimate area. • Partial- or full-thickness depth assessment • Ensure formal assessments are accessible to those providing or consulting on PU care Pressure Ulcer Prevention Address all patient PU risk factors identified 1. Limited mobility, activity, cognition, sensation • Redistribute pressure every 4 hr or as indicated or feasible • Properly trained staff select and use indicated pressure redistribution devices for beds, chairs and wheelchairs that meet psychological, social, anatomic and physiologic needs for those at PU risk, if appropriate for patient. • Use patient-appropriate positioning standards of care per institution protocol. • Implement appropriate exercise program as needed/feasible • Consistently train patient and care providers on PU prevention and treatment as appropriate and feasible Pressure Ulcer Prevention Address all patient PU risk factors identified 2. Manage skin moisture: • Protect skin from excess moisture with barrier • Wick excess fluid away from skin • • Patient-appropriate incontinence plan and skin-fold management if needed and feasible Clean and gently dry skin after incontinence episodes Pressure Ulcer Prevention Address all patient PU risk factors identified 3. Nutrition, circulation, infection: • Consult(s) as needed to identify/reduce PU risk • Consistent with patient and family goals and consult advice, restore, maintain good: – Hydration – Nutrition – Circulation – Infection control Pressure Ulcer Prevention 4. Protect skin • from chemical or physical pressure or trauma – – – – Avoid friction, shear, pressure on transfers Special attention to splints, casts, tubes Avoid vigorous massage Moisturize dry skin to prevent cracking • Protect skin from excess moisture and heat – Attend to areas affected by incontinence or perspiration, and skin folds in bariatric patients Treat Patient and Pressure Ulcer (PU) To Optimize Healing as Feasible • Continue or implement appropriate measures to prevent PU • Select and use appropriate effective pressure redistribution product(s) as feasible – For use on pressure sites for individuals with a PU – To avoid positioning directly on PU when on bed , chair or wheel chair surface, e.g. use cushions Treat Patient and Pressure Ulcer (PU) To Optimize Healing • Manage local and systemic factors per institutional protocols and to meet patient and family needs and goals as feasible Nutrition Circulation Infection Other, such as neuromuscular spasticity, contractures • Cleanse PU with water or saline or non-toxic cleanser at 4-15 psi • Debride nonviable tissue autolytically surgically enzyme • Evaluate PU at each dressing change for signs and symptoms of clinical infection Treat Patient and Pressure Ulcer (PU) To Optimize Healing • Dress/treat PU to maintain a moist environment, protect PU and local skin from friction, shear, pressure, trauma, irritation and excess exudate (e.g. fiber, foam or hydrocolloid dressings) • Manage PU-related pain to meet patient needs. • Identify and address all nutrient deficiencies. • 4 weeks if there is no PU area , – Re-evaluate and improve care plan – Consider adjunct therapy such as electrical stimulation