Projector presentation title in 36-40pt. Arial
advertisement

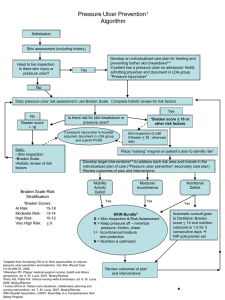
Prevention of Pressure Ulcers: Risk Assessment, Skin Assessment, and Interventions Patti Senk, BSN, RN, Doctoral Candidate Research Associate Center for Nursing Research and Practice Aurora Health Care patti.senk@aurora.org 414-219-5903 Aurora Health Care is a not-for-profit health care provider and a national leader in efforts to improve the quality of health care. Objectives • Recognize the impact of a pressure ulcer to the patient, family, and organization • Identify components of a pressure ulcer risk assessment and a comprehensive skin assessment • Describe interventions for pressure ulcer prevention • Determine your teams next steps for implementing interventions Patient’s Perspective Development of a pressure ulcer impacts an individual’s life: “The limping about is so painful; I’m happier when I am sitting out of the way. I used to be a soldier and youth worker, now I can’t do anything at all” (Hopkins et al., 2006, p. 349). . . . . Other clients describe themselves as “miserable, worthless, useless with feelings of worry, depression, inadequate and powerless” (Hopkins et al., 2006, p. 349). Patient’s Perspective Pain / discomfort “ . . .when I am sitting in my chair like now, that also hurts and if I move a little it hurts even more, so I sit very still in the chair, but still it hurts” (Hopkins et al., 2006, p. 348). Limitations with ADL’s (temporary or permanent) “I have to lie on my side for as long as I can bear [because of the ulcer], but actually my arms begin to ache after a while because, laying on your side, you can’t do anything” (Spilsbury et al., 2007, p. 499). Patient’s Perspective Emotional stress “I noticed the nurses were changing the dressings: they could hardly stand the smell of it. The smell is terrible. It comes through the whole bandage, you see, and to me it’s an embarrassment” (Spilsbury et al., 2007, p.500). Prolonged recovery time (short or long term) “Obviously, when this situation develops [pressure ulcer formation] you cannot see the end of the road” (Hopkins et al., 2006, p.349). Patient’s Perspective Increased cost . . . with the pressure ulcer the patient couldn’t work the whole day, there were frequent doctor visits, and he had to stay home to have the dressing changed; sometimes the nurse was delayed and what would only take an hour ended up taking his whole day (Gorecki et al., 2009). Increased length of stay . . . as a result of developing a pressure ulcer, the patient stayed longer in the acute care setting, and rehabilitation was limited due to restrictions from the pressure ulcer (Hopkins et al., 2006). Family Perspective Extra worry and workload “But when I’m at home as well I’m having to rely on other people to do things for me. Well, it’s not very nice for them. Because, I mean, I’m having to rely on my sister to do that and she’s got a job to go to, she’s got a son to look after, she’s got her own life to lead” (Spilsbury et al., 2007, p. 498). “. . . my wife, she was the one who did all the work and all the worry. . . . . I used equipment that pleased my daughter, not me” (Hopkins et al., 2006, p.349). Organizational Perspective Nurse quality indicator • Reflects directly on nursing practice Cost/reimbursement • Increased risk of infection, delayed healing • Exacerbation of underlying health problems (Spilsbury et al., 2007) • A single pressure ulcer may: - Increase length of stay five fold - Increase hospital charges by $2,000-11,000 • Facility acquired pressure ulcer no longer reimbursed (NPUAP-EPUAP, 2009) Why perform a pressure ulcer risk assessment? • Identifies patients who are susceptible to the development of a pressure ulcer • Allows appropriate allocation of interventions to prevent a pressure ulcer from developing Components of a Pressure Ulcer Risk Assessment • Risk assessment tool • Braden Scale for Predicting Pressure Sore Risk • Norton Pressure Ulcer Risk Assessment Scale • Comprehensive skin assessment • Risk factors to consider: • Advanced age • Skin moisture • Other factors, such as surgery time or acuity Timing of a Pressure Ulcer Risk Assessment • • • • Admission Regular intervals based on patient acuity Change in patient condition Other times Braden Scale for Predicting Pressure Sore Risk Enables nurses to collect information needed to identify patients at risk to develop a pressure ulcer • Scale consists of 6 subscales • Based on point system • Ranges from no impairment or limitation to total dependent care (Braden, 1988, accessed at http://www.bradenscale.com/) Review of Braden Scale Includes these subscales: • • • • • • Sensory Perception Moisture Activity Mobility Nutrition Friction & Shear Comprehensive Skin Assessment • Initial skin assessment provides baseline data • Ongoing assessment identifies changes from patient’s baseline • Is key to determining if the prevention interventions performed are effective Comprehensive Skin Assessment 5 Components: • Color • Temperature • Moisture • Turgor • Integrity Occiput Thoracic Vertebrae Lumbar Vertebrae Scapula Elbow Sacrum Coccyx Hip Ischium Medial Malleolus (Inner Ankle) Lateral Malleolus (Outer Ankle) Metatarsals (Toes) Calcaneus (Heel) Pressure Ulcer Prevention A pressure ulcer will not be prevented unless interventions are implemented Interventions to Prevent Pressure Ulcers • • • • • • Support Surfaces Reposition Reduce friction and shear Skin care Nutrition Education Redistribution Surface • Redistribution mattress, or overlay • Seat cushion when in chair/wheelchair • Devices for heels Do not use: • Donut devices • Water filled gloves • Sheepskin Reposition Consider: • Patient condition • Patient need • Support surface used Position • Head of bed at or below 30 degree • 30 degree side lying Heels • Elevate off bed • Heel protection devices Reduce Friction and Shear • • • • Lift/transfer equipment Trapeze Avoid positioning on medical device Avoid positioning on area with nonblanching erythema • Avoid elevated head of bed Skin Care • Cleanse gently • Skin barriers - Cream Ointment Paste Film-forming protectant • Toileting schedule • Absorbent underpad, or brief Nutrition • Screen and assess nutritional status • Goal is promote and maintain adequate intake • Consult dietician • Provide supplement Education • • • • • • Pressure ulcer risk factors How to minimize risk Skin inspection Skin care Reducing friction and shear Repositioning Skin Assessment • Continue to assess skin at regular intervals • Determines if interventions are effective Next steps: • Create a team - Interdisciplinary approach • Clearly identify risk factors • Include time frame for risk assessment and skin assessment • Communicate prevention interventions • Follow up to evaluate interventions • Evaluate the cause and contributing factors of any pressure ulcer that develops References Braden, B., & Bergstrom, N. (1988). Braden Risk Assessment Scale. Gorecki, C., Brown, J., Nelson, E.A., Briggs, M., Schoonhoven, L., Dealey, C., … Nixon, J. (2009). Impact of pressure ulcers on quality of life in older patients: A systematic review, Journal of American Geriatrics Society, 57(7), 1175-183. Hopkins, A., Dealey, C., Bale, S., Defloor, T., & Worboys, F. (2006). Patient stories of living with a pressure ulcer, Journal of Advanced Nursing, 56(4), 345-353. METASTAR. Pressure Ulcer Bundle. Accessed at http://www.metastar.com/web/Default.aspx?tabid=339 NPUAP-EPUAP (2009). Pressure ulcer prevention & treatment: Clinical practice guideline. Spilsbury, K., Nelson, A., Cullum, N., Iglesias, C., Nixon, J. & Mason, S. (2007). Pressure ulcers and their treatment and effects on quality of life: Hospital inpatient perspectives. Journal of Advanced Nursing, 57(5), 494-504.