Alveolar macrophages (AMs)
advertisement
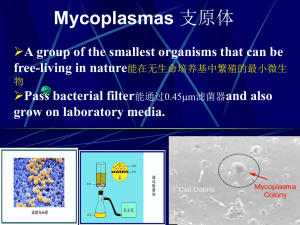
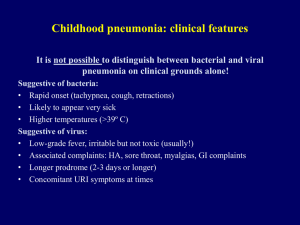
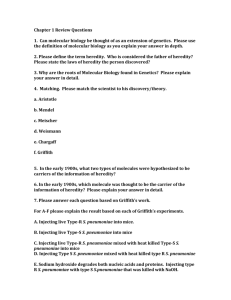
Pulmonary adaptive responses against bacterial pathogens J S Brown Reader in Respiratory Infection Centre for Respiratory Research Department of Medicine University College London Adult community acquired pneumonia: CAP • incidence: overall 0.25%? admissions 50/100,000 per year > 65 years • 50 - 80% mild - outpatient treatment • 50 - 20% admitted - 10 - 20% severe / ITU - mortality 5 – 10% (20% UK audit) - 65000 deaths per year in UK • who gets CAP? - elderly: but only 50% cases >65 years - smokers: attributable risk 51% - comorbidities: attributable risk 14% (lung /cirrhosis / renal disease / diabetes CNS disease) Causes of adult community acquired pneumonia [CAP] (Lim et al. Thorax 2001) UK hospitalised patients influenza other viruses 13% 4% Chlamydia pneumoniae Mycoplasma pneumoniae 3% Legionella 3% 48% 13% 20% Streptococcus pneumoniae 7% Haemophilus influenzae Unknown 20% no pathogen identified Staphylococcus aureus 1.5% Moraxella catarrhalis 2% Gram negative bacilli 1.4% Causes of CAP worldwide (JSBrown Respirology 2009) Streptococcus pneumoniae infections 2nd commonest bacterial cause of death nasopharyngeal commensal 10% adults 50% infants Septicaemia 1 in 25 aspiration mortality 20% otitis media meningitis mortality 0% mortality 20% pneumonia 0 to 75 per 100,000 colonisations Streptococcus pneumoniae infection epidemiology - suggests adaptive immunity to colonisation is important? - waning of adaptive immunity with age? Health Protection Agency, United Kingdom, 2008 Immune response to S. pneumoniae pneumonia Key immune effectors 1. NP colonisation 1. physical defences 2. Early lung infection 1. physical defences 3. Established pneumonia 4. Septicaemia 1. inflammatory exudate 1. Complement 2. RE system 2. mucosal proteins 2. mucosal proteins 3. lymphocytes 3. alveolar macrophages 4. phagocytes 2. phagocytes 3. Circulating phagocytes 3. CD4 and CD8 lymphocytes? Mechanisms of adaptive immunity IFN-gamma Th1 CD4 T-cell IL-22 Mucosal repair Th17 Hyper IgE syndrome Th2 B-cell IL-17 Antimicrobial peptides Antibody Antibody deficiencies Chemokine release Phagocyte recruitment Phagocyte CD8 T-cell Cytotoxicity v. TAP syndrome? intracellular pathogens Alveolar macrophages (AMs) • First-line phagocyte in lung • Large range of receptors for - direct interactions with bacteria - Indirect interactions Fc gamma Receptors Complement Receptors • Airway lining fluid opsonins: - surfactant Scavenger - complement Receptors - IgA and IgG Toll Like Receptors Mannose receptor / lectins Bacterial phagocytosis by AMs can be saturated + + 1 hour All bacteria killed 1 hour 1 hour EFFICIENT BACTERIAL CLEARANCE NO PNEUMONIA / BRONCHITIS • intact epithelium • efficient alveolar macrophages Do IgG and IgA improve S. pneumoniae opsonisation in airways?? • low inoculum • low virulence strain BACTERIAL FACTORS HOST FACTORS Antibody and alveolar macrophages: • significant levels in IgG, IgA and IgM in airway lining fluid • IgG predominant x5 that of IgA • efficacy of IgG at promoting alveolar macrophage activity: IgG effect Gordon et al. Infect Immun 2000 • efficacy of IgA / IgM not clear…… Antibody and prevention pneumonia: • 1er and 2er IgG deficiency recurrent lung infections • therefore IgG essential for preventing lung infection • role of IgA unclear - IgA deficiency 1 in 400, only a subset develop recurrent lung infections • deficiency IgM also only sometimes associated with recurrent lung infection Anti IgG, alveolar macrophages, and S. pneumoniae: mouse data • mice protected v pneumonia after vaccination with: - protein antigens - conjugated capsule antigen - unconjugated capsule antigen - dead or live whole cells Bacterial lung CFU inversely correlate with Ab level to Cps Ag • but few data on mechanism(s) Jakobsen Infect Immun 1999 S. pneumoniae capsular polysaccharide vaccines and protection against CAP: • 23 valent unconjugated Pneumovax - protects against septicaemia - no evidence protects against pneumonia • conjugated vaccine IgG response too weak (unconjugated)? - 7 to 13 valent Host response poor due to comorbidity / age? - protects childrentoo against pneumonia (25%:) Serotype coverage restricted to detect effects? directly?? Wrong antigens? - not used in adults yet - major issue serotype with coverage: Failure of clearance of initial S. pneumoniae infection neutrophilic consolidation IL17 dependent immunity Invading S. pneumoniae increased mucosal: - chemokine release - antimicrobial peptides - mucosal repair Neutrophil recruitment IL-17 IL-22 Primed Th17 CD4 cells Hyper IgE (Job’s) syndrome and pneumonia • triad of: raised IgE, abscesses, and pneumonia • infections with S. pneumoniae • mutations of STAT3, regulates cytokine responses • specifically causes a defect in CD4 Th17 response • demonstrates probable role for Th17 v. lung infection Milner Nature 2008 IL-17 dependent adaptive immunity and S. pneumoniae • required for immunity v. nasopharyngeal colonisation: - after colonisation (Zhang J Clin Inv 2009) - after vaccination with whole cell vaccine (Lu PLoS Pathogens) • mechanism: - neutrophil-dependent - increases neutrophil recruitment and efficacy • We don’t know whether protects against pneumonia…. • Antigen targets unknown…… (lipoprotein?) Target antigens for natural adaptive responses to S. pneumoniae • capsule target for vaccine adaptive responses serotype dependent incidence in children with increasing age • may not be for natural responses: - wide range protein antigens - acquired immunity seems independent of capsule serotype - anti-protein response to colonisation often dominant • protein antigens maybe crossprotective Lipsitch, Plos Medicine, 2005 Summary and conclusions re. lung adaptive immunity v. S.pneumoniae • Antibody via improved alveolar macrophage and neutrophil phagocytosis v. important • Th-17 mechanisms also could be helpful • Natural adaptive immune responses can be directed against protein antigens • Need to aim for vaccination strategy that: - boosts S. pneumoniae clearance from the lungs therefore alveolar macrophage efficacy key -can protect against wide-range of strains protein antigens need to be considered Acknowledgments • UCL Centre for Respiratory Research – – – – – – – Dr Jonathan Cohen Dr Suneeta Khandavilli Dr Catherine Hyams Dr Emilie Camberlein Dr Jose Yuste Dr Alejandro Ortiz Stern Steve Bottoms • UCL Institute of Child Health – – – – Dr Helen Baxendale Prof David Goldblatt Prof Nigel Klein Lindsey Ashton • UCL Dept Immunology – Dr Claudia Mauri – Dr Natalie Carter • Erasmus Medical Centre, Rotterdam • Intercell AG, Vienna – Prof Alex van Belkum – Dr Corné de Vogel • UCL Biological Services Unit – Dr Carmen Giefing – Dr Eszter Nagy