Parenteral empiric antibiotics for inpatient treatment
advertisement
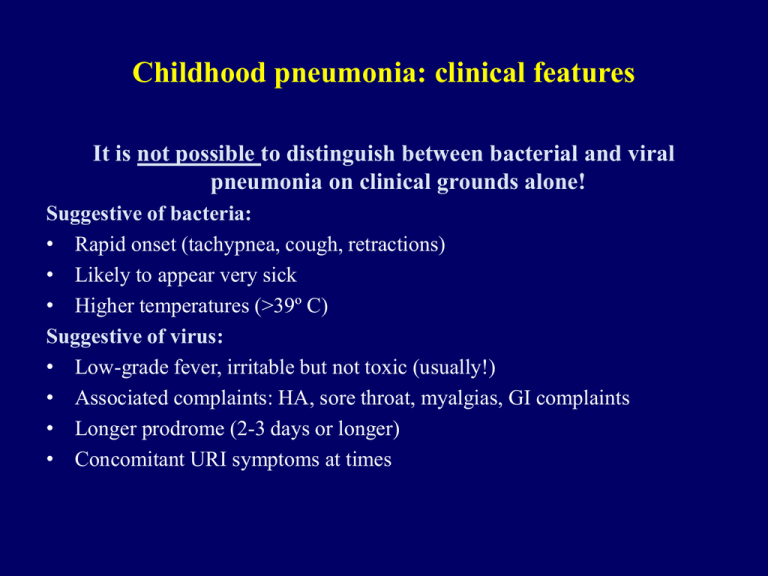
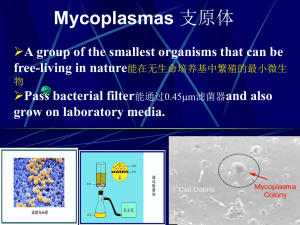
Childhood pneumonia: clinical features It is not possible to distinguish between bacterial and viral pneumonia on clinical grounds alone! Suggestive of bacteria: • Rapid onset (tachypnea, cough, retractions) • Likely to appear very sick • Higher temperatures (>39º C) Suggestive of virus: • Low-grade fever, irritable but not toxic (usually!) • Associated complaints: HA, sore throat, myalgias, GI complaints • Longer prodrome (2-3 days or longer) • Concomitant URI symptoms at times Indications for hospitalization in pediatric pneumonia • Considered for most infants <4 months of age (unless viral etiology/Chlamydia trachomatis and child relatievly asymptomatic) • Hypoxemia (oxygen saturation <92%) • Dehydration, poor oral intake • Moderate to severe respiratory distress: RR> 70 breaths/min in infanst <12 months or >50 breaths/min in older children, difficulty breathing, apnea, grunting • Toxic appearance (tends to be more common with bacterial etiologies) • Underlying conditions predisposing to a more serious course (cardiopulmonary disease, immunocompromised, metabolic disorders) • Presence of complications – effusions/empyema • Failure of outpatient therapy (worsening or no response in 24-72 hours) Indications for treatment in an intensive care unit in pediatric pneumonia • Failure to maintain O2 saturation >92% in FiO2 >0.5-0.6 • Signs of impending respiratory failure (lethargy, increasing work of breathing, and/or fatigue with or without hypercarbia) • Recurrent apneic episodes or slow, irregular respirations • Cardiovascular compromise with progressive tachycardia and/or hypotension Pediatric Community-acquired pneumonia: Etiologic agents Birth to 20 day • • • • • Group B streptococci Gram-negative enteric bacilli Cytomegalovirus Listeria monocytogenes Viruses 3 weeks to 3 months • • • • • • • Chlamydia trachomatis Respiratory syncytial virus Parainfluenza virus Streptococcus pneumoniae Bordetella pertussis Staphylococcus aureus Viruses (metapneumoivrus, adenovirus, influenza virus, rhinovirus, others) Pediatric Community-acquired pneumonia: Etiologic agents Prechool • Streptocccus pneumoniae • Viruses • Mycoplasma pneumoniae • Staphylococcus aureus (including MRSA) 5 to 15 years • Mycoplasma pneumoniae • Chlamydophila pneumoniae • Streptocccus pneumoniae • Viruses • Staphylococcus aureus (including MRSA) Remember to consider tuberculosis, endemic fungal disease (histoplamosis), aspiration pneumonitis, Pneumocystis jiroveci, pertussis, CMV, and other etiologic agents in certain age groups and in specific clinical settings! Childhood pneumonia: clinical features Suggestive of Mycoplasma pneumoniae • Older children • Multiple organ systems may also be involved • Rapid and progressive disease in sickle cell anemia Suggestive of Chlamydia trachomatis (in young infant): • Afebrile pneumonia with tachypnea and crackles • May be associated with conjunctivitis, FTT Diagnosis of pediatric pneumonia Bacteria - WBC count & leukocytosis ,blood cultures (3%-11% in pneumonia), CRP, ESR; “sputum “ (Gram stain and culture), urine pneumococcal antigen (good sensitivity, poor specificity) Viral - viral isolation, antigen detection, molecular diagnostics, serology limited. Mycoplasma – serology (IgM has poor specificity ~60%), paired serology, PCR (limited sensitivity in children; poor sputum sample) Chlamydophila – Serology (poor sensitivity , limited specificity in children), Legionella – Urinary antigen (sensitivity ~80%, specificity ~100%) Radiology – to follow. “… we have found that studies assessing the diagnostic accuracy of clinical, radiological, and laboratory tests for bacterial childhood pneumonia have used a heterogeneous group of gold standards, and found, at least in part because of this, the index tests have widely different accuracies. These findings highlight the need for identifying a widely accepted gold standard for diagnosis of bacterial pneumonia in children.” Lynch T, et al. A systematic review on the diagnosis of pediatric bacterial pneumonia: When gold is bronze. Plos ONE 2010; 5(8): e11989. doi:10.1371/journal.pone.0011989 Michelow IC, et al. Pediatrics 2004; 113:701-707 Michelow IC, et al. Pediatrics 2004; 113:701-707 Michelow IC, et al. Pediatrics 2004; 113:701-707 Michelow IC, et al. Pediatrics 2004; 113:701-707 Parenteral empiric antibiotics for inpatient treatment of pediatric pneumonia Remember: Most community-acquired pneumonia in children <5 years is caused by a virus! Age group Empiric regimen Birth to 3 weeks Bacteria – Group B streptococcus, gram-negative bacilli Ampicillin 200mg/kg/d + gentamicin 5 mg/kg/d and/or cefotaxime 150 mg/kg/d 3 weeks to 4 months Bacterial Chlamydia trachomatis Cefuroxime (100-150 mg/kg/d in three divided doses), or Ceftriaxone (50-75 mg/kg once daily), or Cefotaxime (150-200 mg/kg/d in three or four divided doses) Erythromycin (40 mg/kg/d in four divided doses), or Azithromycin (5 mg/kg once per day) Parenteral empiric antibiotics for inpatient treatment of pediatric pneumonia Age group Empiric regimen >4 months Bacterial (not Mycoplasma or Chlamydophila pneumoniae) Ampicillin 150-200 mg/kg/d div qid. or Cefuroxime (100-150 mg/kg/d in three divided doses [Max 4-6 g/d), or Ceftriaxone (50-75 mg/kg once daily [MAX 4 gm/d]), or Cefotaxime (150-200 mg/kg/d in three or four divided doses [MAX 8-10g/d]) Mycoplasma or C. pneumoniae Erythromycin (40 mg/kg/d in four divided doses [MAX 4g/d]), or Azithromycin (5 mg/kg once per day [MAX 500 mg/d]), or Doxycycline 4 mg/kg/d in two divided doses [MAX 200 mg/d]) – in children >8 years Treatment of severe community-acquired bacterial pneumonia Suspect MRSA in: “Patients with severe pneumonia, particularly during influenza season, in patients with cavitary infiltrates, and in those with a history of MRSA infection” Treatment: Vancomycin or linezolid should be used in such patients Med Lett Drugs Ther 2007; 49(1266):62-64 Empiric antibiotics for treatment of severe pneumonia Moderately severe (non-ICU) pneumonia: Erythromycin, or azithromycin, or doxycycline PLUS Ceftriaxone or cefotaxime Complicated pneumonia/abscess/effusion or severely ill patients requiring ICU admission: Ceftriaxone or cefotaxime PLUS Vancomycin (trough levels 15-20 ug/mL) or ? clindamycin PLUS Azithromycin PLUS (if necessary) Nafcillin Duration of therapy in pediatric pneumonia • Few evidence-based data to guide duration of therapy • Parenteral: Generally preferable to switch to oral antimicrobial therapy in patients who have received IV medications if (a) afebrile for 24-48 hours and (b) able to keep food down. • Uncomplicated cases: 7-10 days combined IV/PO for routine pathogens in uncomplicated infection. • Consider continuing PO therapy until one week beyond resolution of fever • Complicated cases: Necrotizing pneumonia or abscess – likely 4 weeks and patient improving. Su-Ting T, Tancredi D. Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine. Pediatrics 2010; 125:26-33. Byington CL, et al. J Clin Microbiol 2010; 48: 520-525 Parapneumonic effusion and empyema in children – organisms • Streptococcus pneumoniae – most common pathogen • Penicillin-susceptible • Penicillin non-susceptible • Pneumococcal-conjugate vaccine impact • Staphylococcus aureus • Methicillin-resistant (MRSA) • Methicillin-susceptible • Group A streptococcus (Streptococcus pyogenes ), others (in immunocompromised, neonates) • R/O non-infectious etiologies Critical laboratory evaluation: pleural fluid analysis, other microbial analyses, blood cultures, other testing dependent on clinical scenario Antibiotic therapy in therapy in complicated pediatric pneumoniaa, parapneumonic effusion and empyema Ceftriaxone (50 to 100 mg/kg once daily [MAX 4 g/day]) or cefotaxime (150 to 200 mg/kg per day in three to four divided doses [MAX 8 to 10 g/day]) PLUS Clindamycin (30 to 40 mg/kg per day in three or four divided doses [MAX 1 to 2 g/day]) OR, for patients very ill and suspect MRSA or allergic to clindamycin Vancomycin (60 mg/kg per day in four divided doses [MAX 2 to 4 g/day]) Might need to cover atypical pathogens in some cases. Modify antibiotic therapy based on culture/microbiologic results when available. a necrotizing process Effective Therapy for Serious Infections Caused by MRSA Vancomycin – Glycopeptide antibiotic – Inhibits bacterial cell wall synthesis by high-affinity binding to cell wall precursors. – Therapeutic blood level monitoring – VISA, VRSA – IV preparation only Linezolid – Oxazolidinone antibiotic – Interferes with formation of bacterial ribosomal initiation complex to prevent activation of protein synthesis. – Available in both intravenous and oral preparations – Expensive Vancomycin Clinical Failure Rates in MRSA Infections n = 63 patients with MRSA treated with vancomycin Moise-Broder et al. Clin Infect Dis 2004; 38:1700-05