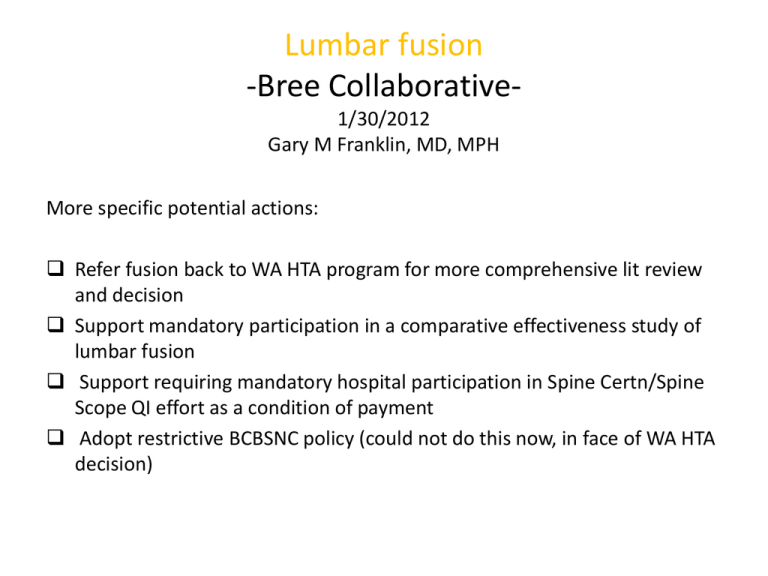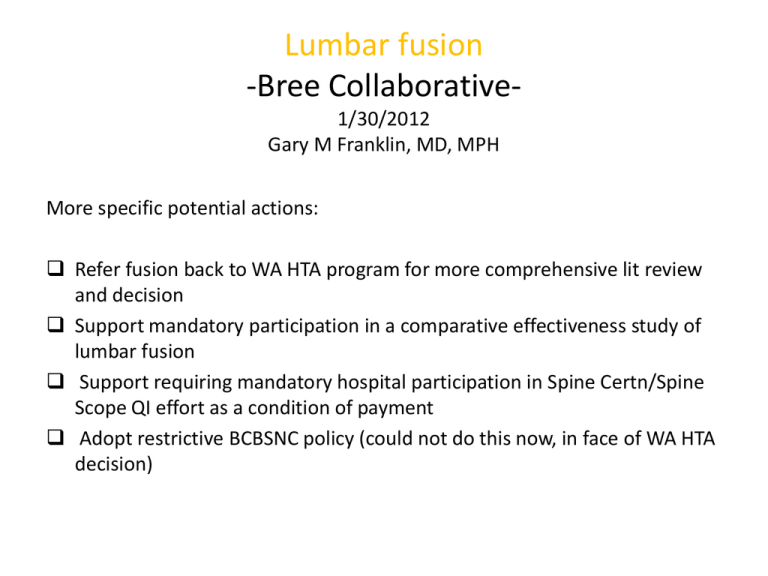
Lumbar fusion
-Bree Collaborative1/30/2012
Gary M Franklin, MD, MPH
More specific potential actions:
Refer fusion back to WA HTA program for more comprehensive lit review
and decision
Support mandatory participation in a comparative effectiveness study of
lumbar fusion
Support requiring mandatory hospital participation in Spine Certn/Spine
Scope QI effort as a condition of payment
Adopt restrictive BCBSNC policy (could not do this now, in face of WA HTA
decision)
Fusion Concerns
– Concern relates to subset of patients with chronic low back pain (LBP)
• Spinal fusion covered and not at issue for traumatic injuries, patients with significant instability,
congenital defects, neurological issues
• Fusion surgery outcomes, especially in workers comp. are poor
– This patient subset suffers substantial and chronic pain that can be disabling and interferes
with life function. There is no gold standard treatment that is curative. Some patients get
better with no treatment while others experience temporary or sustained pain reduction or
relief from:
•
•
•
•
Medication
Physical rehabilitation/care (exercise, rehabilitation, chiropractic, acupuncture)
Mental care (education, cognitive behavioral therapy)
Surgery followed by rehabilitation
– Surgical premise for fusion is that disc degeneration causes pain that can be
reduced/eliminated by immobilizing disc(s)
– Question whether the surgery is effective (any improvement, incremental improvement, or
full resolution)
• Is effect attributable as much to placebo or the rehabilitative component
– Question whether/ when the invasive procedure with attendant significant risk compared with
non-surgical alternatives is appropriate
• Re-operation and surgical complication rates are very high
• If appropriate, when or who in the LBP group benefit
DLI Fusion Guideline
-Last updated 2001• Mandatory prior authorization
• Approval for fusion only if a)measurable
instability present and/or b)objective evidence
of neurological impairment associated with
DDD/bony deformity and/or (since Dec 2009)
c) DDD and failed structured, intensive
multidisciplinary program (SIMP)
Rates of Four Orthopedic Procedures
Among Medicare Enrollees, 2002 and
2003
Standardized Discharge Ratio (Log scale)
3.0
1.0
0.3
Hip
Fracture
(14.3)
Source:
Health Care.
Source:Dartmouth
DartmouthAtlas
AtlasofProject.
Knee
Replacement
(53.6)
Hip
Replacement
(69.5)
Back
Surgery
(103.8)
What is the evidence that fusion improves
outcomes?
• Four randomized controlled clinical trials since
2001(highest level of evidence)
• Fritzell et al, 2001, Spine 26: 2521-32. Compared to
unstructured conservative Rx (PT), fusion paients
sign better on pain (but deteriorated after 6 months),
function (Oswestry, Million), and RTW; early
complications in 17%
• Kwon et al, 2006, Spine 31: 245-9. Critique of
methodology of Fritzell study
3 RCCTs with no evidence of efficacy
• Brox et al, 2003; Spine 28: 1913-21.
Fusion (and PT) vs structured rehab (education,
exercize sessions);pain, function (Oswestry) no
different at 1 yr; early surgical complictions 18%
• Fairbank et al, 2005; BMJ 330: 1233-40.
Fusion vs intensive cognitive rehab; Oswestry
marginally better at 2 years but walking test and SF36 no better; 17% with complications or more
surgery
3 RCCTs with no evidence of efficacy
• Brox et al, 2006; Pain 122: 145-155.
Fusion vs structured rehab(education,
exercize); Oswestry no better at 1 yr
WA HTA decisions
• 2/15/2008-Fusion for DDD covered if
structured, intensive, multidisciplinary
program (SIMP) not available, or if SIMP fails
• 8/15/2008-discography for DDD not covered
Blue Cross/Blue Shield North Carolina
1/20/11
• When lumbar spine fusion surgery is not covered
– Meets an included condition (eg, fracture, stenosis
with neuro compromise)
– Not medically necessary if sole condition is any one or
more of the following:
• Disc herniation
• Degenerative disc disease
• Initial diskectomy/laminectomy for neural structure
decompression
• Facet syndrome
Compensation status relates to poor
outcomes from most procedures
• Harris I, et al. Association between
compensation status and outcome after
surgery: A meta-analysis. JAMA 2005; 293:
1644-52.
• Lumbar fusion: 19 studies; odds ratio of worse
outcome for fusion among compensation
patients: 4.33 (95% CI: 2.81-6.62)
Recent DLI case
•
Initial injury 7/5/99- L3, L4, L5 laminectomy/foraminotomy; RTW as trucker;
Cat 3 PPD
• Injury 1/7/01
– 9/25/01- L5-S1 anterior lumbar interbody fusion with BAK cages
– 11/2/01-fusion revision requested
– 8/13/03- laminectomy redo L4,5,S1; L5-S1 instrumented fusion based on ?
Pseudoarthrosis
– CAT 4 PPD (fusions + S1 radiculopathy)
– 12/16/03-RTW trucking
Injury 6/28/08
6/24/09- Removal L5-S1 hardware; exploration, decompression L4-S1
10/12/11-L4,L5 laminectomy, Pedicle screw, transforaminal interbody
fusion L4-5; intertransverse fusion L4-5 (Paid by another party since
denied by Dept)
Washington State WC Outcomes
• Franklin et al, 1994; Spine 20: 1897-903
N= 388 from 1986-87
68% TTD at 2 years; 23% more surgery by 2 yrs
Instrumentation doubled risk of reoperation
Surgical experience didn’t matter
Key-WC fusion outcomes far worse than previously
reported from surgical case series
1992-DLI Lumbar fusion guideline
• No prior surgery
-measurable instability on flexion/extension
xrays
-Spondylolisthesis with measurable
instability OR neurologic signs/symptoms
-only single level fusion
Lumbar Fusion Policy Translation
1992: tightened lumbar fusion guideline to include measurable
instability; exclude pure “discogenic” back pain; exclude cases
of acute disc herniation
Adapted from Elam et
al. Medical Care
1997;35:417-424
Lumbar Fusion-Effect of Rapid Diffusion
of New Technology
Adapted from Franklin et al. Am J Man Care 1998;4:SP178-SP186
Washington State WC Outcomes
Juratli et al, 2006; Spine 31:2715–23.
1950 fusion subjects from 1994-2000
85% received cages and/or instrumentation
64% disabled at 2 yrs; 22% reoperated by 2 yrs + 12%
other complications
Cage/instrumentation use increased complications
without improving disability or reoperation rate
Juratli et al, Mortality (WC)after Lumbar Fusion
Surgery, Spine 2009; 34: 740-47
• N=2378 fusions between 1994-2001
• Death records-103 deceased by 1994
• 90 day perioperative mortality 0.29%-assoc with
repeat fusion
• Age and gender adjusted all cause mortality 3.1
deaths/1000 worker yrs
• Opioid-related deaths 21% of deaths and 31.4% of
potential life lost
• Risk > with instrumentation/cages and DDD
Percent
3 month reoperation rates across hospitals
in California (Black) and Washington (Red)
15%
10%
5%
0%
0
100
200
300
Volume of WC fusion performed by hospital
Source: SID CA & WA, 2008-2009
Adjusted for age, sex, comorbidity, and diagnosis
Horizontal black line represents overall mean
Martin BI et al, in preparation, 2012
400
Most recent DLI paid fusion #’s
2000-406
2001-418
2002-447
2003-418
2004-412
2005-366
2006-381
2007-341
2008-345
implemented
2009-412 WA HTA decision
12/2009
2010-410
2011-369
(incomplete)
Why Spine SCOAP?
Martin BI, Mirza SK, Flum DR, Wickizer TM, Heagerty PJ, Lenkoski AF, Deyo RA.
Repeat surgery after lumbar decompression for herniated disc: the quality
implications of hospital and surgeon variation. Spine J. 2011 Dec 20.
Spine SCOAP Development
2011 Milestones
• Pilot mode July 1, 2011
• 5-10% sample from 9 hospitals
• 1000 cases for 2011
2012 Plan
• 3000 cases, 80% fusion/20% all other case types
•
LSDF funding and Industry gifts to FHCQ
• 18 hospitals (80% of eligible spine procedures)
Unique Features
• Patient-reported outcomes at baseline through 4 years (funded)
• Focus on fusions
• Hosts a multi-stakeholder spine forum-advisory board
How Spine SCOAP and CER Decrease
Variation
• QI activity shines light on variability in indications
and outcomes across centers/surgeons
– Quarter by quarter improvements starting in 6 months
– Works through “outlier” effect
• CER study shows definitively what works and
what doesn’t
• Both help inform HTA decisions and payment
policy
• Bree collaborative could help by making QI or
CER activity a “community standard”
What direction shall we go?
Refer fusion back to WA HTA program for more comprehensive lit review
and decision
Support mandatory participation in a comparative effectiveness study of
lumbar fusion
Support requiring mandatory hospital participation in Spine Certn/Spine
Scope QI effort as a condition of payment
Adopt restrictive BCBSNC policy (could not do this now, in face of WA HTA
decision)
Highest priority
Second priority
Your input
THANK YOU!
For electronic copies of this
presentation, please e-mail Melinda
Fujiwara
vasudha@u.washington.edu
For questions or feedback, please
e-mail Gary Franklin
meddir@u.washington.edu