Topic 2
advertisement

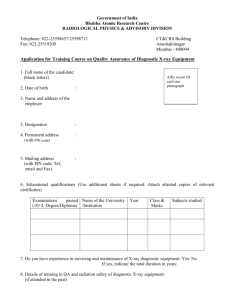
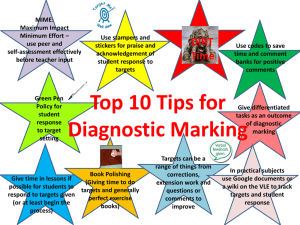
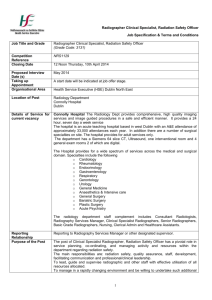
Quality assurance and Quality control in medical radiography Topic 2 • Departmental standards for radiographic image quality • QA/QC group establishment • Quality Management Objectives Diagnostic procedure chain “Quality assurance as applied to medical radiography is the organized effort of the staff to ensure that the diagnostic images produced are of high quality. Its purpose is to provide adequate diagnostic information with the least possible cost and the least possible radiation exposure to the patient and staff” “Quality assurance as applied to medical radiography is the organized effort of the staff to ensure that the diagnostic images produced are of high quality. Its purpose is to provide adequate diagnostic information with the least possible cost and the least possible radiation exposure to the patient and staff” “Quality assurance as applied to medical radiography is the organized effort of the staff to ensure that the diagnostic images produced are of high quality. Its purpose is to provide adequate diagnostic information with the least possible cost and the least possible radiation exposure to the patient and staff” “Quality assurance as applied to medical radiography is the organized effort of the staff to ensure that the diagnostic images produced are of high quality. Its purpose is to provide adequate diagnostic information with the least possible cost and the least possible radiation exposure to the patient and staff” “Quality assurance as applied to medical radiography is the organized effort of the staff to ensure that the diagnostic images produced are of high quality. Its purpose is to provide adequate diagnostic information with the least possible cost and the least possible radiation exposure to the patient and staff” • It requires the combined efforts of the whole radiology staff. • A hospital qa/qc committee and a qa/qc team must be created to institutionalize the program. Requirements of a QA/QC program i. Hospital chief radiologist- head of the x-ray section/department ii. Chief x-ray/radiologic technologist iii. Hospital physicist iv. Other radiologists and radiology resident physicians v. Other x-ray/radiologic technologist Hospital QA/QC team i. Chief of hospital ii. Administrative officer iii. Chief radiologist iv. Chief x-ray/radiologic technologist v. Chief physicist vi. Hospital maintenance engineer/technician vii. Others Hospital QA/QC committee Responsibilities of these groups are as follows: I. Do periodic film analysis and monthly film analysis report to the QA/QC committee II. Establish additional radiographic technique charts when needed, or revise existing technique charts when appropriate. III. Establish additional darkroom processing charts or revise existing ones when necessary Hospital QA/QC team IV. Do periodic quality control test of x-ray equipment, accessories, and darkroom equipment and accessories V. Keep a room logbook which contains all the test data on equipment, accessories and all the changes/repairs done to all equipment/accessories in the room, sample images, procedures for QC tests, etc. VI. Keep all brochures and technical manuals pertaining to equipment and accessories. I. Meet regularly to discuss film analysis report, QC test results, other reports and problems of the x-ray department/section. II. Decide on corrective action to be implemented and on other matters related to the program III. Keep a record of minutes of meetings. Hospital QA/QC committee In planning and establishing a QA/QC program the following should be considered In medical radiography A. Commitment and support of radiology personnel to sustain the program B. Establishment of standards of image quality C. Conduct of film analysis every month D. Establishment of standard darkroom techniques and conduct darkroom QC checks E. Conduct of preventive maintenance and quality control checks F. Establishment of standard protocols in performing different examination G.Establishment of a radiation safety program H. Conduct of continuous education and training The purpose of A QC testing program • Is to maintain the quality of diagnostic images. • This is done with routine monitoring of photographic and x-ray equipment parameters to detect deviations of equipment performance and take prompt corrective action. The purpose of a QC testing program • QC test equipment • Equipment acceptance testing • QC testing program • X-ray equipment QC • Photographic equipment QC QC test • A program of QA monitors proper patient scheduling, reception, and preparation and answers the following questions; • Is the scheduled examination appropriate for the patient? • If so, has the patient been properly instructed before the time of the examination? Quality assurance deals with people • Equipment performance records and record keeping • Equipment appraisal and replacement policy • Standardization of exposure • Acceptance criteria for diagnostic radiograms • Reject-repeat analysis program QA test • Refer to TJC 10 step quality assurance program • Quality control deals with instrumentation and equipment. QA also involves image interpretation or outcome analysis. Quality control is more tangible and obvious because in this program the radiologist is provided with optimal image produced through good equipment performance and resulting in minimal patient radiation exposure. Quality management program • It should consist of at least the FF. Components: • • • • Equipment quality control Administrative responsibilities Risk management Radiation safety program Components for quality management program • It involves evaluation of equipment performance to ensure proper image quality, as well as patient and operator safety. Equipment quality control • It involves the establishment of various processes to accomplish the specific departmental task. • • • • • • Procedure manuals Data collections Scheduling and routing of patients Education of personnel Equipment acquisition Communication with other department Administrative responsibilities • It is the ability to identify potential risk to patients, employees and visitors at the healthcare institution. • Nosocomial infections Risk management • It is to ensure patient exposure is kept as low as reasonably achievable (ALARA), medical staff, dept. Personnel, and member of the general public are protected from overexposure to ionizing radiation. Radiation safety program • Personnel protection • Time • Distance • Shielding Other Quality Management/ Quality Improvement Models • FADE • 5 STAGE PLAN • SWOT analysis • FOCUS-PDCA • FMEA End