Mobile Radiography
advertisement

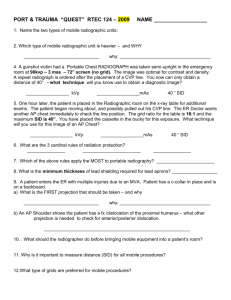
Mobile Radiography (Portables) 8/29/2012 Class ed. Principles of Mobile Radiography You bring imaging services to pt using transportable x-ray equipment Where are they commonly used? pt room ER ICU surgery and recovery rooms nursery and neonatal units When was mobile x-ray equipment first used? battlefield WW1 -units were carried to field sites Mobile X-Ray Machines • True or false? Portables are as sophisticated as stationary units? – False • Typical unit has what 2 controls? – kVp and mAs • What is the mAs range? – Generally 0.04 to 320 mAs What is the kVp range? -generally 40 to 130 kVp Two basic types of Mobile X-Ray Machines 1. Battery powered • Uses two different sets of batteries (lead-acid, or nickel-cadmium ) – One powers driving of machine – One set provides power to x-ray tube • Fully charged batteries: - can make 10 to 15 exposures - be driven reasonable distances 2. Capacitor discharge (obsolete) • No batteries • Carries two metal plates that hold electrical charge • Capacitor units must be charged prior to each use Battery-operated Unit Advantages: – Cordless – Provide constant kVp and mAs Disadvantages: - Heavy - hard to control What is “Deadman” type of brake? – stops machine instantly when push-handle released Capacitor Discharge Units Advantages? lightweight, smaller and easier to maneuver require much less time to charge than battery units Disadvantages? can’t handle thick body parts due to voltage drop during exposure must be charged prior to each use The Nomad For places with no electricity or chemical processors Mainly for dental x-rays 3 important technical factors that must be clearly understood to perform optimum mobile examinations: Grid Anode-heel effect Source–to–image receptor (SID) Grid Must be level! X-ray beam must be properly centered to grid Correct focal distance must be used (Best grids for mobile radiography have ratios of 6:1 or 8:1 and a focal range of 36 - 44 inches) Make sure grid is fastened to cassette properly (tape) Anode Heel Effect • Correctly place anode-cathode (marked on tube housing) with respect to anatomy – • Anode should be on thinner part (T-spine) Heel effect increases with short SID, larger field sizes (more common in mobile radiography) Beam travels through thicker part of target on anode side, thus attenuating beam more SID- Mobile Units What is standard SID? 40 Possible problems with greater SID? Need increased mAs, thus longer exposure time Increases risk of imaging motion Increased drain on battery Possible grid cut-off Performing Mobile Examinations Plan ahead! Gather all necessary devices to take with you IR (bring extras!) Grid Tape Markers Sponges Before Beginning Examination • Find pt’s x-ray order • Let nurse’s station know of your presence and purpose • Identify pt and introduce yourself with your title • Explain exam and ensure it is appropriate and correct • Politely ask any visitors to leave • Obtain assistance when necessary! Interfering Devices • Watch out for orthopedic beds, fracture frames, tubes, wiring, etc., producing artifacts • Know which objects can be moved and which ones you have to work around • May have to perform with object in image • Ask if unsure whether an object can be moved Portable Position • If exam in supine position, move base of machine to middle of bed • If seated upright, base at end of bed • Lateral and decubitus positions, place base parallel or perpendicular to bed Performing Mobile Examinations Make sure collimation is not open larger than IR size Check CR and IR alignment to prevent distortion Use consistent system for keeping exposed and unexposed IRs separate Keep log of procedures, time of examination, technical factors for image ID Technique Charts and Logs Exposure for optimum exam! Should be available for every machine Should display standard technical factors for all projections performed with machine Logbook of all recent pt exams and technique Caliper should also be available for accurate patient measurement Scatter Radiation and Mobile Radiography Mobile radiography produces some of highest occupational radiation exposure for radiographers! Wear a lead apron! Wear film badge at collar or waist outside lead protection What is single most effective radiation protection measure? Distance! What is minimal safe distance ? 6 feet Safest Place to Stand Least exposure is at what angle to pt and primary beam? Right angle When should you shield pt’s gonads? – X-raying children - Person is of reproductive age – Pt requests – Gonads lie in or near useful beam – When shield will not interfere with anatomy of interest Radiation Safety cont’d What is minimum source-to-skin distance? – 12 Have visitors leave area Warn other personnel when you are about to make an exposure Patient Mobility Never move pt or part without: Assessing ability to move or ability to tolerate movement Checking with staff obtain assistance and permission to move a part that has had surgery or fractured Inappropriate movement can further injure pt! Warn pt of potential discomfort from IR Cold Hard IR can damage skin of older patient Use cloth or paper cover to reduce risk of injury Protect IR from contamination by use of appropriate impermeable cover Assess Patient Condition Be aware of any limitations to procedure! • • • • • • • Alertness Respiration Ability to cooperate Language comprehension Mobility Fractures Interfering devices If in OR, don’t break sterile field! Isolation Considerations What are two types of pts in isolation? Those who have contagious infectious microorganisms you want to avoid them! Those who must be protected from exposure to infectious microorganismsthey want to avoid you! This known as? Reverse isolation! Isolation Considerations cont’d • Wear all required protective apparel for specific situation • Wash hands before gloving • Protect IR with protective cover Isolation Considerations cont’d After procedure: Discard of protective apparel according to protocol Wash hands! Wear clean gloves to clean equipment and use appropriate aseptic technique Wash hands again after removing gloves Most Common Portable Radiographic Exams • • • • • • Chest Abdomen Pelvis Femur Cervical spine Neonate AP Chest • Elevate head of the bed as pt condition permits • Pull pt to head of bed before elevating if condition permits • Make sure pt is not rotated What if pt has respiration assistance? • watch pt chest to determine inspiratory phase (or respirator) AP or PA Chest Lateral Decubitus Position • Place firm support under pt to elevate body and keep pt from sinking down in bed • Protect pt from rolling off of bed! Lateral Decubitus Position Considerations • Fluid levels best imaged with? – affected side down • Air levels seen best with? – affected side up • How long should pts be in this position before exposure? – 5 minutes • Why? – to allow fluid or air to settle Orthopedic Examinations How many images required? at least 2 films at right angles to each other Who do you obtain permission from prior to moving an injured pt? pt’s nurse or physician How do you position pts? very carefully! Lateral Cervical Spine – Dorsal decubitus position – CR horizontal – If there is a immobilization device when should you remove it? • NEVER or until Dr. gives permission Neonate • Move arms out of anatomy of interest • Bring legs down • Who should hold infant in position? • Nurse- (provide lead apron) • Why do you leave head rotated? – to avoid advancing endotracheal tube too far • Collimate closely • Shield gonads Neonate • AP projection of chest and abdomen often ordered and shot in one exposure • Infant is supine • Some bassinets equipped with tray to hold IR • If IR placed directly under infant- wrap with soft cover